Translate this page into:
Diagnosis and management of psoriatic arthritis
2 Department of Dermatology, P. D. Hinduja National Hospital, Mahim, Mumbai, India
Correspondence Address:
Canchi Balakrishnan
Department of Rheumatology, P. D. Hinduja National Hospital, Veer Savarkar Marg, Mahim, Mumbai - 400 016
India
| How to cite this article: Balakrishnan C, Madnani N. Diagnosis and management of psoriatic arthritis. Indian J Dermatol Venereol Leprol 2013;79:18-24 |
Abstract
Psoriatic arthritis (PsA) is a multi-faceted disease marked by varying combinations of peripheral arthritis, dactylitis, spondylitis, and enthesitis. Rarely, recurrent uveitis occurs. Skin involvement may or may not exist. However, patients with nail psoriasis have a higher probability of developing PsA. Untreated patients have significant morbidity and mortality. Timely diagnosis and aggressive treatment of the disease can lead to lower morbidity. Drug therapy of PsA includes symptomatic therapy and therapy with disease-modifying anti-rheumatic drugs. Biologics are the only agents that address all the pathological changes, of this chronic condition.Introduction
Over the last decade, significant strides have been made in our understanding of psoriatic arthritis (PsA). There is recognition that PsA is a multi-faceted disease, often with differing pathologies at different sites. [1] Patients often have varying combinations of peripheral arthritis, spondylitis, dactylitis, and enthesitis. In a proportion of patients, the presence of extra-articular manifestations like recurrent uveitis also influences therapeutic decisions. [2],[3] Untreated patients with PsA have significant morbidity and probably early mortality. [2],[3] Increased cardiovascular mortality due to inflammation-mediated premature atherogenesis has also been described. [4] Hence, there is a need to diagnose, stage, and treat this disease aggressively.
Diagnosis of PSA
The presence of inflammatory arthritis in a patient with past or current psoriasis is the basis of diagnosis of PsA. However, in about 10% to 20% of patients, there is no history of obvious skin involvement by psoriasis. In these patients, one should search diligently for psoriasis at hidden sites such as the natal cleft, behind the ear, in the umbilicus, and on the scalp, and for nail changes like nail pitting, onycholysis and total nail dystrophy.
Various diagnostic criteria have been proposed for PsA [5],[6],[7],[8] including the widely used Moll and Wright criteria. This criteria necessitates the presence of:
- Psoriasis vulgaris
- A negative serology for rheumatoid arthritis (RA)
- Clinical features suggestive of inflammatory arthritis in one or more of the following patterns:
- Distal interphalangeal joint disease
- Asymmetric, oligoarticular (< 5 joints involved)
- Symmetric, polyarticular "rheumatoid arthritis-like",
- Mainly spondylitic (axial involvement)
- Destructive arthritis (arthritis mutilans)
The group for research and assessment of psoriasis and psoriatic arthritis (GRAPPA) has selected three simple screening tools, which can be used by clinicians to screen for PsA. [10] These are still undergoing validation in population studies.
- Toronto Psoriatic Arthritis Screening Tool (ToPAS)
- Psoriasis Epidemiology Project (PEST)
- Psoriatic Arthritis Screening and Evaluation tool (PASE)
The sensitivity of most of the above criteria has been compared. The criteria by Vasey and Espinzoa, McGonagle and the CASPAR criteria exhibited a sensitivity of almost 96%. The specificity of the various criteria was anywhere between 93% and 99%. One would choose a more sensitive criteria when conducting community based studies especially of early PsA and specific criteria when doing drug trials.
