Translate this page into:
Disseminated blastomycosis in a child with a brief review of the Indian literature
2 Department of Radiology, Maharajah's Institute of Medical Sciences (MIMS), Nellimarla, Vizianagaram, India
3 Department of Neurology, Andhra Medical College, Visakhapatnam, Andhra Pradesh, India
Correspondence Address:
G Raghurama Rao
Department of Dermatology, Surya Skin Care and Research Center, # 15-1-2, Gopal Sadan, Naoroji Road, Maharanipeta, Visakhapatnam - 530 002, Andhra Pradesh
India
| How to cite this article: Rao G R, Narayan BL, Durga Prasad B K, Amareswar A, Sridevi M, Raju B. Disseminated blastomycosis in a child with a brief review of the Indian literature. Indian J Dermatol Venereol Leprol 2013;79:92-96 |
Abstract
Disseminated blastomycosis is rare in India, particularly in the pediatric population. We discuss the clinical picture, progress and outcome of disseminated blastomycosis in a 4-year-old child. We also present a brief review of the literature focussing on the scenario of blastomycosis in India.Introduction
Blastomycosis is rare in India, and is caused by Blastomyces dermatitidis. It was commonly known as North American blastomycosis, and was initially thought to be restricted to North America, but, more recently, cases have been reported from all over the world, including India. It was first described by Gilchirst in 1894. All age groups are susceptible to blastomycosis, but majority of the patients are in the age group of 20-70 years. Three percent to 11% of the reported cases are less than 20 years of age. [1] There are three clinical forms of the disease: pulmonary, disseminated and primary cutaneous blastomycosis. Cutaneous blastomycosis is almost always secondary to lung involvement, and primary forms are very rare.
We report a rare and first case of disseminated blastomycosis from Andhra Pradesh, and we also discuss the Indian scenario of blastomycosis.
Case Report
A 4-year-old boy presented with a 6-month history of multiple, hyperkeratotic, suppurating plaques and nodules over the face, chest, back and upper and lower extremities, with a huge intraocular flesh-colored mass in the left eye. The boy was from a rural area and from the low socioeconomic strata. To start with, he had cough with fever, followed by a plaque over the right cheek with cervical lymphadenopathy. He was examined by a local pediatrician. Chest radiograph revealed patchy consolidation of the upper lobes of the right lung. Fine needle aspiration cytology (FNAC) of the cervical lymph nodes showed non-specific lymphadenitis, and anti-tuberculosis treatment (ATT) was given. While the child was on ATT, he started developing multiple cutaneous lesions, nasal stuffiness causing airway obstruction and a large mass in the left eye causing proptosis. On the day of presentation, the child′s general condition was good. His anthropometric measurements were height 100 cm and weight 10 kg. All vital signs were within normal limits. There were multiple, hyperkeratotic plaques of varying sizes on the face, chest and back and some suppurating plaques on the neck. In addition, there were multiple umbilicated papules and nodules over the extremities. There was a huge flesh-colored mass protruding from the left eye [Figure - 1]a and b. There was generalized lymphadenopathy and no organomegaly, and all other systems were normal. There was an airway obstruction and the case was referred to an ENT specialist and ophthalmologist for further examination. There was a pinkish mass in the left nostril with mucoid discharge. Detailed ophthalmic examination revealed normal vision in the right eye (6/6). The left eye had finger counting at 2 meters with mild ptosis and proptosis with a mass on the supero-temporal quadrant of the orbit showing a clear demarcation from the orbital rim. Fundus examination of both eyes revealed no abnormal changes. In view of the clinical features, a chronic granulomatous etiology was suspected and the case was thoroughly evaluated.
