Translate this page into:
Dermoscopy of lichen planus pigmentosus in Indian patients – Pitfalls to avoid
2 Institute of Dermatology, University Hospital “Santa Maria Della Misericordia”, Udine, Italy
3 Department of Dermatology, College of Medicine, King Faisal University, Hofuf, Saudi Arabia
4 Department of Skin and V. D., Patna Medical College and Hospital, Patna, Bihar, India
5 First Department of Dermatology, Aristotle University, Thessaloniki, Greece
Correspondence Address:
Sidharth Sonthalia
Skinnocence: The Skin Clinic, C-2246, Sushant Lok-1, Block-C, Gurgaon - 122 009, Haryana
India
| How to cite this article: Sonthalia S, Errichetti E, Kaliyadan F, Jha AK, Lallas A. Dermoscopy of lichen planus pigmentosus in Indian patients – Pitfalls to avoid. Indian J Dermatol Venereol Leprol 2018;84:311-313 |
Sir,
We read with interest the cross-sectional observational study by Sharma et al., involving fifty Indian patients with suspected facial lichen planus pigmentosus evaluated for correlation between the clinico-dermoscopic, histopathological and patch test results, which was published in a recent issue of this journal.[1] Despite the well-founded intent behind the conduct of this study, we wish to highlight some significant issues pertaining to the technique and interpretation of the dermoscopic features mentioned, and add a few comments based on our limited but arduous work in this field.
- While describing dermoscopic features, it is imperative to mention whether the images were captured in a polarized or nonpolarized mode, along with the magnification. The differences in the optics and the consequent histological depth of evaluation by polarized and nonpolarized dermoscopes have been well established. Authors have mentioned that they employed the HEINE Delta mini® dermoscope, a relatively older nonpolarized device. Although they have not mentioned if an immersion fluid was used, the dermoscopic images are apparently suggestive of nonpolarized contact immersion dermoscopy. Moreover, if indeed employed, the authors should specify the composition of the immersion fluid. Nevertheless, the dermoscopic images published in this manuscript are essentially nonpolarized.[1]
- Although polarized dermoscopes have for long become cliched, it is important to know the essential basics of dermoscopy optics to understand the issues highlighted in this letter more easily. Broadly, dermoscopy can be divided into nonpolarized and polarized dermoscopy. Unlike nonpolarized dermoscopy, polarized dermoscopy significantly reduces the visualization of surface-reflected light and allows visualization of deep skin structures obviating the necessity of a liquid interface or direct skin contact with the dermoscope.[2] Although the employment of a liquid interface and direct contact between the scope and the skin enhances the depth of visualization in nonpolarized dermoscopy, contact nonpolarized dermoscopy with immersion fluid can still not attain the dermal depth of polarized dermoscopy. Thus, in the era of easy availability of dermoscopes of different makes, and the fact that majority of the diagnostic and histologically quantifying alterations in lichen planus pigmentosus are localized to the dermis, this study should have employed a dermoscope with polarizing mode. Notwithstanding the advantages of nonpolarizing dermoscopy over polarizing dermoscopy in certain circumstances, the esteemed authors should have used either polarizing mode alone or both the modes for documentation of reliable dermoscopic features.