As dermatologists, concentrating on psoriasis of the skin and nail, we may be missing many cases of early arthritis. Dactylitis, a uniform sausage-like swelling of the fingers and toes, and enthesitis, which is pain and inflammation at the point of tendon insertion, may be early signs of arthritis in these patients. Furthermore, nail involvement is postulated to be due to a Koebner′s phenomenon secondary to enthesitis of the distal phalanx, and may be predictive for the development of PsA. [11] Recently, Soscia et al. have studied nails with magnetic resonance imaging (MRI), and concluded that MRI can detect nail changes in patients of psoriasis even when there is no clinical evidence in any nail. [12]
Differential Diagnosis
PsA needs to be distinguished from other common forms of arthritis, viz. rheumatoid arthritis, osteoarthritis, connective tissue disease, infective, and gouty arthritis. Oligoarticular disease, asymmetry, distal interphalangeal joint involvement [Figure - 1], enthesitis, and negative serology are typical of PsA. Those with rheumatoid arthritis may have, in addition, rheumatoid nodules and extra-articular signs without enthesitis and central axial involvement. Osteoarthritis mainly involves the knee and hip joints, occurring with "wear and tear" of the joints. Lupus arthritis, occurring in patients of systemic lupus erythematosus, affects the wrists, hands, and knees. Anti-nuclear antibody (ANA) and dsDNA may be positive. An acutely swollen, painful joint swelling may be seen in infective/septic arthritis or gouty arthritis. Culture of the joint fluid will reveal the causative organism. A negative culture should alert to the possibility of gouty arthritis. Elevated serum uric acid level helps to confirm the diagnosis. Gouty arthritis is usually monoarticular, commonly involving metatarsophalangeal joint. A radiograph of the affected joint shows lytic areas with sclerotic margins described as "rat bite" lesions.
 |
| Figure 1: Distal interphalengeal joint (DIP) of the ring fi nger showing erythema and swelling suggestive of arthritis. Plaque of psoriasis also seen on the dorsum of the hand. DIP involvement is never seen in RA |
Investigations
The following hematologic, serologic, and imaging studies, although not specifically diagnostic, can be supportive.
- The erythrocyte sedimentation rate and C-reactive protein may be raised, but this is not specific.
- Rheumatoid factor test should be performed. Although, a negative serology can rule out rheumatoid arthritis, about 25% of PsA patients of the rheumatoid type may have a positive or equivocal test result. [13]
- HLA-B27, though not specific, is strongly supportive of axial disease.
- X-rays of the hands and feet may be needed [Figure - 2]. Early changes may be limited to peri-articular soft tissue swelling and joint erosions similar to rheumatoid arthritis. Sites of entheseal attachments may show periostitis and new bone formation. Advanced cases, especially of the mutilating variety, may show widespread joint destruction, with "penciling" or narrowing of the heads of the metacarpals and metatarsals. Destruction of the central portion of the articular surface gives the "pencil-in-cup" appearance. With the destruction of the interphalangeal joints, especially the distal ones, bony ankylosis can occur.
- The sacroiliac changes in PsA are similar to those in ankylosing spondylitis, but with the ossification of the paravertebral tissues in the thoracic and lumbar area occurring more laterally. [14]
- Ultrasound and MRI are more effective for the detection of enthesitis. [15]
- Lipid profile, HbA1C, liver function tests (LFT), body mass index (BMI) for evaluating co-morbidities.
 |
| Figure 2: Radiograph of both hands showing fl uffy periosteitis in the proximal phalanges of all fi ngers bilaterally. A soft tissue swelling is seen around the middle finger of the left hand suggestive of "sausage digit" |
Management of PSA
Treatment needs to be holistic and includes drug therapy and management of co-morbidities such as obesity, deranged lipid profile, abnormal liver functions, and underlying diabetes mellitus. A BMI> 25 kg/m 2 increases the risk of PsA. [16] Such patients need encouragement for dietary changes and life-style modifications. It has been estimated that up to 50% of untreated patients may develop persistent inflammation leading to joint damage culminating into disability and deformation, severely limiting physical activity. However, there is paucity of data about reduction of PsA incidence rates if it is treated early and aggressively.