 |
| Figure 1: (a) Multiple verrucous plaques with protruding ocular mass. (b) Multiple umbilicated lesions on the back |
Hemogram revealed a low hemoglobin of 8.5 gm/dL, leukocytosis 24, 420/mm 3 , neutrophils 23%, lymphocytes 40%, eosinophils 33%, monocytes 3%, basophils 1%, platelet count 150,000/mm3 and high erythrocyte sedimentation rate 64 mm/h. No abnormal cells were detected in the peripheral smear. All relevant biochemical tests were normal. Enzyme-linked immunosorbent assay for human immunodeficiency virus (HIV) and Venereal Disease Research Laboratory tests were non-reactive. Anti-nuclear antibody (ANA) test and Mantoux test were negative. Radiograph of the chest revealed fibrotic infiltrates in the right upper lobe. FNAC from the right cervical lymph node was suggestive of chronic non-specific lymphadenitis, but no organisms were detected. Contrast computerized tomography of the orbits revealed extraconal mass lesion involving the left orbit with proptosis and no bony involvement, with diffuse mucosal thickening of the nasal cavities [Figure - 2]a and b. Radiograph of the long bones of both upper and lower extremities was normal. Ultrasound abdomen revealed mild hepatomegaly. Smears from the suppurative lesions revealed no acid fast bacilli and no fungal elements. Two elliptical biopsies were taken from the skin lesions, one for identification and culture of the organism and the other for histopathological examination. The suppurative fluid and a portion of curettage tissue (skin biopsy specimen) were cultured on Sabouraud dextrose agar containing chloramphenicol. They were incubated at room temperature (25-28°C) and were regularly observed for fungal growth. After 4 weeks of incubation, no colonies were identified. Histopathology of the skin specimen showed nodular granulomatous infiltrate of lymphocytes, plasma cells and giant cells involving the whole of the dermis. Gramuloma was poorly defined, and extends into the interstitium of the reticlular dermis. Scattered within the granuloma were several fungal broad-based budding yeast cells within the giant cells. Periodic acid Schiff (PAS) stain was positive [Figure - 3] and [Figure - 4]. In light of the clinical features and histopathological findings, a diagnosis of disseminated cutaneous blastomycosis was made and oral itraconazole 100 mg daily was started with supportive therapy. After 2 months of itraconazole therapy, majority of the skin lesions regressed and the intraocular mass also reduced in size with improvement of airway. During the third month of itraconazole therapy, the patient developed painful swellings of elbows and knees with a considerable functional disability. Radiograph of both knees and elbows revealed creeping type of periosteal reaction, which was suggestive of fungal etiology [Figure - 5]a and b. Considering the bone involvement and progress of the disease, we wanted to shift the patient from itraconazole to amphotericin B therapy. But, the family′s affordability factor was responsible for continuing itraconazole. After 