Translate this page into:
Diagnosis of subclinical extramammary Paget’s disease with a combination of noninvasive photodynamic diagnosis and reflectance confocal microscopy
Corresponding author: Dr. Minzhi Wu, Department of Dermatology, The Fifth People’s Hospital of Suzhou, The Affiliated Hospital of Infectious Diseases of Soochow University, Suzhou 215131, Jiangsu Province, China. 44276276@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Huang L, Wang Y, Wu M, Zhao J, Zhang W, Zhao L, et al. Diagnosis of subclinical extramammary Paget's disease with a combination of noninvasive photodynamic diagnosis and reflectance confocal microscopy. Indian J Dermatol Venereol Leprol 2021;87:371-4.
Abstract
Extramammary Paget’s disease is a rare skin malignancy, and its diagnosis requires invasive biopsy and histopathological examination. Surgery is the standard treatment for extramammary Paget’s disease patients; however, as incision boundaries and the depth of tumor cell infiltration are often unclear, the postoperative recurrence rate is high. We present a case in which we used photodynamic diagnosis in combination with reflectance confocal microscopy before surgery to detect an extramammary Paget’s disease lesion that was located 3 cm away from the classical lesion. This secondary lesion exhibited a subclinical presentation, and it was eventually confirmed as an extramammary Paget’s disease lesion by pathological examination. During detection using our technique, we delineated the boundaries of the extramammary Paget’s disease lesion as a guide for surgical excision. The findings of our case demonstrate that photodynamic diagnosis combined with reflectance confocal microscopy can be used for the noninvasive diagnosis of subclinical extramammary Paget’s disease and may be used to guide strategies for planning treatment and preventing relapse.
Keywords
Extramammary
Paget’s disease
photodynamic diagnosis
reflectance confocal microscopy
Introduction
Extramammary Paget’s disease is a rare skin tumor that presents as eczema-like lesions, involving the apocrine sweat glands of the scrotum, penis, labia majora, labia minora and vaginal orifice.1 These tumors often exhibit indistinct boundaries, irregular plaques, erosion, ulceration, exudation, desquamation and scabs. Wide local excision is the standard treatment for extramammary Paget’s disease.2 Owing to the indistinct boundaries and unclear infiltration depth of tumor cells, surgical outcomes are often unsatisfactory with relapse rates as high as 20–60%.3 Here, we present a case in which we used photodynamic diagnosis in combination with reflectance confocal microscopy to detect a subclinical extramammary Paget’s disease lesion.
Case Report
A 64-year-old man with a 3-year history of erythema and itching in the genital region was hospitalized for further evaluation of ulceration and exudation after scratching. The area of erythema gradually increased from 1 × 1cm to 9 × 6cm. After scratching, the surface became ulcerated with exudation, and growths appeared in the center of the lesion.