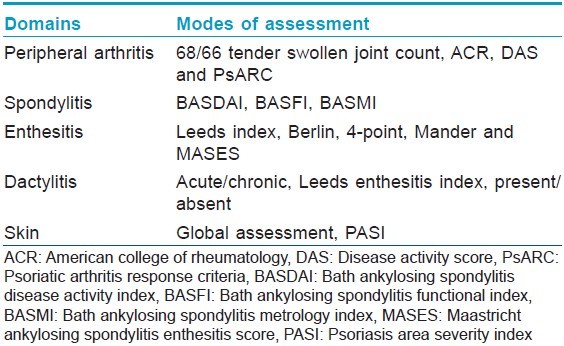
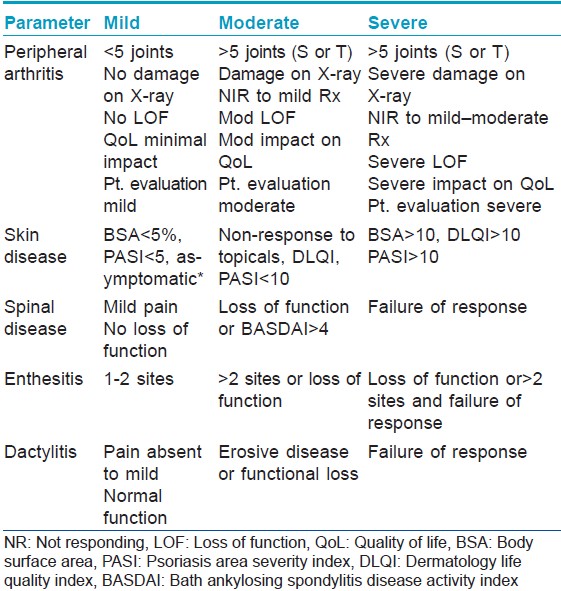
Assessment of PsA should begin with assessment of the following five domains: skin disease, peripheral arthritis, axial disease, enthesitis, and dactylitis. Various measures of assessment are available for each of these domains [Table - 1]. Based on these domains a disease severity grid has been devised [Table - 2]. Once a patient′s data has been entered in the grid, therapeutic decisions can be made.
Various organizations have laid out treatment guidelines for PsA depending on the disease severity, derived from prevalent data. Prominent among these include GRAPPA, [10] European League against Rheumatism (EULAR), [17] and the American Academy of Dermatology (AAD). [18]
Drug Therapy of PSA
Drug therapy in PsA has been extrapolated from drugs used to manage RA. These include those giving symptomatic relief and those with disease-modifying anti-rheumatic drugs (DMARDs) effect.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS)
NSAIDs are used to reduce symptoms in acute episodes of PsA. The choice of the drug depends on efficacy, adverse effects and co-morbidities. Long acting agents like celecoxib [19] and nimesulide, [20] in a dose of 200-400 mg once daily, help to control symptoms and also to reduce morning stiffness.
Corticosteroids
Systemic corticosteroids are usually avoided in PsA for the fear of precipitating of pustular psoriasis when they are withdrawn suddenly. [21] However, when low dose systemic steroids (≤ 7.5 mg/day of prednisolone) [22]
are combined with other DMARDs, good control of symptoms can be achieved. Intra-articular corticosteroid injections are reserved for mono/oligoarthritis and maybe used as an adjuvant in patients with well-controlled polyarthritis experiencing single joint flares. Intra-articular injections are also helpful in patients experiencing dactylitis and enthesitis.
DMARDs
Methotrexate (MTX), cyclosporine, and leflunomide (LEF) are often used as the first-line DMARDs in PsA because of their ability to control both, the arthritis, and the cutaneous manifestations of psoriasis.
MethotrExate
MTX has long been the mainstay drug for starting therapy in PsA. However, surprisingly, a literature search revealed only a few randomized controlled trials (RCTs) demonstrating efficacy of MTX in PsA. [23],[24],[25] In a recently concluded RCT to demonstrate the efficacy of MTX for treatment of synovitis for PsA, no improvement was noted in symptoms of synovitis and the publication questioned the role of MTX as a DMARD. [26] Another study suggested co-administration of a biologic (infliximab) for better patient outcome. [27] MTX acts via inhibition of DNA synthesis in the folate pathway, preferentially within lymphoid cells. It increases adenosine (anti-inflammatory) concentration and decreases s-adenyl methionione (pro-inflammatory) production. It is recommended to administer folic acid (1-5 mg/day) everyday, while on MTX therapy to minimize its toxicity. Early signs of MTX intolerance include oral aphthosis, stomatitis, cutaneous ulceration and increased gastrointestinal adverse events. Hepatotoxicity is the dreaded
side-effect and has been the topic for much debate. It was generally felt that patients with PsA are more prone to MTX hepatotoxicity than those with RA. However, it has been recently understood that it is not the psoriasis but the presence of pre-existing risk factors like a history of chronic viral hepatitis, consumption of excessive alcohol, hepatotoxic drugs or an inherited liver disease, which could predispose to hepatotoxicity. [28] Even so, it is safe to administer MTX by monitoring the patients with serial LFTs and tests as per the American College of Rheumatology (ACR) guidelines. A liver biopsy should only be considered if LFTs are persistently elevated. [29] MTX is teratogenic (Category X) and should be stopped in women at least 3 months before conception.