2 months, the joint symptoms improved. While the patient was on itraconazole therapy for nearly 6 months, he developed severe headache with vomiting. The case was referred to a neurophysician and the child was hospitalized. The child was irritable, conscious with decreased comprehension and was able to move all the four limbs equally with bilateral plantar extensors. Fundus examination revealed blurring of the disc margins and magnetic resonance imaging of the brain showed obstructive hydrocephalus. Cerebrospinal fluid analysis revealed high protein (600 mg/dL) with normal cell count and no acid fast bacilli and fungal elements were isolated. In view of the deteriorating clinical picture with HIV non-reactive status, we suspected idiopathic CD4+ lymphocytopenia (ICL), and CD4 and CD8 counts were performed. His CD4 count was 152, CD8 168 and CD4/CD8 ratio 0.9. The patient was administered injection dexamethasone 2 cc i.v. three-times daily and amphotericin B initially 0.25 mg infusion for 2 days as a test dose followed by 0.5 mg. The dose was gradually increased to 1 mg over a period of 5 days. The patient did not respond. His general condition gradually deteriorated and he succumbed to death.
 |
| Figure 2: (a) Extraconal mass lesion of the left orbit. (b) Intact bony cortex with diffuse thickening of the nasal cavities |
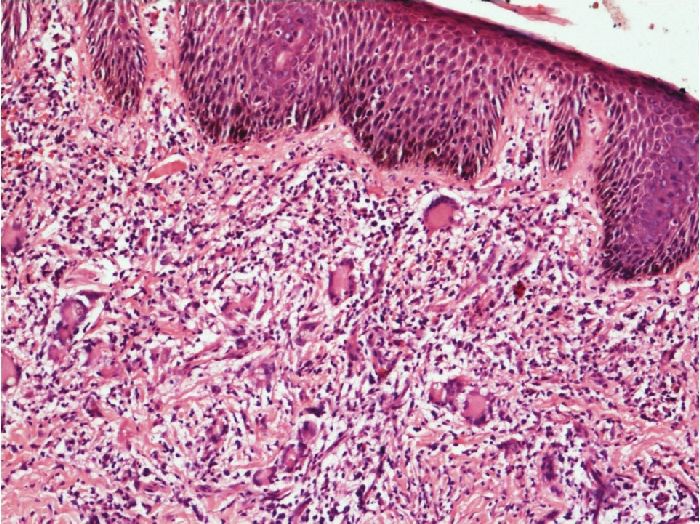 |
| Figure 3: The epidermis is mildly hyperplastic. The dermis shows a granulomatous inflammation with histiocytes and giant cells (H and E, X40) |
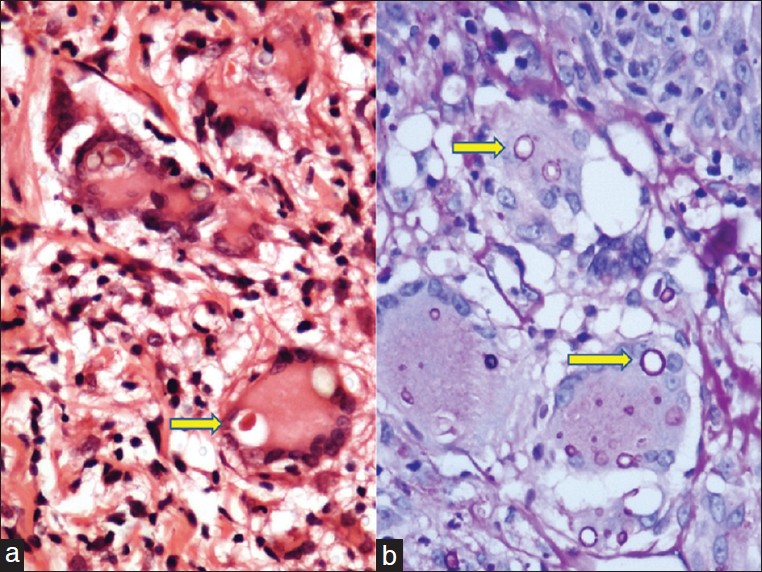 |
| Figure 4: Composite picture at high-power view showing the fungal yeast forms within the giant cells, highlighted by the Periodic acid Schiff (PAS) positive fungal wall in the right panel (H and E, X400 (a); PAS X400 (b)) |
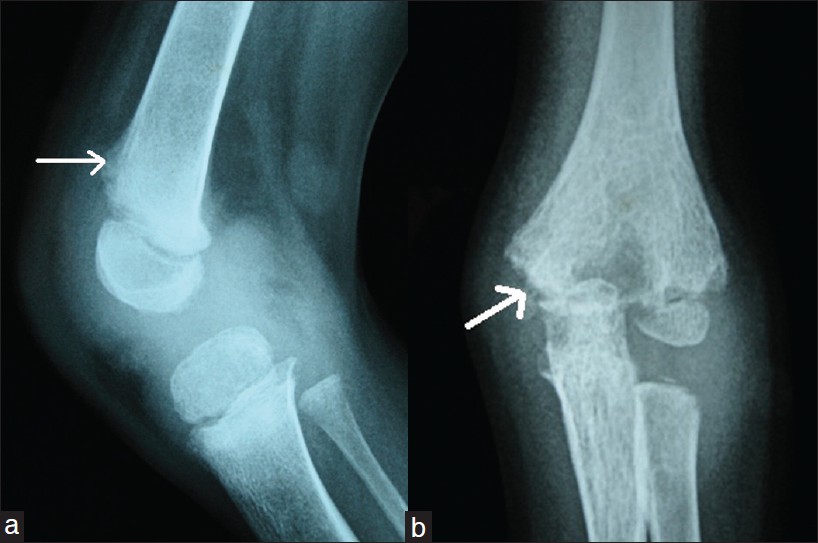 |
| Figure 5: (a) Lateral radiograph of the knee showing joint effusion with creeping type of periosteal reaction involving the distal end of the femur. (b) Destructive lesions seen involving the elbow joint with joint effusion |
Discussion
Blastomycosis is a relatively uncommon chronic granulomatous disease even in endemic regions, more so in India. It is typically caused by inhalation of conidia of the dimorphic fungus Blastomyces dermatitidis, although direct inoculation has been known to occur. Skin is the most frequent site (40-80%) of dissemination of pulmonary blastomycosis, followed by bone (10-50%), genitourinary tract (10-30%) and central nervous system (1-5%). The mortality is very high with central nervous system (CNS) involvement. [2],[3] In some cases, the primary pulmonary focus may resolve before the dissemination of the disease to the skin and other organs, as in the present case. Disseminated blastomycosis with ocular involvement is rare. There are no eye findings specific for ophthalmic blastomycosis. Uveitis is the most common clinical finding and panophthalmitis is also reported. [4] In our case, there was a huge intraocular mass without symptoms of uveitis or panophthalmitis.