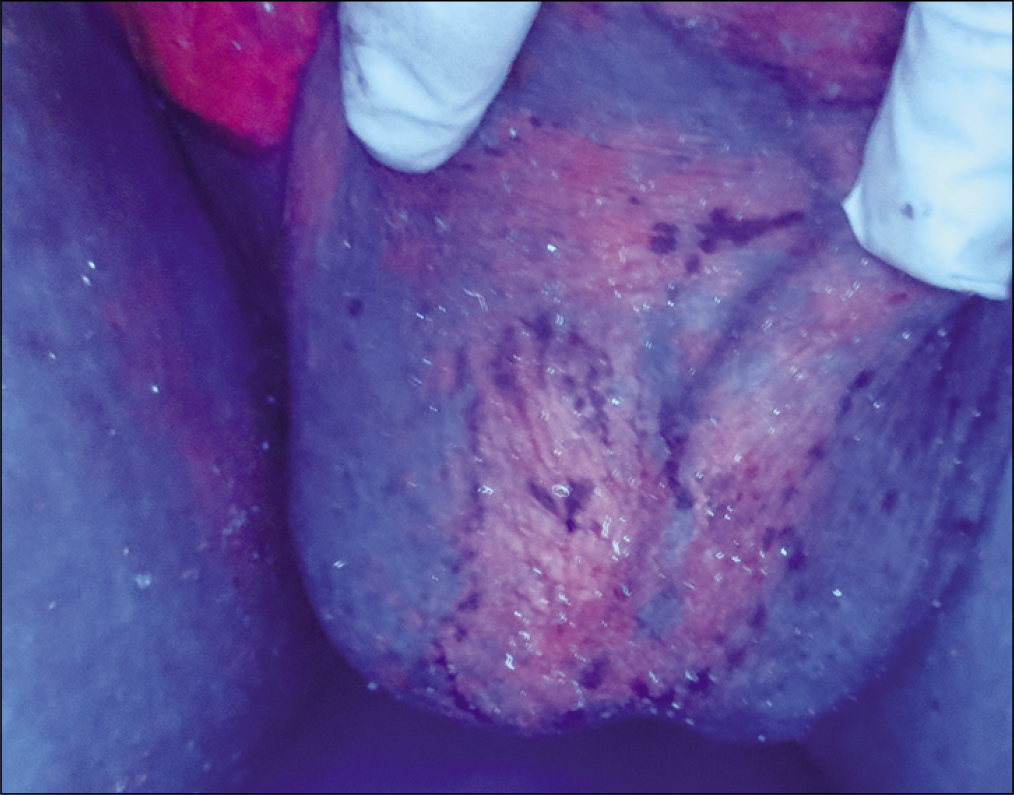
Dermatological examination showed a 10 × 8 cm infiltrative erythema in the right mons pubis, groin, upper scrotum and root of the penis. The center of the lesion had an irregular, elevated red mass with indistinct boundaries and surface erosion, accompanied by slight mucous secretion. No apparent abnormalities were seen in the external genital and perianal regions [Figure 1].

- Infiltrative erythema (10 × 8 cm) on the right mons pubis, groin, upper scrotum and root of the penis
The patient underwent biopsy and microscopic pathological examination revealed hyperkeratosis accompanied by parakeratosis, pseudoepitheliomatous hyperplasia of the epidermis and Paget-like cells (arranged singly or in nests) throughout the epidermis layer. The cells were round with large cell bodies and lightly stained cytoplasm. Some tumor cells infiltrated the hair follicles and sweat ducts and entered the deep dermis at the level of the sweat glands. Immunohistochemical analysis indicated negativity for CK20 (cytokeratin 20), CK5/6 (cytokeratin 5/6), gross cystic disease fluid protein (GCDFP15) and Melan-A, but the tissue showed positivity for CK7 (cytokeratin 7), EMA (epithelial membrane antigen), CEA (carcinoembryonic antigen) and Her-2. Thus, a pathological diagnosis of extramammary Paget’s disease with infiltrative growth into the dermis along the appendages was made.
Supplementary blood, urine and stool examination results were normal and revealed negativity for liver inflammatory markers, venereal disease markers, alpha-fetoprotein and carcinoembryonic antigen. Color ultrasound indicated no apparent abnormalities in the liver, gallbladder, bile duct, pancreas, spleen, kidneys, ureters or bladder. Multiple enlarged lymph nodes were observed on both sides of the groin with the largest being 2.335 × 2.062 × 0.797cm. These lymph nodes were oval with a clear corticomedullary structure and no internal blood flow signal.
On hospitalization, his pubic hair was removed and 3% boric acid solution was applied onto the skin lesion and then zinc oxide was applied topically thrice a day. After 2 days, surface exudation from the lesion disappeared and the erythema alleviated. We performed photodynamic diagnosis in combination with reflectance confocal microscopy using a Vivascope 1500 (wavelength 830nm) confocal microscope (Lucid Inc., Rochester, NY, USA) to determine the boundaries of the skin lesion to guide intraoperative excision.