Cyclosporine A
Cyclosporine A (CyA) combines with cyclophilin and forms a complex, which inhibits the intracellular enzyme, calcineurin. This reduces IL-2 (a potentpro-inflammatory mediator) production by CD4-T cells. It also reduces other pro-inflammatory cytokines such as Granulocyte-macrophage colony stimulating factor (GM-CSF), Tumor necrosis factor-alfa (TNF-α), Interleukin (IL)-1, IL-3, IL-4, IL-5, IL-6, IL-8 by inhibiting their transcription. This effectively results in decreased T-cell and keratinocyte proliferation. CyA has been used in doses ranging from 3-6 mg/kg/day with variable outcome. Although, it shows excellent results in reducing peripheral joint disease, its role in controlling axial disease is dismal. [30] Potential, irreversible nephrotoxicity is the dreaded complication of CyA. With regular blood pressure monitoring and renal function tests, the toxicity can be kept in check. Development of hypertrichosis may be a cosmetic concern in women. Abrupt discontinuation of CyA may result in a flare of psoriasis.
Leflunomide
Kaltwasser et al., [31] randomized 190 patients of PsA and psoriasis into 2 groups. One group of 95 patients received 100 mg LEF, daily for 3 days and then 20 mg daily up to 24 weeks. The second group (91 patients) received placebo. At the end of 24 weeks, 58.9% versus 29.7% were responders. The LEF group had higher GI symptoms and abnormal LFTs as compared to the placebo group. LEF is a teratogenic drug and is contraindicated in women of childbearing potential. Women should undergo a rapid wash-out procedure with cholestyramine or should not become pregnant for 2 years after the cessation of therapy. It is advisable that men wishing to father a child should discontinue LEF and should also undergo the wash-out procedure.
Sulfasalazine (SSZ)
Large RCT for SSZ in PsA are few. In a study by Clegg Do, et al. of 264 patients comparing the efficacy of SSZ vs placebo in treating ankylosing spondylitis revealed a trend favoring SSZ treatment (P = 0.13). The authors concluded that SSZ at a dosage of 2,000 mg/day was well-tolerated and may be more effective than placebo in the treatment of patients with PsA. [32] Most of the other studies are small, precluding meaningful conclusions.
The other DMARDs used in the management of PsA include mycophenolate mofetil, [33] azathioprine, [34] antimalarials, gold, [35],[36] and penicillamine.
It is important to note that DMARDs in PsA have their limitations. Although, some of them can control psoriasis and the peripheral arthritis, they have not been shown to be of value in the other facets of PsA [Table - 3].
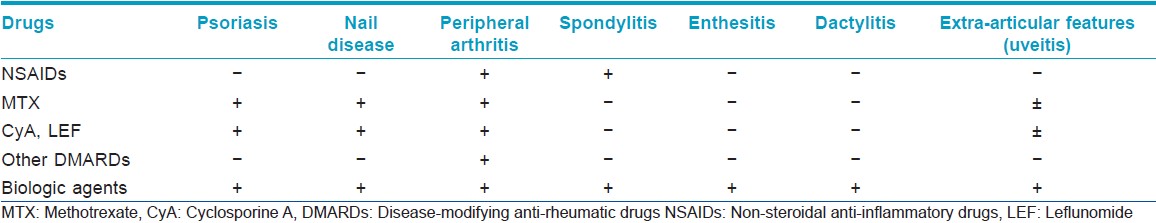
Biologic Therapy in PSA
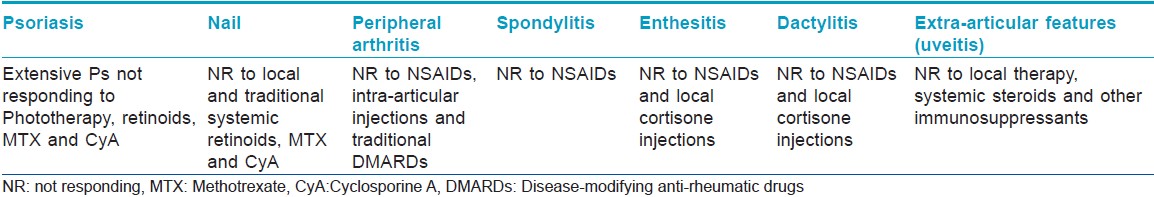
Over the last decade, targeted therapy with biologic agents has revolutionized the treatment of PsA since they are the only agents that can address all the pathological changes seen in PsA. They not only control the psoriasis but also control synovitis, enthesitis, and non-infectious inflammatory osteitis seen in PsA [Table - 3]. As a general consensus, biologic agents are reserved for resistant disease [Table - 4]. However, they may be considered as first line for the treatment of enthesitis/dactylitis and those with predominantly axial disease. [17]