Blastomycosis is rarely diagnosed in children. In children, lung involvement is followed by that of the skin, bone and CNS in descending order of incidence. [5] In this case also, the child initially had a brief pulmonary illness followed by cutaneous lesions, lymphadenopathy and involvement of the bone and CNS. Because of delayed diagnosis, generally, children present with more advanced disease. To the best of our knowledge, this is the first case of disseminated blastomycosis from India in the pediatric age group.
The diagnosis of blastomycosis may be confirmed through the identification of yeasts of Blastomyces dermatitidis in body fluids and tissues. Although culture is the gold standard method for detecting fungus, it is positive in only 3.2% of the patients. [3] Even in the absence of positive culture, the case can be diagnosed by histopathological examination and FNAC of the lesions. [1] Yeast forms can be seen in hematoxylin and eosin-stained sections, but are better visualized with methenamine silver stain or PAS stain. Differentiation from other deep fungal infections showing similar histopathological features include chromoblastomycosis, coccidioidomycosis, paracoccidioidomycosis and histoplasmosis. Absence of pigment and presence of characteristic multinucleate yeast forms with single broad-based buds are suggestive of blastomycosis. [1] Skin tests and serology are of little benefit in the diagnosis of Blastomyces dermatitidis infections. Both have shown low sensitivity in detecting infection. [2] Our case was diagnosed on the basis of clinical features, histopathological findings, progress of the disease and partial response to itraconazole.
Most early literature did not consider blastomycosis as an opportunistic infection among immunocompromised patients. However, Lemos and colleagues [6] recently found that 25% of the patients with blastomycosis had preceding immunosuppressive conditions like diabetes mellitus, HIV and malignancies. [6] The clinical manifestations of disease in these patients are more severe. Although there were no underlying immunosuppressive conditions like diabetes, HIV and malignancy in our case, still, the patient did not respond to continuous itraconazole therapy and finally succumbed to death due to CNS involvement. These events prompted us to suspect a rare condition of idiopathic CD4+ lymphocytopenia (ICL) as the cause of underlying immunosuppression. The mandatory criteria for the diagnosis of ICL includes low numbers of CD4+ lymphocytes (<300) on two or more measurements over at least 6 weeks. [7] But, in our case, we had only one report of CD4 with 152 cells at the time of CNS involvement, and his previous CD4 and CD8 tests had not been performed. Although ICL is not established with certainty in this child, we presume that it may be a cause for rapid progress of the disease. Recently, a case of refractory cryptococcal meningitis with ICL in a 50-year-old man and another two cases of ICL in children were reported in the Indian literature. [8],[9] Although ICL is rare, it merits clinical suspicion in non-immunodeficient patients presenting with deep mycotic infections and other opportunistic infections.
Blastomycosis in India had been unknown until 1982, when Khan isolated Blastomyces dermatitidis from the lungs of a bat captured from abandoned parts of a school building in Delhi. [10] Before 1982, nine cases were reported with inadequate documentation. [11] In 1983, Randhawa et al. reported the first case of blastomycosis isolated from bronchial aspiration of a female patient from Uttar Pradesh. [12] Savio et al.[13] reviewed 13 cases of blastomycosis published during the period from 1983 to 1997 from different parts of India. Of these 13 cases, eight were human cases and five were case reports of blastomycosis in animals including bat, bird droppings, cattle, dog and monkey. In the eight human case reports, there was no mention of travel outside India and thus the infection was claimed to be acquired in India. In the same article, the authors published a case of blastomycosis in a south Indian patient after visiting an endemic area in the USA. Bumb et al.,[14] in 1996, reported localized cutaneous blastomycosis on the basis of KOH mount and histopathology. They successfully treated the case with fluconazole. In 1997, Gharpuray et al.[15] reported localized blastomycosis on clinical grounds without laboratory evidence. They treated this case with ketoconazole. A case of cutaneous blastomycosis presenting as non-healing ulcer and responding to oral ketoconazole was reported from Mangalore in 2003. [16] Chander et al.[17] reported a rare case of cerebral blastomycosis presented as meningioma in a 23-year-old female in 2007. To the best of our knowledge, only one case of pediatric cutaneous blastomycosis in an 8-year-old boy presenting with a 2-year history of multiple, hyperkeratotic, verrucous plaques and nodules was reported from Delhi. The authors successfully confirmed the case on FNAC and treated him with oral itraconazole. [1]
Although a few autochthonous cases of blastomyosis in humans and animals have been reported from various parts of the country, mostly from northern India, a vast majority of these infections remain undiagnosed. A high index of clinical suspicion and good mycological diagnostic services are needed to recognize these infections early to prevent further complications.
