Translate this page into:
Desquamative gingivitis in dermatological disorders
Corresponding author: Dr. Ramesh M. Bhat, Department of Dermatology, Father Muller Medical College, Mangalore - 575 002, Karnataka, India. rameshderma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ramesh A, Bhat RM, Madhumita M, Jaganathan P. Desquamative gingivitis in dermatological disorders. Indian J Dermatol Venereol Leprol 2021;87:446-51.
Introduction
“Desquamative gingivitis” was introduced by Prinz in 1932 as a descriptive term to denote the presence of erythema, desquamation, erosion and blistering of the gingival epithelium (free and attached gingiva) [Table 1].1 In 1960, McCarthy et al. proposed that it was a nonspecific clinical response of the gingiva to various mucocutaneous conditions and not a diagnosis per se.2 Nearly 75% of reported cases have a dermatological origin, majority being caused by lichen planus, mucous membrane pemphigoid and pemphigus vulgaris.3
| Reaction pattern of masticatory mucosa to various dermatoses |
| Fiery, red, glazed, friable appearance of gingiva |
| Painful blistering desquamation, erosions and ulcers |
| Commonly affects facial gingiva(In health, thefacial gingivabegins at the mucogingival junction and continues coronally, covering the alveolar process to the free gingival margin) |
| Marginal gingiva less commonly involved |
| Biopsy with DIF is essential for diagnosis |
| Topical steroids with oral hygiene is the mainstay of treatment |
Desquamative gingivitis occurs commonly in women in their fourth and fifth decades of life. But it can also be seen during puberty or in the seventh or eighth decade.3 It was initially thought to occur solely in post-menopausal women with hormonal imbalance. It is rare in children.3
Detailed clinical history with an emphasis on the duration of the lesions, habits which worsen the condition and details of previous therapy are mandatory. Thorough clinical examination of the pattern of distribution of the lesions (focal or multifocal with or without confinement to the gingival tissues) and presence or absence of Nikolsky’s sign, serve as a valuable tool in identifying the underlying dermatoses and their activity.3 An incisional biopsy for histopathological confirmation of the condition is essential. Immunofluorescence increases the diagnostic accuracy for the associated dermatological condition.4
Desquamative gingivitis is frequently associated with some underlying dermatological conditions (mainly mucocutaneous conditions and vesiculobullous disorders). Other conditions include bacterial, fungal and viral infections, 2 hormonal imbalance, drug abuse, allergic reactions to tooth-paste or mouthwashes and those with idiopathic etiology.4 Differential diagnoses of desquamative gingivitis include necrotizing ulcerative gingivitis and chronic destructive periodontal disease.2
Etiology of Desquamative Gingivitis
Dermatological conditions: Dermatological conditions causing desquamative gingivitis commonly include pemphigus vulgaris [Figure 1], cicatricial pemphigoid and oral lichen planus. Diseases such as bullous pemphigoid, epidermolysis bullosa acquisita, erythema multiforme, systemic lupus erythematosus, linear IgA disease, chronic ulcerative stomatitis and paraneoplastic pemphigus may also cause desquamative gingivitis.5,6
Endocrine disturbances: Hypothyroidism, estrogen deficiency and testosterone imbalance
Chronic infections: Tuberculosis, chronic candidiasis and histoplasmosis
Malignancies: Gingival squamous cell carcinoma may be mistaken for desquamative gingivitis.
Miscellaneous causes: Sarcoidosis, Crohn’s disease, leukemia, aging.