Biologics target very specific components within the inflammatory pathway of psoriatic disease process. Most widely used and studied are those which block TNF-α, a potent pro-inflammatory cytokine. These include etarnercept, [37] infliximab [38],[39] and adalimumab [40] all of which have received FDA approval for treatment of PsA. Newer ones like certolizumab pegol, [41] and golimumab [42] have shown similar beneficial effects, but adequate trials are still lacking. On starting therapy, functional capacity of the joints improves dramatically. Concurrent administration of MTX improves drug survival, especially in patients receiving infliximab. [43] Patients who develop reduced/no response to their first anti-TNF-α drug can be switched over to another anti-TNF-α drug and this shows good improvement. [44]
Efalizumab, a humanized monoclonal antibody, which was in the market, has been withdrawn because of it′s complication of causing progressive multifocal leukoencephalopathy. [45]
Ustekinumab is a newer humanized monoclonal antibody, which selectively binds to the p40 subunit of IL-12 and IL-23, and inhibits their binding to the receptor IL-12Rβ1. IL-23 plays a key role in the Th17 mediated inflammatory pathway while IL-12 is a key cytokine in the Th1 inflammatory pathway. So ustekinumab can potentially inhibit both inflammatory pathways. Early clinical studies have shown to improve dactylitis and enthesitis in PsA. [46]
Alefacept inhibits LFA-3/CD2 interaction by blocking the CD2 receptor on the T lymphocytes which then prevents T-cell activation. It is important to monitor CD4 T-cell levels while on treatment with Alefacept. [47]
Tocilizumab binds to IL-6 receptor and thus inhibits the inflammatory events by IL-6. It has been approved for the treatment of rheumatoid arthritis and is currently being tried for PsA [48]
Abatacept prevents T-cell activation by inhibiting co-stimulatory signals responsible for inflammation in PsA. Hence, its use in early disease and in biologicaly naïve patients has garnered much interest.
The Danish Society of Gastroenterology has laid out detailed guidelines for investigations prior to initiating anti-TNF-α treatment. [49] Recommended tests to be done at baseline include complete hemogram, urine routine/microscopy, chest radiograph, Mantoux test, viral serology and liver and renal function tests. The issue of prophylaxis for tuberculosis is controversial and it has been suggested that all patients with a positive Mantoux test, past history of tuberculosis or abnormal chest X-ray suggestive of tuberculosis should receive prophylactic anti-tuberculosis therapy before starting the biologic therapy. All patients on anti-TNF-α therapy who develop tuberculosis should discontinue therapy and receive anti-tuberculosis chemotherapy. In the case of infliximab, monitoring needs to be continued for 6 months after discontinuing treatment due to the prolonged elimination phase of infliximab. Cautious use of DMARDs and biologics is recommended in pregnant and lactating mothers, and in patients with pre-existing liver, kidney, cardiac and neurologic dysfunction.
Conclusions
Untreated PsA leads to significant morbidity and mortality. The GRAPPA has identified screening tools, which dermatologists can use to diagnose PsA early, an important step towards proper treatment. The treatment protocol can be individualized once the disease extent and severity have been staged. Biologic agents have been impressive in the management of severe PsA. However, patient selection and screening for latent tuberculosis are both important. Combined management by the dermatologist and rheumatologist is required for better patient care.
Acknowledgment
We sincerely appreciate the assistance of Dr. Kaleem Khan in the preparation of this manuscript.
| 1. |
Ritchlin CT, Kavanaugh A, Gladman DD, Mease PJ, Helliwell P, Boehncke WH, et al. Treatment recommendations for psoriatic arthritis. Ann Rheum Dis 2009;68:1387-94.
[Google Scholar]
|
| 2. |
Gladman DD. Mortality in psoriatic arthritis. Clin Exp Rheumatol 2008;26:S62-5.