Acknowledgments
The authors acknowledge Dr. Uday Khopkar of Mumbai, Dr. Swarnalatha from Apollo Hospital (Hyderabad) and Dr. Madan from Visakha Medical Center (Visakhapatnam) for reviewing the histopathological slides and for their valuable opinions.
| 1. |
Shukla S, Singh S, Jain M, Kumar Singh S, Chander R, Kawatra N. Paediatric cutaneous blastomycosis: A rare case diagnosed on FNAC. Diagn Cytopathol 2009;37:119-21.
[Google Scholar]
|
| 2. |
Mason AR, Cortes GY, Cook J, Maize JC, Thiers BH. Cutaneous blastomycosis: A diagnostic challenge. Int J Dermatol 2008;
[Google Scholar]
|
| 3. |
Lemos LB, Guo M, Baliga M. Blastomycosis: Organ involvement and etiologic diagnosis. A review of 123 patients from Mississipi. Ann Diagn Pathol 2000;4:391-406.
[Google Scholar]
|
| 4. |
Lopez R, Mason JO, Parker JS, Pappas PG. Intraocular blastomycosis: Case report and review. Clin Infect Dis 1994;18:805-7.
[Google Scholar]
|
| 5. |
Garvey K, Hinshaw M, Vanness E. Chronic disseminated cutaneous blastomycosis in an 11-year old, with a brief review of the literature. Pediatr Dermatol 2006;23:541-5.
[Google Scholar]
|
| 6. |
Lemos LB, Baliga M, Guo M. Blastomycosis: The great pretender can also be an opportunist. Initial clinical diagnosis and underlying diseases in 123 patients. Ann Diagn Pathol 2002;6:194-203.
[Google Scholar]
|
| 7. |
McKinnell JA, Pappas PG. Blastomycosis: New insights into diagnosis, prevention, and treatment. Clin Chest Med 2009;30:227-39.
[Google Scholar]
|
| 8. |
Sharma A, Lal V, Modi M, Khurana D, Bal S, Prabhakar S. Idiopathic CD4 lymphocytopenia presenting as refractory cryptococcal meningitis. Ann Indian Acad Neurol 2010;13:136-8.
[Google Scholar]
|
| 9. |
Mukherjee A, Lodha R, Kabra SK. Idiopathic CD4+ T-cell lymphocytopenia. Indian J Pediatr 2009;76:430-2.
[Google Scholar]
|
| 10. |
Khan ZU, Randhawa HS, Lulla M. Isolation of Blastomyces dermatitidis from the lungs of a bat, Rhinopoma hardwickei hardwickei Gray, in Delhi. Sabouraudia 1982;20:137-44.
[Google Scholar]
|
| 11. |
Randhawa HS, Sandhu RS, Viswanathan R. Medical mycology in India-a review of the work done since 1910. Indian J Chest Dis 1961;3:33-49.
[Google Scholar]
|
| 12. |
Randhawa HS, Khan ZU, Gaur SN. Blastomyces dermatitidis in India: First report of its isolation from clinical material. Sabouraudia 1983;21:215-21.
[Google Scholar]
|
| 13. |
Savio J, Muralidharan S, Macaden RS, D'Souza G, Mysore S, Ramachandran P, et al. Blastomycosis in a South Indian patient after visiting an endemic area in USA. Med Mycol 2006;44:523-9.
et al. Blastomycosis in a South Indian patient after visiting an endemic area in USA. Med Mycol 2006;44:523-9.'>[Google Scholar]
|
| 14. |
Bumb RA, Mehta RD, Kumar K, Saini S. Localised cutaneous blastomycosis: Response to fluconazole. Indian J Dermatol Venereol Leprol 1996;62:120-1.
[Google Scholar]
|
| 15. |
Gharpuray MB, Mahajan PM, Tolat SN. Localised cutaneous blastomycosis. Indian J Dermatol Venereol Leprol 1997;63:243-5.
[Google Scholar]
|
| 16. |
Balasaraswathy P, Theerthanath. Cutaneous blastomycosis presenting as non-healing ulcer and responding to oral ketoconazole. Dermatol Online J 2003;9:19.
[Google Scholar]
|
| 17. |
Chander B, Deb P, Sarkar C, Garg A, Mehta VS, Sharma MC. Cerebral blastomycosis: A case report. Indian J Pathol Microbiol 2007;50:821-4.
[Google Scholar]
|
Fulltext Views
4,614
PDF downloads
1,631