- Dermoscopy is a constantly evolving technology that mandates updating the principles of technique and interpretation of features. Despite a 15-year-old singular observation that suggested colors appear sharper on conventional dermoscopy compared with polarized dermoscopy, conclusions from many recent studies devoted to this aspect are in agreement about polarized dermoscopy allowing better visualization of melanin with better color contrast.[3],[4] In our collective experience, the color and hue of the same pigmentary structure look appreciably different under polarized dermoscopy and nonpolarized dermoscopy. Benvenuto-Andrade et al. indeed reported that compared to nonpolarized dermoscopy (contact immersion), polarized dermoscopy renders different shades of brown and blue for melanin distributed in the skin, and imparts a little darker hue to the brown and blue colors.[3] Although this difference may not affect the interpretative dermoscopic pattern of lesions such as skin tumors, it is highly likely to have a bearing over the visualization and description of dermoscopic features of a primary non-nevus pigmentary disorder with deep histological alterations such as the lichen planus pigmentosus in which pigmentary structures are the main dermoscopic clues. It is noteworthy that red areas (secondary to vascular changes) are also better appreciated under polarized dermoscopy.[3],[4]
- The validity of the study would have increased if specific area(s) of the face were chosen in all patients for dermoscopy and histopathology to eliminate the element of topographical differences in different facial regions stemming from the content of appendages dictating the background pigment pattern. In the absence of an image bank of dermoscopic images of the “normal” skin in different areas, the employment of this approach attains huge significance. The recent study by Vinay et al. exemplifies this model approach in which dermoscopic evaluation was performed for four uniform predefined sites of the face in the study population.[5]
- Authors have described all dots and globules as “brown” only. The colors, despite being difficult to discern in dark-skinned individuals, serve as a reliable guide of the depth of pigment incontinence. If observed carefully [Figure - 1], the color and hue of the dots, globules and other structures visible in original [Figure - 2], [Figure 3], [Figure 4] can be appreciated to range from brownish-black to brown to dark grayish-brown. The color as well as the size of the dots are very relevant for the dermoscopic differentiation of conditions closely simulating lichen planus pigmentosus, especially ashy dermatosis. In fact, one of our authors (EE) has reported dermoscopic differentiation between lichen planus pigmentosus and ashy dermatosis.[6] Presence of gray-bluish small dots over a bluish background (corresponding to the Tyndall effect generated by melanophages/melanin deposits in deeper dermis) was typical of ashy dermatosis in contrast to lichen planus pigmentosus, that displayed larger dots/globules having a brownish shade (melanophages/melanin deposits being located relatively more superficially, resulting from the peculiar lichenoid inflammation occurring just below the epidermis).[6] These findings were suitably based on polarized dermoscopy. It is important to mention here that, despite some workers considering ashy dermatosis to be a variant of lichen planus pigmentosus, the two entities have been reported to be different based on a large case series.[7] The latest attempt by Chandan and Kumarsinghe to provide clarification of the confusing nosology based on the available literature has also strongly supported the latter opinion.[8] Last but not the least, the nosological controversy has hitherto been the domain of clinicohistological correlation.[7],[8] It is likely that dermoscopy and clinico-dermoscopic-pathological correlation may hold the key to a clear distinction or unification thereof of such overlapping entities.[9]
- One of the characteristic dermoscopic descriptive features of facial melanoses reported in a majority of previous cases and studies and in our own experience is the background color,[10],[11],[12] which is usually light-to-dark brown in lichen planus pigmentosus in darker skin types. In fact, in most of the dermoscopy figures in the study being discussed, there is a conspicuous diffuse light to dark-brown background, faint erythema along the exaggerated pigment network and larger dark-colored structures (clods or blotches), which have not been commented upon.