[Google Scholar]
|
| 3. |
Buckley C, Cavill C, Taylor G, Kay H, Waldron N, Korendowych E, et al. Mortality in psoriatic arthritis-a single-center study from the UK. J Rheumatol 2010;37:2141-4.
[Google Scholar]
|
| 4. |
Gladman DD, Ang M, Su L, Tom BD, Schentag CT, Farewell VT. Cardiovascular morbidity in psoriatic arthritis. Ann Rheum Dis 2009;68:1131-5.
[Google Scholar]
|
| 5. |
Moll JM, Wright V. Psoriatic arthritis. Semin Arthritis Rheum 1973;3:55-78.
[Google Scholar]
|
| 6. |
Brent LH. Inflammatory arthritis: An overview for primary care physicians. Postgrad Med 2009;121:148-62.
[Google Scholar]
|
| 7. |
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H, et al. Classification criteria for psoriatic arthritis: Development of new criteria from a large international study. Arthritis Rheum 2006;54:2665-73.
[Google Scholar]
|
| 8. |
Helliwell PS, Taylor WJ. Classification and diagnostic criteria for psoriatic arthritis. Ann Rheum Dis 2005;64 Suppl 2:ii3-8.
[Google Scholar]
|
| 9. |
Helliwell PS, Porter G, Taylor WJ, CASPAR Study Group. Polyarticular psoriatic arthritis is more like oligoarticular psoriatic arthritis, than rheumatoid arthritis. Ann Rheum Dis 2007;66:113-7.
[Google Scholar]
|
| 10. |
Qureshi AA, Dominguez P, Duffin KC, Gladman DD, Helliwell P, Mease PJ, et al. Psoriatic arthritis screening tools. J Rheumatol 2008;35:1423-5.
[Google Scholar]
|
| 11. |
Maejima H, Taniguchi T, Watarai A, Katsuoka K. Evaluation of nail disease in psoriatic arthritis by using a modified nail psoriasis severity score index. Int J Dermatol 2010;49:901-6.
[Google Scholar]
|
| 12. |
Soscia E, Sirignano C, Catalano O, Atteno M, Costa L, Caso F, et al. New developments in magnetic resonance imaging of the nail unit. J Rheumatol Suppl 2012;89:49-53.
[Google Scholar]
|
| 13. |
Roberts ME, Wright V, Hill AG, Mehra AC. Psoriatic arthritis. Follow-up study. Ann Rheum Dis 1976;35:206-12.
[Google Scholar]
|
| 14. |
Bywaters EG, Dixon AS. Paravertebral ossification in psoriatic arthritis. Ann Rheum Dis 1965;24:313-31.
[Google Scholar]
|
| 15. |
De Simone C, Caldarola G, D′Agostino M, Carbone A, Guerriero C, Bonomo L, et al. Usefulness of ultrasound imaging in detecting psoriatic arthritis of fingers and toes in patients with psoriasis. Clin Dev Immunol 2011;2011:390726.
[Google Scholar]
|
| 16. |
Love TJ, Zhu Y, Zhang Y, Wall-Burns L, Ogdie A, Gelfand JM, et al. Obesity and the risk of psoriatic arthritis: A population-based study. Ann Rheum Dis 2012;71:1273-7.
[Google Scholar]
|
| 17. |
Gossec L, Smolen JS, Gaujoux-Viala C, Ash Z, Marzo-Ortega H, van der Heijde D, et al. European League Against Rheumatism recommendations for the management of psoriatic arthritis with pharmacological therapies. Ann Rheum Dis 2012;71:4-12.
[Google Scholar]
|
| 18. |
American Academy of Dermatology Work Group, Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 6. Guidelines of care for the treatment of psoriasis and psoriatic arthritis: Case-based presentations and evidence-based conclusions. J Am Acad Dermatol 2011;65:137-74.
[Google Scholar]
|
| 19. |
Kivitz AJ, Espinoza LR, Sherrer YR, Liu-Dumaw M, West CR. A comparison of the efficacy and safety of celecoxib 200 mg and celecoxib 400 mg once daily in treating the signs and symptoms of psoriatic arthritis. Semin Arthritis Rheum 2007;37:164-73.
[Google Scholar]
|
| 20. |
Sarzi-Puttini P, Santandrea S, Boccassini L, Panni B, Caruso I. The role of NSAIDs in psoriatic arthritis: Evidence from a controlled study with nimesulide. Clin Exp Rheumatol 2001;19:S17-20.