- Desquamative gingivitis in a female patient with pemphigus vulgaris
Clinical Characteristics of Desquamative Gingivitis in Dermatological Disorders
Lichen planus
Lichen Planus (LP) is the most common cause of desquamative gingivitis. It is responsible for nearly 45% of cases of desquamative gingivitis.6 It most frequently affects the posterior buccal mucosa, lateral border of the tongue and gingiva.7 Desquamative gingivitis may be the only manifestation in 10% of cases of oral LP.5 The atrophic variant of oral LP often presents on the gingiva and in some cases may affect the whole thickness of the attached gingiva. Plaque induced gingivitis may complicate the clinical picture. Lesions of oral LP may be associated with vulvovaginal lesions of LP(“vulvovaginal-gingival syndrome”).4,7 The vulvovaginal and gingival lesions are either coincidental, as is often the case, or one often follows the other within two years of its onset. Lichenoid oral lesions may also exist alongside lichen sclerosus lesions in the mouth and vulva which is referred to as “lichen planus/lichen sclerosus overlap syndrome”.8 Local examination of the gingiva in such patients may reveal erythematous gingiva with faint keratotic lines. The rest of the oral mucosa and the skin need to be carefully checked for classical lichenoid lesions [Figure 2].

- Desquamative gingivitis in a female patient with lichen planus
Immune mediated blistering disorders
Desquamative gingivitis is a presenting feature, in virtually every patient with mucous membrane pemphigoid.3 Nearly 35% of the cases of desquamative gingivitis have been attributed to mucous membrane pemphigoid [Figure 3].2 A common presentation is erythematous gingiva with lack of stippling which spreads apically from the gingival margins to the alveolar mucosa. There may be areas of superficial erosions with tags of detached epithelium in the gingiva.9 Vesiculobullous lesions and positive Nikolsky’s sign may be present.

- Desquamative gingivitis as an early presenting feature of mucous membrane pemphigoid
Oral lesions are cardinal manifestations of many disorders of pemphigus group, particularly pemphigus vulgaris. It is characterized by severe gingival desquamation, erosions and ulcers from ruptured bullae. 5 Positive Nikolsky’s sign can be seen. Desquamative gingivitis is also seen in IgA pemphigus (intraepidermal IgA pustulosis) and paraneoplastic pemphigus.6 In some cases, oral lesions may be the sole manifestation which may accompany, precede, or follow cutaneous lesions.
Though desquamative gingivitis is rare in dermatitis herpetiformis, erythema with white lesions and erosions may be seen in the buccal and lingual gingiva along with a background of gluten-sensitive enteropathy.5
Adult linear IgA disease can produce oral vesicles, ulcers and gingival lesions in the form of desquamative gingivitis.10 Chronic bullous disease of childhood may present similarly and additionally be associated with scarring.11
Miscellaneous Conditions
Chronic ulcerative stomatitis
It is a rare recalcitrant autoimmune disease characterized by painful chronic oral lesions similar to erosive LP. The findings include ulcers and erosions in the gingival, buccal and lingual mucosae. It may rarely be associated with genital and conjunctival mucosal lesions. DIF studies show nuclear deposits of IgG in basal 1/3rd of the epithelium.11
Erythema multiforme major
Erythema multiforme major almost always involves the oral mucosa. The oral lesions may arise before or after the onset of cutaneous lesions or in isolation. It includes swollen lips, labial erosions, intra-oral blisters and serosanguinous discharge.5 Though gingival involvement is reported to be uncommon, when present it may be overlooked due to the extensive oral ulceration and sloughing seen in this condition.12
Pyostomatitis vegetans
It is a rare disorder characterized by erythema and edema of oral mucosa with numerous small superficial yellow pustules. It may also have lesions of desquamative gingivitis. It is found to be clinically associated with inflammatory bowel disease - both Crohn’s disease and ulcerative colitis. The oral lesions follow the onset of gastrointestinal symptoms.13
Systemic Lupus Erythematous
One of the cardinal manifestations of lupus erythematosus is the presence of oral lesions. The gingivitis seen here is more commonly localized rather than generalized. The type and severity of gingival lesions are directly related to disease activity. Discoid lupus erythematosus presents on the buccal mucosa and palate as lichen planus like plaques. Systemic lupus erythematosus presents as ulcerative, hyperkeratotic plaques on the palate and buccal mucosa. 14 Discoid lupus occurs with desquamative gingivitis, if the latter is characterized by labial erosions and serosanguineous discharge. Marginal edematous gingivitis with bluish red color (due to superficial capillary dilation) is a special sign of capillary involvement in dermatomyositis and mixed connective tissue disorder.14
Epidermolysis bullosa acquisita
This condition is characterized by oral mucosal fragility with recurrent blistering, scarring, microstomia and enamel defects. It may also have gingival involvement, in the form of gingival hyperkeratosis (as seen in epidermolysis bullosa simplex, Dowling – Meara type ) and desquamative gingivitis.15
Plasma cell gingivitis
This hypersensitivity reaction to mouth rinses, flavored mint/ chewing gum, etc., though rare, may present as desquamative gingivitis. It is referred to as stomatitis medicamentosa. A similar reaction may occur as a contact allergic response to drugs taken orally or parenterally (eg: penicillin, aspirin burns) and is referred to as stomatitis venenata.16
Toxic epidermal necrolysis
This condition may manifest with extensive gingival desquamation. This is particularly seen in patients with HIV-AIDS and is preceded by systemic symptoms such as fever, cough, malaise, etc.5
Tables 2 and 3 summarise the salient features of desquamative gingivitis in various dermatological and non-dermatological conditions, respectively.