Aminolevulinic acid hydrochloride (20% in physiological saline) was applied with a thin layer of cotton over the skin lesion and a 5-cm boundary around the lesion. After 3 h, Wood’s lamp was used to visualize the extent of the skin lesion. During labeling, we incidentally found a 3 × 2cm brick-red region with a slightly weaker fluorescence intensity in the middle and lower scrotum 3 cm away from the main lesion [Figure 2]. Gross re-examination did not reveal any apparent abnormalities in this region [Figure 3]. Reflectance confocal microscopy showed a disordered epidermal structure, vacuolar cells between keratinocytes, highly refractive dendritic cells at the basal layer, dermal capillary tortuosity and infiltration of large amounts of inflammatory cells, indicating extramammary Paget’s disease [Figure 4].
- Brick-red region (3 × 2 cm) in the middle and lower scrotum with slightly weaker fluorescence intensity, under Wood’s lamp, after application of aminolevulinic acid

- No apparent abnormalities in the weakly fluorescent area and surrounding nonfluorescent area on gross re-examination
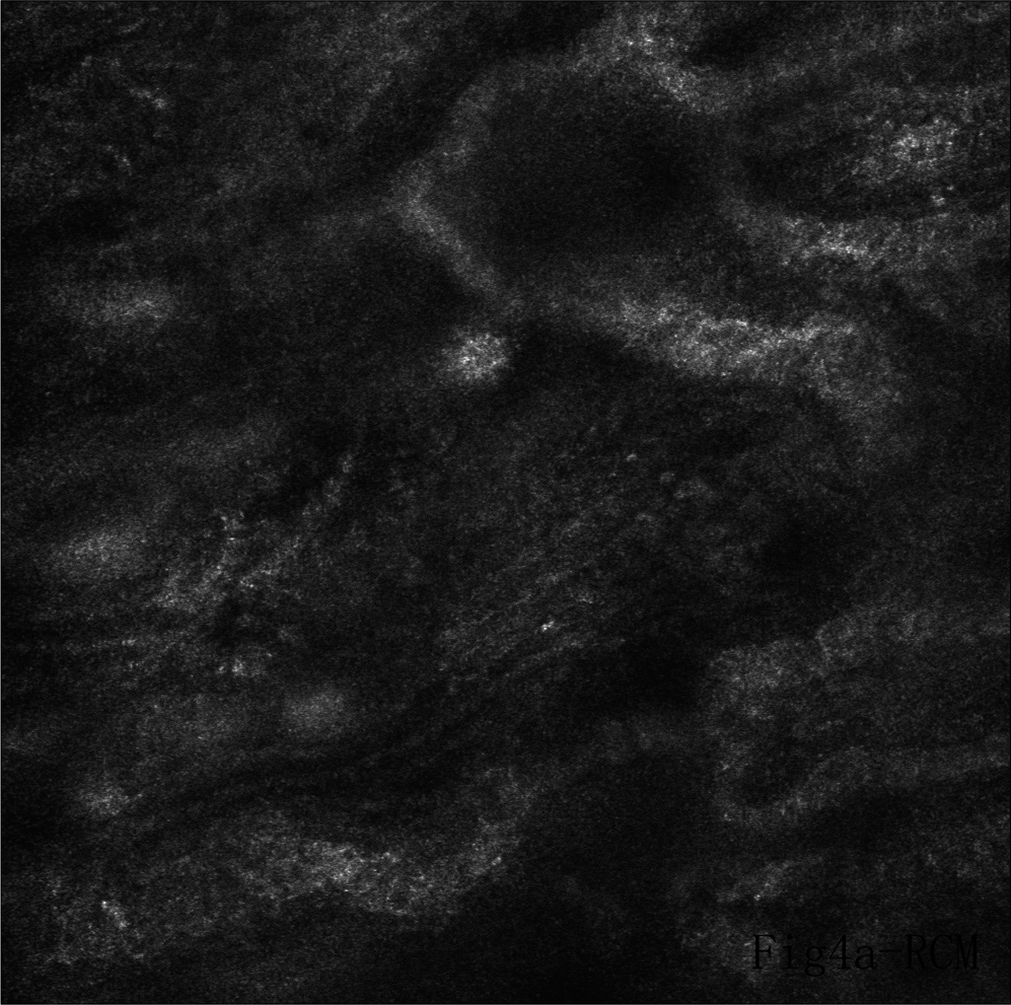
- Weakly fluorescent region on reflectance confocal microscopy with various findings indicative of extramammary Paget’s disease
After obtaining written informed consent, spinal anesthesia was administered. The skin lesion and weakly fluorescent region were excised, and skin flap repair was performed. The largest lymph node was biopsied. No tumor cells were observed in the lymph node. Pathological examination of the weakly fluorescent region showed several scattered or cluster-like Paget cells at the epidermis [Figure 5a and b]. Immunohistochemical analysis of the lesion revealed CK7 and EMA positivity [Figures 6 and 7].