[Google Scholar]
|
| 21. |
Griffiths CE, Barker JN. Psoriasis. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook′s Textbook of Dermatology. 8 th ed. Singapore: Wiley-Blackwell; 2010. p. 20-48.
[Google Scholar]
|
| 22. |
Augustin M, Schäfer I, Reich K, Glaeske G, Radtke M. Systemic treatment with corticosteroids in psoriasis - Health care provision far beyond the S3-guidelines. J Dtsch Dermatol Ges 2011;9:833-8.
[Google Scholar]
|
| 23. |
Black RL, O′Brien WM, Vanscott EJ, Auerbach R, Eisen AZ, Bunim JJ. Methotrexate therapy in psoriatic arthritis; Double-blind study on 21 patients. JAMA 1964;189:743-7.
[Google Scholar]
|
| 24. |
Kragballe K, Zachariae E, Zachariae H. Methotrexate in psoriatic arthritis: A retrospective study. Acta Derm Venereol 1983;63:165-7.
[Google Scholar]
|
| 25. |
Espinoza LR, Zakraoui L, Espinoza CG, Gutiérrez F, Jara LJ, Silveira LH, et al. Psoriatic arthritis: Clinical response and side effects to methotrexate therapy. J Rheumatol 1992;19:872-7.
[Google Scholar]
|
| 26. |
Kingsley GH, Kowalczyk A, Taylor H, Ibrahim F, Packham JC, McHugh NJ, et al. A randomized placebo-controlled trial of methotrexate in psoriatic arthritis. Rheumatology (Oxford) 2012;51:1368-77.
[Google Scholar]
|
| 27. |
Baranauskaite A, Raffayová H, Kungurov NV, Kubanova A, Venalis A, Helmle L, et al. Infliximab plus methotrexate is superior to methotrexate alone in the treatment of psoriatic arthritis in methotrexate-naive patients: The RESPOND study. Ann Rheum Dis 2012;71:541-8.
[Google Scholar]
|
| 28. |
Kalb RE, Strober B, Weinstein G, Lebwohl M. Methotrexate and psoriasis: 2009 National Psoriasis Foundation Consensus Conference. J Am Acad Dermatol 2009;60:824-37.
[Google Scholar]
|
| 29. |
Lindsay K, Fraser AD, Layton A, Goodfield M, Gruss H, Gough A. Liver fibrosis in patients with psoriasis and psoriatic arthritis on long-term, high cumulative dose methotrexate therapy. Rheumatology (Oxford) 2009;48:569-72.
[Google Scholar]
|
| 30. |
Salvarani C, Macchioni P, Olivieri I, Marchesoni A, Cutolo M, Ferraccioli G, et al. A comparison of cyclosporine, sulfasalazine, and symptomatic therapy in the treatment of psoriatic arthritis. J Rheumatol 2001;28:2274-82.
[Google Scholar]
|
| 31. |
Kaltwasser JP, Nash P, Gladman D, Rosen CF, Behrens F, Jones P, et al. Efficacy and safety of leflunomide in the treatment of psoriatic arthritis and psoriasis: A multinational, double-blind, randomized, placebo-controlled clinical trial. Arthritis Rheum 2004;50:1939-50.
[Google Scholar]
|
| 32. |
Clegg DO, Reda DJ, Abdellatif M. Comparison of sulfasalazine and placebo for the treatment of axial and peripheral articular manifestations of the seronegative spondylarthropathies: A Department of Veterans Affairs cooperative study. Arthritis Rheum 1999;42:2325-9.
[Google Scholar]
|
| 33. |
Schräder P, Mooser G, Peter RU, Puhl W. Preliminary results in the therapy of psoriatic arthritis with mycophenolate mofetil. Z Rheumatol 2002;61:545-50.
[Google Scholar]
|
| 34. |
Lee JC, Gladman DD, Schentag CT, Cook RJ. The long-term use of azathioprine in patients with psoriatic arthritis. J Clin Rheumatol 2001;7:160-5.
[Google Scholar]
|
| 35. |
Carette S, Calin A, McCafferty JP, Wallin BA. A double-blind placebo-controlled study of auranofin in patients with psoriatic arthritis. Arthritis Rheum 1989;32:158-65.