| Disease | Nature of gingival involvement |
|---|---|
| Lichen planus | Reticular pattern/erosions in gingival mucosa |
| Mucous membrane pemphigoid | Desquamative gingivitis with vesicles, positive Nikolsky’s sign |
| Pemphigus | Extensive gingival erosions, desquamative gingivitis, ulcers, positive Nikolsky’s sign |
| Chronic ulcerative stomatitis | Painful recurrent gingival ulcers(similar to erosive LP) |
| Erythema multiforme (major) | Gingivo-labial erosions with sero-sanguinous exudate and swollen lips |
| Pyostomatitis vegetans | Erythema and edema of oral mucosa, desquamative gingivitis with numerous small superficial pustules |
| Connective tissue disorders (SLE, DM, PM, MCTD) | Recurrent, recalcitrant oral mucosal ulcerations with desquamative gingivitis |
| Epidermolysis bullosa acquisita | Oral mucosal friability, desquamative gingivitis, enamel defects |
LP: Lichen planus, SLE: Systemic lupus erythematosus, DM: Dermatomyositis, PM: Polymyositis, MCTD: Mixed connective tissue disorder
| Nondermatological causes | Salient features |
|---|---|
| Endocrine disturbances Estrogen deficiency after hysterectomy/oophorectomy and in postmenopausal women Testosterone imbalance Hypothyroidism |
Cellular differentiation, proliferation and keratinization of gingival epithelium is affected17 Fluctuation in FSH and LH results in inflammatory reactions, hypertrophy or atrophy of gingiva |
| Nutritional deficiency | Folic acid deficiency with oral epithelium maturation and decreased keratinization Individuals are more prone to ulcer formation18 |
| Aging | Aging causes nutritional deficiency which in turn results in desquamation (termed as “senile atrophic gingivitis”) |
| Chronic infections Tuberculosis Chronic candidiasis Histoplasmosis |
Chronic candidiasis results in erythematous gingiva with granular surface Epithelial atrophy evident with burning sensation in the mouth |
| Irritation from concentrated mouthwashes and dental materials | Allergic reactions occur due to additives like cinnamon and preservatives |
| Oxidative stress | Low level of extracellular ROS causes initial desquamation |
| Idiopathic | - |
FSH: Follicle stimulating hormone, LH: Luteinising hormone, ROS: Reactive oxygen species
Diagnosis of desquamative gingivitis
History: History taking should focus on the onset, progression, aggravating factors, relieving factors and prior treatment taken. Patients may be asymptomatic or more commonly complain of persistent soreness of the gingiva, mild burning sensation or intense pain of the affected site.2 The symptoms may be aggravated by intake of acidic foods such as citrus fruits. Also, look for intentional or unintentional aggravating local factors like masticatory forces, poor dental restorations, plaque accumulation, etc. Symptoms are known to occur in cycles of remission and exacerbation
Examination: General examination is pivotal in determining the involvement of other mucosal surfaces and the pattern of distribution. A thorough examination to find out any cutaneous involvement is also important. It is also essential to identify any underlying systemic disease.
