Translate this page into:
Dermoscopy of dermatofibrosarcoma protuberans in skin of colour: A study of four cases
Corresponding author: Dr. Keshavamurthy Vinay, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. vinay.keshavmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mustari A, Chauhan P, Chatterjee D, Vinay K. Dermoscopy of dermatofibrosarcoma protuberans in skin of colour: A study of four cases. Indian J Dermatol Venereol Leprol. 2024;90:801-3. doi: 10.25259/IJDVL_325_2023
Dear Editor,
Dermatofibrosarcoma protuberans (DFSP) is a rare, locally aggressive, soft tissue sarcoma associated with poor prognosis.1 Dermoscopy is a non-invasive diagnostic tool that may increase its diagnostic accuracy. Current literature is scarce regarding the dermoscopic features of DFSP in skin of colour. We retrospectively reviewed the clinical, dermoscopy and histopathological features of four patients with DFSP with skin phototypes IV–VI. Dermoscopy images were taken using DermLite™ DL4 (3Gen, San Juan Capistrano, CA, USA) at ×10 magnification in polarised mode.
Two male (aged 36 and 47 years) and two female (aged 25 and 40 years) patients with primary DFSP were included. There was no history of preceding trauma in any of the patients. All had unifocal involvement and the sites involved were arm (patient 1), leg (patient 2), supraclavicular area (patient 3) and pre-sternal area (patient 4) measuring (longest diameter) 4 cm, 7 cm, 6 cm and 2.5 cm, respectively. Morphologically, the lesions were erythematous indurated nodulo-plaques with lobulated surface, irregular borders, central depression and telangiectasia (arm), [Figures 1a and b]; multiple erythematous protruding nodules in the background of atrophic scarring (leg), [Figure 2]; indurated oval plaque with lobulated surface with overlying papules and telangiectasia (supraclavicular area), [Figure 3]; and erythematous oval depressed plaque with smooth shiny surface and ill-defined borders (pre-sternal area), [Figure 4].
Histopathological examination revealed dermal tumour consisting of CD34+ monomorphic spindle-shaped cells in storiform pattern with nucleus showing moderate pleomorphic vesicular chromatin and blunt ends. These cells were merging into the collagenous stroma. A histopathological diagnosis conformed to classical DFSP in patients 1, 2 and 3 [Figure 5a] and atrophic DFSP in patient 4 [Figure 5b].
Dermoscopy showed pigment network and pink background in all patients (4/4; 100%). White streaks over pink background and white structureless areas were seen in three patients (3/4; 75%; [Figures 1a and 2]. Linear and arborizing telangiectasia (focused and unfocused) [Figures 1a and 2], grouped erythematous dome-shaped papillary excrescence at the borders [Figure 1b] and light-brown structureless areas were seen in two patients (2/4; 50%). Short fine telangiectasia and yellow structureless areas [Figure 3] and yellow globules [Figure 4] were seen in one patient each (1/4; 25%; [Table 1]).
DFSP, dermatofibrosarcoma protuberans; Y- Yes; N- No; M- Male; F- Female.
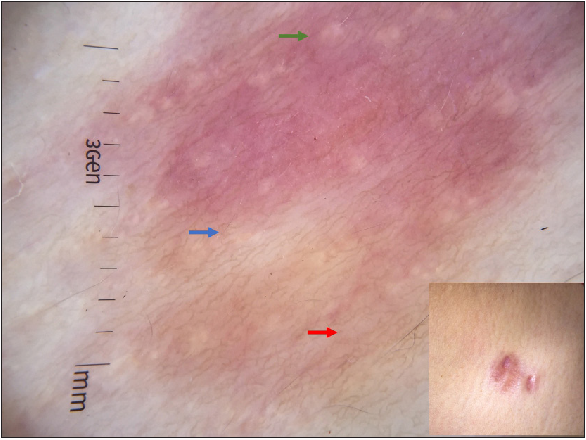
Linear and arborizing telangiectasia (red arrow) over pink background with white streaks (green arrow) and white structureless areas (blue arrow). Inset: Clinical presentation of DFSP over arm.