![Several scattered or cluster like Paget cells in the weakly fluorescent region [hematoxylin and eosin (H & E), ×20]](/content/126/2021/87/3/img/IJDVL-87-371-g005.png)
- Several scattered or cluster like Paget cells in the weakly fluorescent region [hematoxylin and eosin (H & E), ×20]
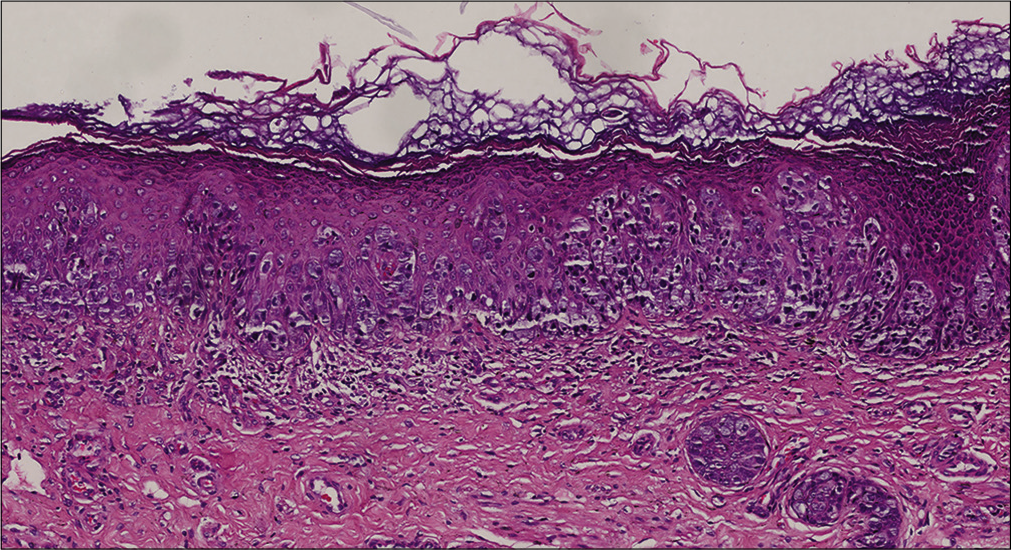
- Several scattered or cluster like Paget cells in the weakly fluorescent region (H & E, ×200)
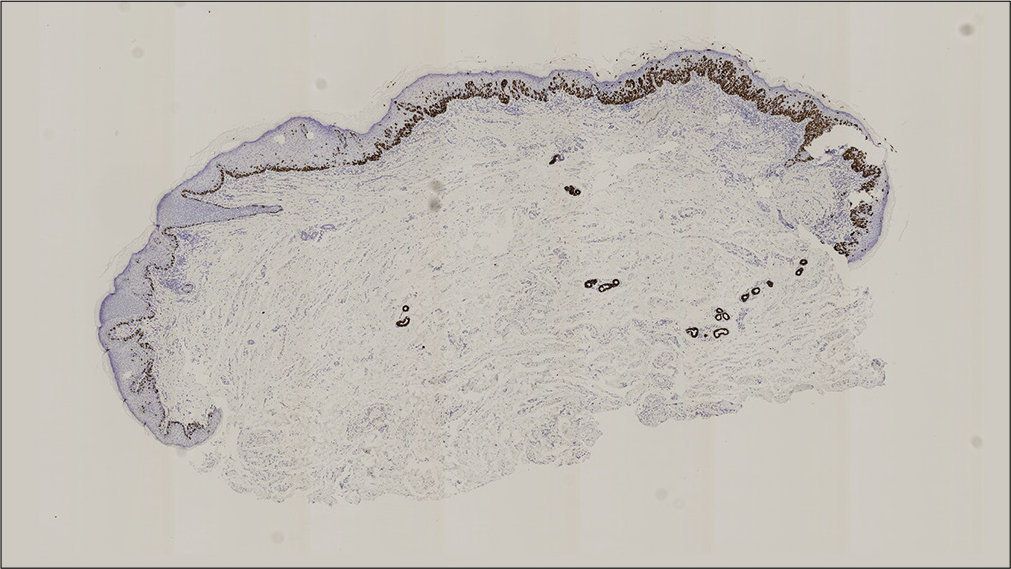
- CK7 positive lesion on immunohistochemical analysis (×20)