Local examination
Desquamative gingivitis clinically appears as fiery red, glazed, atrophic or eroded gingiva, particularly seen on the buccal/labial surface of the gingival epithelium (free and attached gingiva).4,5 Less severe cases present with erythema and edema. In cases with greater severity, paraesthesia, mucosal desquamation with blister formation, erosions and ulcerations can be seen. A thorough local examination is important to not only characterize the peculiar features of desquamative gingivitis in different dermatoses [Table 2] but also to elicit Nikolsky’s sign (formation or spread of blister on application of lateral pressure to the normal looking mucosa) which is diagnostic of many vesiculobullous diseases.
Investigations
Histopathological examination
Biopsy of the perilesional mucosa is preferred to that of the ulcerated mucosa.2,5
Formalin-fixed, paraffin-embedded tissue stained with conventional H and E is obtained for light microscopy examination [Figure 4].
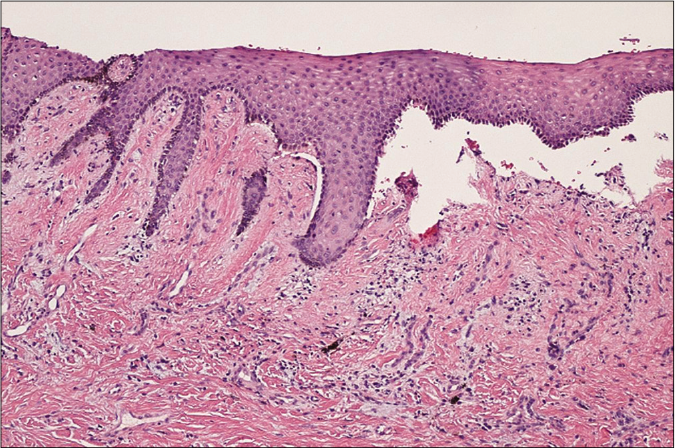
- Histopathology showing sub-epithelial cleft and basal cell degeneration, along with chronic inflammatory cells and haemorrhagic areas, in mucous membrane pemphigoid (H and E, ×100, low power magnification)
Table 4 highlights the histological features of common mucocutaneous diseases presenting with desquamative gingivitis.
| Disease | Histopathology |
|---|---|
| Lichen planus | Hyperkeratosis, hydropic degeneration of the basal layer and sawtoothed rete pegs; lamina propria shows dense, bandlike infiltrate, primarily of lymphocytes; colloid bodies are present |
| Mucous membrane pemphigoid | Subepithelial clefting with epithelial separation from the underlying lamina propria with an intact basal layer |
| Pemphigus | Intraepithelial clefting above the basal cell layer; basal cells have a characteristic “row of tombstone” appearance; acantholysis is present |
| Chronic ulcerative stomatitis | Hyperkeratosis, acanthosis, basal cell layer liquefaction, subepithelial clefting and chronic lymphohistiocytic infiltrate in a bandlike configuration |
| Dermatitis herpetiformis | Collection of neutrophils, eosinophils and fibrin in the connective tissue papillae |
| Bullous pemphigoid | Subepithelial clefting with epithelial separation from the underlying lamina propria, leaving an intact basal layer |
| Systemic Lupus erythematosus | Hyperkeratosis, basal cell degeneration, epithelial atrophy and perivascular inflammation |
| Epidermolysis bullosa acquisita | Subepithelial clefting with epithelial separation from the underlying lamina propria, leaving an intact basal layer |
Immunofluorescence studies
In direct immunofluorescence, unfixed frozen sections are incubated with a variety of fluorescein-labeled, antihuman sera (i.e., anti-IgG, anti-IgA, anti-IgM, antifibrin and anti-C3) [Figure 5]. With indirect immunofluorescence, unfixed frozen sections of oral or esophageal mucosa from monkeys are first incubated with the patient’s serum to allow for the attachment of any antibodies to the mucosal tissue. Table 5 summarises the immunofluorescence findings in select dermatological conditions presenting as desquamative gingivitis.