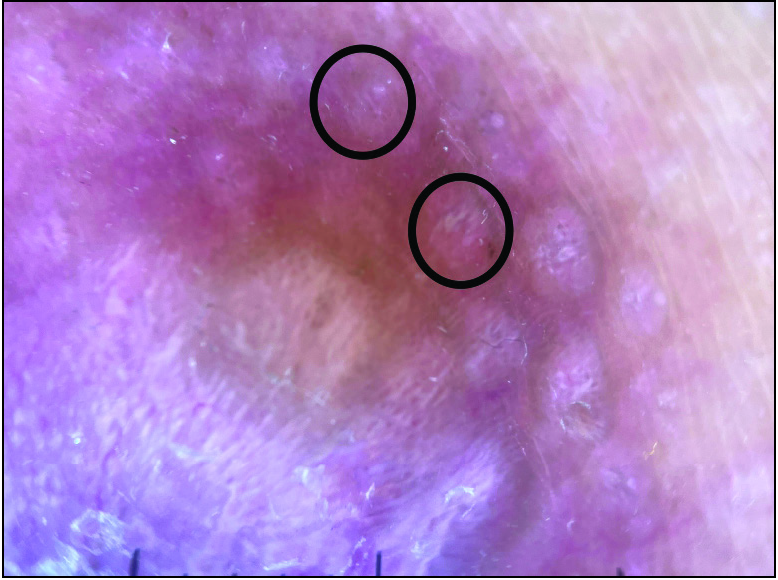
Dermoscopic presentation. Grouped erythematous doom-shaped papillary excrescence at the borders (black circles).

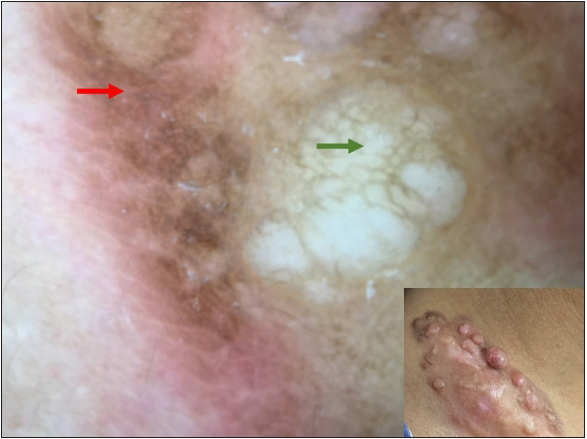
Linear and arborizing telangiectasia (red arrow), pigment network (green arrow) and white structureless areas (blue arrow). Inset: Clinical presentation of DFSP over leg.
Pigment network (red arrow) and yellowish structureless areas (green arrow). Inset: Clinical presentation of DFSP over supraclavicular area.
Dermoscopy of atrophic DFSP; yellow globules (green arrow) and yellowish structureless area (blue arrow) over pink background with prominent pigment network (red arrow). Inset: Clinical presentation of DFSP over pre-sternal area.
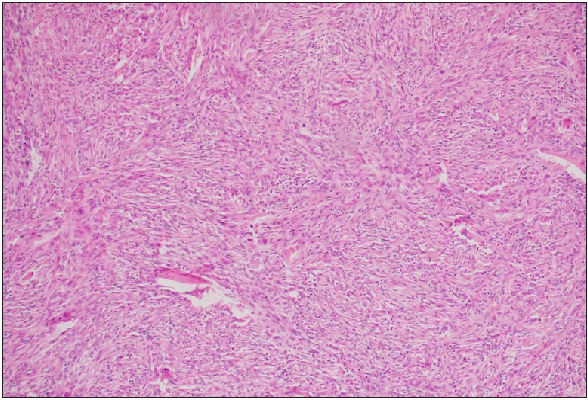
Dermal tumour cells of DFSP arranged in storiform pattern (Haematoxylin and eosin, ×400).
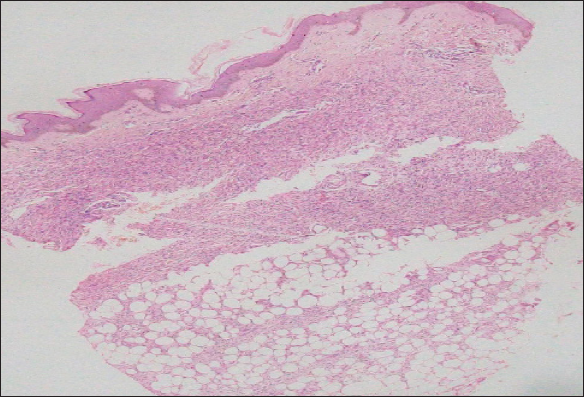
Atrophic DFSP; showing focal Focal epidermal atrophy and dermal tumour cells extending to subcutaneous tissue (Haematoxylin and eosin, ×100).