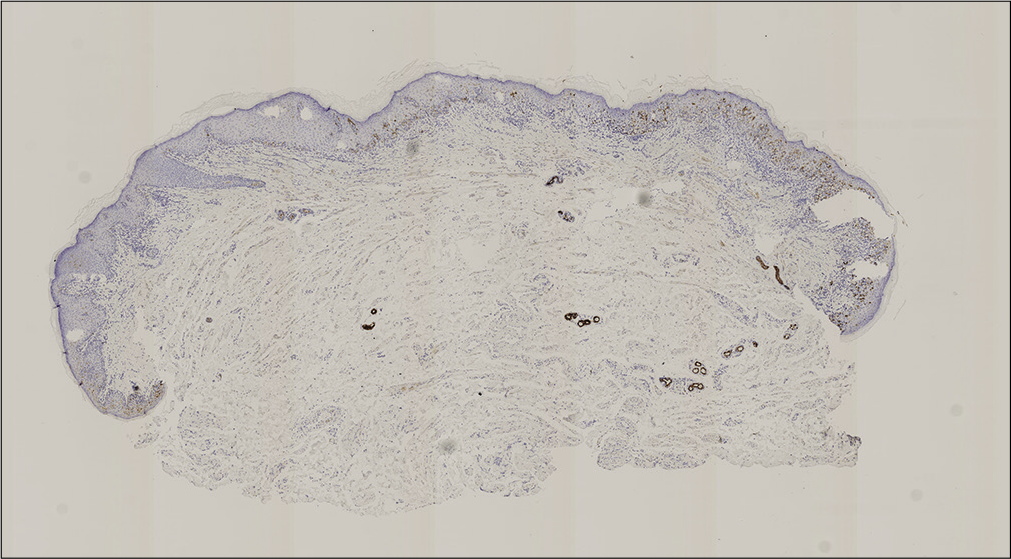
- EMA positive lesion on immunohistochemical analysis (×20)
Discussion
Photodynamic fluorescence uses photosensitizers which are absorbed by target cells and metabolized to porphyrin. Under illumination with a specific wavelength of light, fluorescence will indicate a clear boundary between normal and lesional skin.4 Using this technique, extramammary Paget’s disease will be characterized by highly refractive, large-nucleated cells on the epidermis under reflectance confocal microscopy.