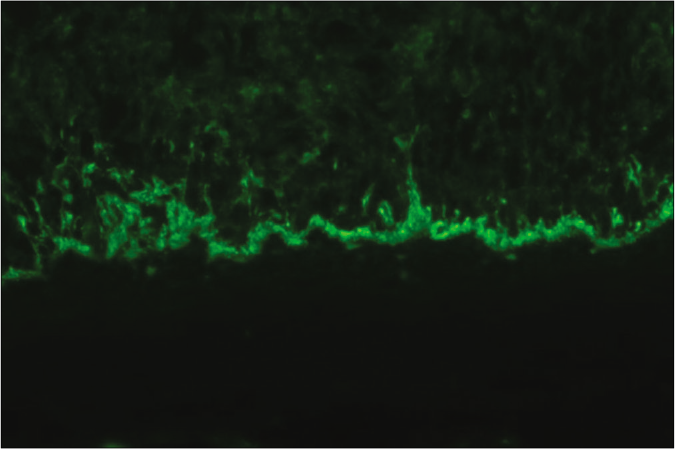
- Direct immunofluorescence showing a linear deposition of IgG and C3 at the dermo-epidermal junction, in mucous membrane pemphigoid
| Disease | DIF | IIF | |
|---|---|---|---|
| Mucosa | Serum | ||
| Lichen planus | Fibrillar deposits of fibrin at the dermal-epidermal junction | Negative | Negative |
| Mucous membrane pemphigoid | Linear deposits of C3 with or without IgG at the basement membrane zone in almost all cases | Same as for perilesional mucosa | Basement membrane zone(IgG) antibodies in 10% of cases |
| Pemphigus | Intercellular deposits in the epithelium; IgG in all cases and C3 in most cases | Same as for perilesional mucosa | Intercellular (IgG) antibodies in ≥90% of cases |
| Chronic ulcerative stomatitis | IgG deposits in the nuclei of the basal layer of epithelial cells | Same as for perilesional mucosa | ANA specific for basal cells of stratified squamous epithelium |
| Dermatitis herpetiformis | IgA deposits in the dermal papillae in 85% of cases | Same as for perilesional mucosa | IgA endomysial antibodies in 70% of cases; antigliadin antibodies in 30% of cases |
| Bullous pemphigoid | Linear deposits of C3 with or without IgG at the basement membrane zone in almost all cases | Same as for perilesional mucosa | IgG antibodies against basement membrane zone in 40%-70% of cases |
| Systemic lupus erythematosus | IgG or IgM with or without C3 deposits at the dermal-epidermal junction | Same as for perilesional mucosa | ANA in >95% of cases; DNA and ENA antibodies in >50% of cases |
| Epidermolysis bullosa acquisita | Linear deposits of IgG and C3 at the basement membrane zone in almost all cases | Same as for perilesional mucosa | Basement membrane zone(IgG) antibodies in 25% of cases |
DIF: Direct immunofluorescence, IIF: Indirect immunofluorescence, ANA: Anti-nuclear antibodies, ENA: Extractable nuclear antigen.
Conditions that Mimic Desquamative Gingivitis
Foreign body gingivitis
It is a non-plaque induced chronic inflammatory process that may seldom involve the gingiva.17 It is triggered by the introduction of foreign particulate material such as dental restorative material or dental prophylaxis paint. It may present as a lichenoid or granulomatous response masquerading as desquamative gingivitis.