Age in years/sex
Site
Pigment network
Erythematous background
White streaks
Structureless white areas
Short fine telangiectasia
Arborizing vessels
Structureless light-brown areas
Structureless yellowish areas
47/M
Arm
Y
Y
Y
Y
N
Y
Y
N
40/F
Leg
Y
Y
Y
Y
N
Y
N
N
36/M
Supraclavicular area
Y
Y
Y
Y
Y
N
Y
Y
25/F
Pre-sternal area
Y
Y
N
N
N
N
N
Y
DFSP is a locally invasive, slow-growing intermediate malignant tumour with fibroblastic differentiation. It is commonly seen in the third to fourth decade in males over the upper trunk and proximal extremities. It starts as an asymptomatic indurated plaque and gradually progresses over several years to form large protuberant coalescing reddish-blue nodules with an atrophic telangiectatic surface.1 However, in skin of colour, DFSP is often misdiagnosed as keloid, dermatofibroma, leiomyoma, cutaneous B-cell lymphomas (CBCLs), deep fungal infections and desmoplastic melanoma.
The most common dermoscopic feature seen in our case series was pigment network and pink background, consistent with Bernard et al.2 The prominent pigment network may be explained by variation in the skin phenotype. In contrast, arborizing vessels were seen in two patients and short fine telangiectasia was seen in one patient each. The white streaky areas and white structureless areas represent increased collagen deposition and fibrosis respectively.2 Arborizing telangiectasia on diffuse yellow background has been described in atrophic DFSP.3,4 This feature was seen in one of our patients with atrophic DFSP as well. The vascular patterns seen were focused arborizing vessels and short fine telangiectasia. The yellowish structureless globules in atrophic DFSP is due to superficially placed adipose tissue. The novel finding of grouped erythematous papules at the border of the lesion in two of our patients needs further evaluation.
In contrast to DFSP, dermatofibroma shows a central white scar with delicate pigment network. Vascular structures can be seen in dermatofibroma but has varied morphology; dotted, coma and glomeruloid vessels.5 Leiomyoma shows dermatofibroma-like pigment network, white cloud-like areas and pinkish-brown thin lines.6 Even though arborizing and linear vessels are seen in keloids,7 the combination of pigment network, arborizing and linear vessels or short fine telangiectasia and white streaky areas and white structureless areas could be potential criteria for diagnosing DFSP. CBCL show prominent serpentine (linear-irregular) blood vessels on salmon-coloured background.8 Deep fungal infections can be differentiated by the presence of central crusting along with yellowish-orange structureless areas and polymorphous vessels.9 Atypical pigment network, atypical globules, atypical vascular patterns and crystalline structures are clues towards desmoplastic melanoma.10
To conclude, dermoscopy complements clinical diagnosis, helps in early suspicion of DFSP, increases diagnostic accuracy and helps in better patient management. It also helps in ruling out clinical mimickers such as leiomyoma, keloids, dermatofibroma, deep fungal infections, CBCL and desmoplastic melanoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Dermatofibrosarcoma protuberans: A review of the literature. Dermatol Surg.. 2012;38:537-51.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of dermatofibrosarcoma protuberans: A study of 15 cases. Br J Dermatol.. 2013;169:85-90.
- [CrossRef] [PubMed] [Google Scholar]
- Atrophic dermatofibrosarcoma protuberans: are there specific dermatoscopic features? J Dtsch Dermatol Ges. 2014;12:425-427.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of dermatofibromas: a prospective morphological study of 412 cases. Arch Dermatol. 2008;144:75-83.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy as an adjuvant tool for detecting skin leiomyomas in patient with uterine fibroids and cerebral cavernomas. BMC Dermatol. 2014;14:7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Keloids and hypertrophic scars: characteristic vascular structures visualized by using dermoscopy. Ann Dermatol. 2014;26:603-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy and the diagnosis of primary cutaneous B-cell lymphoma. J EurAcad Dermatol Venereol. 2018;32:53-6.
- [Google Scholar]
- Dermoscopy of bacterial, viral and fungal skin infections: A systematic review of the literature. Dermatol Ther (Heidelb). 2023;13:51-76.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical and dermoscopic characteristics of desmoplastic melanomas. JAMA Dermatol. 2013;149:413-21.
- [CrossRef] [PubMed] [Google Scholar]