[Google Scholar]
|
| 36. |
Palit J, Hill J, Capell HA, Carey J, Daunt SO, Cawley MI, et al. A multicentre double-blind comparison of auranofin, intramuscular gold thiomalate and placebo in patients with psoriatic arthritis. Br J Rheumatol 1990;29:280-3.
[Google Scholar]
|
| 37. |
Mease PJ, Kivitz AJ, Burch FX, Siegel EL, Cohen SB, Ory P, et al. Etanercept treatment of psoriatic arthritis: Safety, efficacy, and effect on disease progression. Arthritis Rheum 2004;50:2264-72.
[Google Scholar]
|
| 38. |
Antoni C, Krueger GG, de Vlam K, Birbara C, Beutler A, Guzzo C, et al. Infliximab improves signs and symptoms of psoriatic arthritis: Results of the IMPACT 2 trial. Ann Rheum Dis 2005;64:1150-7.
[Google Scholar]
|
| 39. |
Van der Heijde D, Kavanaugh A, Gladman DD, Antoni C, Krueger GG, Guzzo C, et al. Infliximab inhibits progression of radiographic damage in patients with active psoriatic arthritis through one year of treatment: Results from the induction and maintenance psoriatic arthritis clinical trial 2. Arthritis Rheum 2007;56:2698-707.
[Google Scholar]
|
| 40. |
Rheumatology Therapeutics: Drugs and Biologics. Available from: http://www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm105782.htm. [Accessed 2013 Feb 23].
[Google Scholar]
|
| 41. |
Mease P, Fleischmann R, Deodhar A, Wollenhaupt J, Kielar D, Woltering F, et al. Effect of certolizumab pegol on signs and symptoms in patients with psoriatic arthritis: 24 week results of a phase 3 double blinded randomized placebo-controlled study (RAPID-PsA). Ann Rheum Dis 2012;71:s150.
[Google Scholar]
|
| 42. |
Kavanaugh A, McInnes IB, Mease PJ, Krueger GG, Gladman DD, van der Heijde D, et al. Clinical efficacy, radiographic and safety findings through 2 years of golimumab treatment in patients with active psoriatic arthritis: Results from a long-term extension of the randomised, placebo-controlled GO-REVEAL study. Ann Rheum Dis 2012. [In Press]
[Google Scholar]
|
| 43. |
Fagerli KM, Lie E, van der Heijde D, Heiberg MS, Lexberg AS, Rødevand E, et al. The role of methotrexate co-medication in TNF-inhibitor treatment in patients with psoriatic arthritis: Results from 440 patients included in the NOR-DMARD study. Ann Rheum Dis 2013. [In Press]
[Google Scholar]
|
| 44. |
Hyrich KL, Lunt M, Dixon WG, Watson KD, Symmons DP, BSR Biologics Register. Effects of switching between anti-TNF therapies on HAQ response in patients who do not respond to their first anti-TNF drug. Rheumatology (Oxford) 2008;47:1000-5.
[Google Scholar]
|
| 45. |
Korman BD, Tyler KL, Korman NJ. Progressive multifocal leukoencephalopathy, efalizumab, and immunosuppression: A cautionary tale for dermatologists. Arch Dermatol 2009;145:937-42.
[Google Scholar]
|
| 46. |
Wu Y, Chen J, Li YH, Ma GZ, Chen JZ, Gao XH, et al. Treatment of psoriasis with interleukin-12/23 monoclonal antibody: A systematic review. Eur J Dermatol 2012;22:72-82.
[Google Scholar]
|
| 47. |
Mease PJ, Reich K, Alefacept in Psoriatic Arthritis Study Group. Alefacept with methotrexate for treatment of psoriatic arthritis: Open-label extension of a randomized, double-blind, placebo-controlled study. J Am Acad Dermatol 2009;60:402-11.
[Google Scholar]
|
| 48. |
Smolen JS, Beaulieu A, Rubbert-Roth A, Ramos-Remus C, Rovensky J, Alecock E, et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): A double-blind, placebo-controlled, randomised trial. Lancet 2008;371:987-97.
[Google Scholar]
|
| 49. |
Nordgaard-Lassen I, Dahlerup JF, Belard E, Gerstoft J, Kjeldsen J, Kragballe K, et al. Guidelines for screening, prophylaxis and critical information prior to initiating anti-TNF-alpha treatment. Dan Med J 2012;59:C4480.
[Google Scholar]
|
Fulltext Views
8,391
PDF downloads
2,117