Candidiasis
Oral candidiasis, particularly in immune-compromised patients, may involve the gingiva. This gives it an erythematous and granular appearance, often mistaken as desquamative gingivitis.18
Wegener’s granulomatosis
Oral lesions are seen in around 6% of cases.19 They manifest as mouth ulcers and erythematous, painful gingival enlargement (“strawberry gingivitis”). This can be confused with desquamative gingivitis.20
Graft-versus-host disease
Following allogeneic hematopoetic stem cell transplantation oral graft-versus-host disease which affect the gingiva may occur. This results in epithelial desquamation, erythema and erosions of the buccal, glossal and labial gingiva, presenting a “desquamative gingivitis” type of clinical appearance.21
Kindler’s syndrome
The oral manifestations include erosive and erythematous appearance of the gingiva. The salient cutaneous features include neonatal bullae, poikiloderma, photosensitivity and acral atrophy.22
Factitious gingivitis
Self- inflicted oral injuries, though atypical in their site and nature of occurrence, may potentially appear like lesions of desquamative gingivitis.23
Squamous cell carcinoma
Gingival squamous cell carcinoma arising from the keratinized mucosa results in gingival enlargement and may be misdiagnosed as desquamative gingivitis.19
Treatment
Management of desquamative gingivitis requires a thorough elicitation of medical history. It is followed by clinical and laboratory confirmation. Differentiation of the disorders provides good prognosis and successful management of the condition.6
General Considerations in Treatment
Treatment of the underlying disease: Prompt identification and appropriate control of the underlying dermatological disease are key to resolution of the lesions of desquamative gingivitis.24
Oral Hygiene: Patients should be educated to perform oral hygiene procedures without causing any mechanical or chemical trauma. This must be emphasised as improper brushing/flossing technique will aggravate the lesions
If the hypersensitivity to allergens is confirmed after a skin patch test, topical substances including antiseptic mouthwashes, toothpaste with sodium lauryl sulphate, cosmetics, flavors and food additives, should be avoided.
Drugs found to be responsible for the disease should be stopped
Enhancement of plaque control measures need to be carried out
During air abrasive polishing, caution must be taken not to apply to gingiva, as it can penetrate them and worsen the condition.
Symptomatic Treatment
Topical corticosteroids are the first line of treatment for localised lesions.6,25
Mild localised lesions can be effectively managed with fluorinated compounds like fluocinonide (0.05%), whereas more severe lesions benefit from the use of clobetasol propionate (0.05%), triamcinolone orabase (0.1%) and topical tacrolimus (0.03%, 0.1%, 0.3%)
Gel-based formulations are preferred due to their ready absorption in the oral mucosa. It is further enhanced by the use of custom-built splints, silicone or acrylic carriers
Intralesional corticosteroid injections (triamcinolone at a dose of 0.5-1 ml of a 1mg/ml suspension) can be given 2-4 times a week for severe exacerbation of desquamative gingivitis/recalcitrant desquamative gingivitis
In case of failure of topical therapy, oral prednisolone can be given at a dose of 40-80 mg a day , for 1-2 weeks and tapered rapidly. In children, considering the age and potential side effects of oral steroids, dapsone is preferred in severe, refractory cases of desquamative gingivitis.
Pulse therapy with oral methylprednisolone (1 mg/kg/ day for three days a week), steroid-sparing agents such as azathioprine, cyclosporine and dapsone may also be used
Benzydamine hydrochloride 0.15% mouth rinse can be administered as an analgesic
Superinfection with candida can be treated with anti-fungal drugs
Conclusion
Desquamative gingivitis is not a disease sui generis and it is a reaction pattern of the gingiva to various underlying dermatoses. Correct diagnosis of the condition involves taking a detailed history, in conjunction with intra and extraoral examination and gingival biopsy for histopathology and immunofluorescence studies. Presence of co-existing or subsequently occurring lesions in the skin as well as in the ocular and genital mucosae have to be promptly identified and managed accordingly. A regular and thorough examination of the oral cavity is of paramount importance in such patients to effectively treat the underlying pathology. The use of occlusive topical corticosteroids and improvement of oral hygiene are the pillars in the management of desquamative gingivitis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Chronic desquamative gingivitis: A reconsideration. Oral Surg. 1960;13:1300-13.