- Authors have further described a novel dermoscopic finding in lichen planus pigmentosus, the 'targetoid lesion' (depicted in original [Figure 6]), characterized by “a central dot surrounded by a hypopigmented halo,” and correlated it with follicular plugging on histopathology. In that figure, authors have highlighted brown dots within white “halo” within two marked yellow squares. Notwithstanding the fact that periappendageal pigment clustering has been reported in lichen planus pigmentosus,[10] a wholesome field view of [Figure 6] of the original manuscript clearly reveals the simple random spread of brown dots/globules (due to pigment incontinence) and white dots (some of which represent the normal eccrine openings), which are rimming or overlapping at places [Figure - 2]. In fact, even we are curious about the other larger, vague, white areas visible in that image and would request the authors to enlighten about the histogenesis of these areas. Further support to our contention in this regard has come from the recently published interesting study by Vinay et al., who, for the sake of treatment planning and prognostication clubbed lichen planus pigmentosus, Riehl's melanosis and ashy dermatosis into acquired dermal macular hyperpigmentation (ADMH).[5] Interestingly, even their cases (excepting one) that had the most extensive pigment incontinence showed sparing of eccrine and follicular openings. And their description of owl's eye structure (central dark dot surrounded by a white halo) clearly excluded the white halos representing eccrine openings; furthermore, the authors' (Vinay et al.) suspicion of the owl's eye structures representing follicular plugs was ruled out on histopathology. The presence of follicular plugs in such a setting has in fact been reported to be a clue of another specific condition, erythromelanosis follicularis faciei et colli.[13]
- Although the authors' effort of exploring a correlation of the dermoscopic and histopathological features with patch test reactivity is commendable, their subsequent self-admission about the nosological overlap between lichen planus pigmentosus and Riehl's melanosis and the lack of consensus on the two conditions being different or representing a continuum of a morphological spectrum, tends to countervail it.
To conclude, we recommend: (a) approach to dermoscopic characterization of any condition should be systematic and dermoscopic features must be closely examined before committing a specific feature to the condition being studied, (b) using the appropriate type of dermoscopic mode (polarized dermoscopy vs nonpolarized dermoscopy) depending on the condition under evaluation and ensuring that the details of the same are mentioned in the study. Using both the modes is complimentary and can emphasize on specific features. The findings of a recently published survey by one of the authors (FK) and co-workers suggested that lack of familiarity and proper training were the most important reasons for Indian dermatologists not using dermoscopy.[14] It is thus only fair that exerting caution in the relatively virginal study of a novel technique, that too for a condition like lichen planus pigmentosus that remains a semantic, etiological as well as therapeutic enigma, be imperative for all researchers.
 |
| Figure 1: Composite figure reconstructed from original [Figure - 2],[Figure 3],[Figure 4], displaying dots and globules in different colors and hue – brown (white arrows), brownish-black (yellow), and greyish-brown (red arrows). The yellow and black-colored squares/circles were present in the original images. (Dermoscopy, ×10, ? polarization mode undefined) |
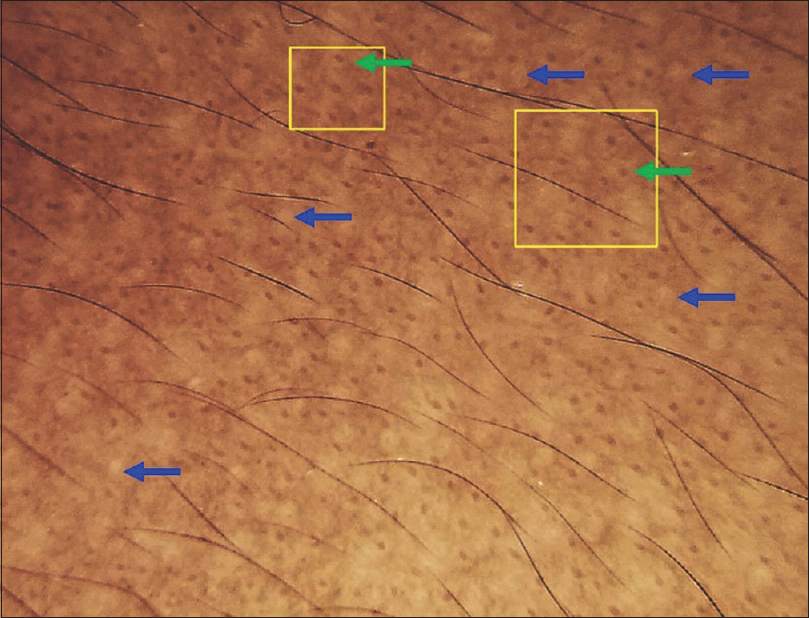 |
| Figure 2: Original Figure 6 from the study with re-interpretation of dermoscopy features – Light to dark brown background with numerous randomly distributed brown dots, interspersed with white dots, some of which represent the normal eccrine openings (blue arrows). At few places, the brown dots are giving a “targetoid appearance” due to being localized in the centre of the white dots (green arrows) (Dermoscopy, ×10,?polarization mode undefined) |
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sharma VK, Gupta V, Pahadiya P, Vedi KK, Arava S, Ramam M, et al. Dermoscopy and patch testing in patients with lichen planus pigmentosus on face: A cross-sectional observational study in fifty Indian patients. Indian J Dermatol Venereol Leprol 2017;83:656-62.