Particularly, pathological cells are at least twice the size of normal keratinocytes and exhibit moderate nuclear brightness and a less refractive cytoplasm. Mitotic dendritic cells can be observed in high refraction zones. Guitera et al. assessed reflectance confocal microscopy images and histopathological images of nine extramammary Paget’s disease patients and one mammary patient.5 They found that reflectance confocal microscopy was not only important in extramammary Paget’s disease diagnosis but also useful for preoperative labeling of the tumor boundary to help guide surgeons during surgery.5 Yélamos et al. found that handheld reflectance confocal microscopy was a useful auxiliary tool for diagnosing extramammary Paget’s disease recurrence and guiding scouting biopsies, thus reducing the number of biopsies needed for a correct diagnosis.6 Pan et al.found that the features observed on reflectance confocal microscopy of extramammary Paget’s disease lesions correlated well with their histopathologic findings.7 Reflectance confocal microscopy may be used as an auxiliary diagnostic tool for the diagnosis and management of extramammary Paget’s disease. However, because of the physical structural constraints of reflectance confocal microscopy and the limitation of a small field of view of the lens, comprehensive examination of uneven regions, as well as the scrotal region is currently difficult owing to skin folds, large extensions and skin shrinkage.We suggest that photodynamic diagnosis, associated with reflectance confocal microscopy, could be used as a supplementary method for screening. Dermoscopy has been reported to facilitate the diagnosis of extramammary Paget’s disease; however, subclinical extramammary Paget’s disease skin lesions are rarely detected.8,9
In the present case, although the secondary region exhibited weak fluorescence, reflectance confocal microscopy suggested extramammary Paget’s disease; thus, the region was excised. Pathological examination confirmed extramammary Paget’s disease. Clinically, the identification of subclinical extramammary Paget’s disease skin lesions away from classical extramammary Paget’s disease skin lesions using photodynamic diagnosis is rare. The application of photodynamic diagnosis to a 5-cm boundary of a classical clinical extramammary Paget’s disease lesion is recommended to rule out subclinical lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Scientific Research Project of Jiangsu Commission of Health (BJ16007) Supported by the Fundamental Research Funds for the Central Universities (2016RC320006). The Introduction Project of Clinical Expert Team in Suzhou (SZYJTD201811).
Conflicts of interest
There are no conflicts of interest.
References
- Paget's disease of the vulva: Pathology, pattern of involvement, and prognosis. Gynecol Oncol. 2000;77:183-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of extramammary Paget disease of the vulva with imiquimod: A retrospective, multicenter study by the German colposcopy network. J Am Acad Dermatol. 2014;70:644-50.
- [CrossRef] [PubMed] [Google Scholar]
- Extramammary Paget's disease: Surgical treatment with Mohs micrographic surgery. J Am Acad Dermatol. 2004;51:767-73.
- [CrossRef] [PubMed] [Google Scholar]
- Complete remission of two patients with recurrent and wide spread extramammary Paget disease obtained from 5 aminolevulinic acid based photodynamic therapy and imiquimod combination treatment. Photodiagnosis Photodyn Ther2014;. ;11:434-40.
- [CrossRef] [PubMed] [Google Scholar]
- Reflectance confocal microscopy for diagnosis of mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol. 2013;27:e24-9.
- [CrossRef] [PubMed] [Google Scholar]
- Handheld reflectance confocal microscopy for the detection of recurrent extramammary Paget disease. JAMA Dermatol. 2017;153:689-93.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo reflectance confocal microscopy of extramammary Paget disease: Diagnostic evaluation and surgical management. J Am Acad Dermatol. 2012;66:e47-53.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and dermoscopic characteristics of extramammary Paget disease: A study of 35 cases. Br J Dermatol. 2016;174:1104-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscope guided lesional biopsy to diagnose EMA+ CK7+ CK20+ extramammary Paget's disease with an extensive lesion. J Eur Acad Dermatol Venereol. 2018;32:e92-4.
- [CrossRef] [PubMed] [Google Scholar]