- [CrossRef] [Google Scholar]
- Desquamative gingivitis In: Newman MG, Takei H, Klokkevold PR, Carranza FA, eds. Carranza's Clinical Periodontology (11th ed). New Delhi: Elsevier Health Sciences; 2011. p. :152.
- [Google Scholar]
- Desquamative gingivitis: A review. J Istanb Univ Fac Dent. 2016;50:54-60.
- [CrossRef] [PubMed] [Google Scholar]
- Desquamative gingivitis: Diagnosis and treatment. J Am Acad Dermatol. 2018;78:851-61.
- [CrossRef] [PubMed] [Google Scholar]
- Desquamative gingivitis: Clinical findings and diseases. J Am Acad Dermatol. 2018;78:839-48.
- [CrossRef] [PubMed] [Google Scholar]
- Desquamative gingivitis as a manifestation of chronic mucocutaneous disease. J Dtsch Dermatol Ges. 2011;9:184-8.
- [CrossRef] [PubMed] [Google Scholar]
- Mucosal lichen sclerosus/lichen planus overlap syndrome with cutaneous lesions of lichen sclerosus. Eur J Dermatol. 2016;26:204-5.
- [CrossRef] [PubMed] [Google Scholar]
- Desquamative gingivitis-A clinical sign in mucous membrane pemphigoid: Report of a case and review of literature. J Pharm Bioallied Sci. 2014;6:122-6.
- [CrossRef] [PubMed] [Google Scholar]
- Linear IgA and IgG bullous dermatosis. An Bras Dermatol. 2016;91:32-4.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic ulcerative stomatitis: Case series of an under recognized entity. J Cutan Pathol. 2018;45:927-32.
- [CrossRef] [PubMed] [Google Scholar]
- Oral mucosal diseases: Erythema multiforme. Br J Oral Maxillofac Surg. 2008;46:90-5.
- [Google Scholar]
- Pyostomatitis vegetans in ulcerative colitis; management with topical tacrolimus and systemic azathioprine in a 10 year old boy (case report and review of the literature) J Int Oral Health. 2016;8:132-6.
- [Google Scholar]
- Oral manifestations of autoimmune connective tissue diseases. Indian J Rheumatol. 2018;13:264-72.
- [CrossRef] [Google Scholar]
- Periodontal manifestation of epidermolysis bullosa: Looking through the lens. J Indian Soc Periodontol. 2016;20:72-4.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma cell gingivitis: A rare and perplexing entity. J Indian Acad Oral Med Radiol. 2016;28:94-7.
- [CrossRef] [Google Scholar]
- Studies on the biology of the periodontium of marmosets: VIII. The effect of folic acid deficiency on the marmoset oral mucosa. J Dent Res. 1970;49:616-20.
- [CrossRef] [PubMed] [Google Scholar]
- Desquamative gingivitis: Does the gingiva tell you more than what meets the eye? A comprehensive review. J Adv Clin Res Insights. 2019;6:48-52.
- [CrossRef] [Google Scholar]
- Gingival manifestations of Wegener's granulomatosis. J Periodontol. 1990;61:705-9.
- [CrossRef] [PubMed] [Google Scholar]
- Oral manifestation and dental management in a patient with chronic graft versus host disease with around a 10 year follow up. Biomed Res Ther. 2018;5:2370-7.
- [CrossRef] [Google Scholar]
- Clinical and microbiologic study of periodontitis associated with Kindler syndrome. J Periodontol. 2003;74:25-31.
- [CrossRef] [PubMed] [Google Scholar]
- Factitious desquamative gingivitis simulating a possible immunologi disease. J Allergy Clin Immunol. 1987;75:44-6.
- [CrossRef] [Google Scholar]
- Oral hygiene instructions and professional control as part of the treatment of desquamative gingivitis. Systematic review. Med Oral Patol Oral Cir Bucal. 2019;24:e136-44.
- [CrossRef] [PubMed] [Google Scholar]
- Multidisciplinary management of desquamative gingivitis with periodontal disease. Ann Dent UM. 2019;26:30-3.
- [CrossRef] [Google Scholar]