[Google Scholar]
|
| 2. |
Pan Y, Gareau DS, Scope A, Rajadhyaksha M, Mullani NA, Marghoob AA, et al. Polarized and nonpolarized dermoscopy: The explanation for the observed differences. Arch Dermatol 2008;144:828-9.
[Google Scholar]
|
| 3. |
Benvenuto-Andrade C, Dusza SW, Agero AL, Scope A, Rajadhyaksha M, Halpern AC, et al. Differences between polarized light dermoscopy and immersion contact dermoscopy for the evaluation of skin lesions. Arch Dermatol 2007;143:329-38.
[Google Scholar]
|
| 4. |
Agero AL, Taliercio S, Dusza SW, Salaro C, Chu P, Marghoob AA, et al. Conventional and polarized dermoscopy features of dermatofibroma. Arch Dermatol 2006;142:1431-7.
[Google Scholar]
|
| 5. |
Vinay K, Bishnoi A, Parsad D, Saikia UN, Sendhil Kumaran M. Dermatoscopic evaluation and histopathological correlation of acquired dermal macular hyperpigmentation. Int J Dermatol 2017;56:1395-9.
[Google Scholar]
|
| 6. |
Errichetti E, Angione V, Stinco G. Dermoscopy in assisting the recognition of ashy dermatosis. JAAD Case Rep 2017;3:482-4.
[Google Scholar]
|
| 7. |
Vega ME, Waxtein L, Arenas R, Hojyo T, Dominguez-Soto L. Ashy dermatosis and lichen planus pigmentosus: A clinicopathologic study of 31 cases. Int J Dermatol 1992;31:90-4.
[Google Scholar]
|
| 8. |
Chandran V, Kumarasinghe SP. Macular pigmentation of uncertain aetiology revisited: Two case reports and a proposed algorithm for clinical classification. Australas J Dermatol 2017;58:45-9.
[Google Scholar]
|
| 9. |
Sonthalia S, Errichetti E. Dermoscopy – Not just for diagnosis and not just for dermatologists! Kathmandu Univ Med J 2017;15:1-2.
[Google Scholar]
|
| 10. |
Pirmez R, Duque-Estrada B, Donati A, Campos-do-Carmo G, Valente NS, Romiti R, et al. Clinical and dermoscopic features of lichen planus pigmentosus in 37 patients with frontal fibrosing alopecia. Br J Dermatol 2016;175:1387-90.
[Google Scholar]
|
| 11. |
Errichetti E, Stinco G. Dermoscopy in general dermatology: A practical overview. Dermatol Ther (Heidelb) 2016;6:471-507.
[Google Scholar]
|
| 12. |
Sonthalia S, Jha AK, Langar S. Dermoscopy of melasma. Indian Dermatol Online J 2017;8:525-6.
[Google Scholar]
|
| 13. |
Errichetti E, Pizzolitto S, Stinco G. Dermoscopy of erythromelanosis follicularis faciei et colli. Actas Dermosifiliogr 2017;108:779-81.
[Google Scholar]
|
| 14. |
Kaliyadan F, Ashique KT, Jagadeesan S. A survey on the pattern of dermoscopy use among dermatologists in India. Indian J Dermatol Venereol Leprol 2018;84:120.
[Google Scholar]
|
Fulltext Views
16,926
PDF downloads
3,784





