Translate this page into:
Disseminated cryptococcosis
Correspondence Address:
Pan-gen Cui
Jiangwangmiao Street No. 12, Nanjing, Jiangsu, 210042
China
Wen-kai Zong
Jiangwangmiao Street No. 12, Nanjing, Jiangsu, 210042
China
| How to cite this article: Yang Y, Shen Yn, Zong Wk, Cui Pg. Disseminated cryptococcosis. Indian J Dermatol Venereol Leprol 2016;82:206-208 |
Sir,
Cryptococcosis is mainly caused by two species of Cryptococcus that is, C. neoformans and C. gattii. Disseminated cryptococcosis is defined by a positive culture from at least two different sites or a positive blood culture. [1] We report a case with manifestations in lung and skin, with positive cultures from both sites identified as of the same fungus by DNA sequencing.
A 33-year-old male presented with a 3-month history of a nodule on the left upper eyelid and a 2-month history of productive cough. The nodule had enlarged gradually, after the onset of cough. There was no history suggestive of tuberculosis, acquired immunodeficiency syndrome (AIDS), idiopathic T-cell lymphopenia, diabetes mellitus, autoimmune disease, glucocorticoid use, high risk behavior or trauma. None of the family members had similar manifestations. Cutaneous examination revealed a dark red nodular plaque of size 1.5 cm × 1.0 cm with crusting, on the left upper eyelid [Figure - 1].
 |
| Figure 1: A 1.5 × 1.0 cm dark red nodular plaque with hemorrhagic crusting on the left upper eyelid |
Laboratory studies including a complete blood count, urinalysis and blood biochemistry were normal; blood and sputum cultures were negative. HIV screening was also negative. T-cell subset counts were not done. Histopathologic examination [Figure - 2]a of the cutaneous lesion revealed numerous yeast cells in the dermis which stained positive with periodic acid-Schiff (PAS) [Figure - 2]b and mucicarmine [Figure - 2]c. Fungal culture [Figure - 3] of the skin lesion yielded milky colonies in Sabouraud′s dextrose agar (SDA) medium. Mycological examination of the culture with India ink [Figure - 4] was positive. Computed tomography (CT) of the chest revealed cavitary lesions in the left lung [Figure - 5]. A fiber bronchoscopic biopsy was then done, and this revealed plenty of round organisms which stained positive with PAS and PAM (periodic acid-silver methenamine), suggestive of cryptococcus. Cryptococcus was also cultured from bronchoalveolar lavage fluid. Cerebrospinal fluid examination and a CT scan of the head were carried out, and both were normal. C. neoformans was identified in culture from both the skin and lung by multi-locus sequence typing, confirming disseminated cryptococcosis.
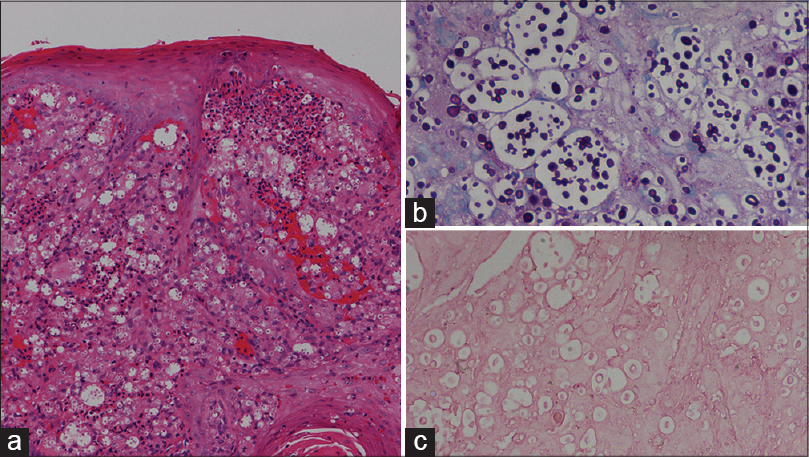 |
| Figure 2: (a) Numerous yeast cells in the dermis (H and E, ×100). (b) Yeast cells stained purple with PAS (×100) and (c) pink with mucicarmine (×100) |
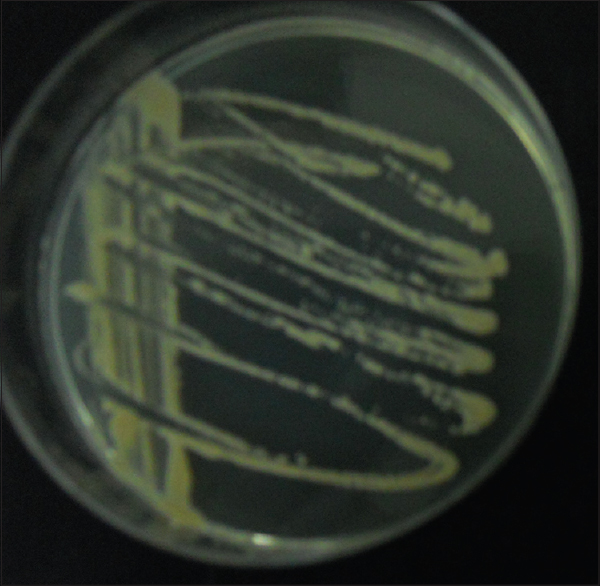 |
| Figure 3: Growth of milky colonies in SDA medium |
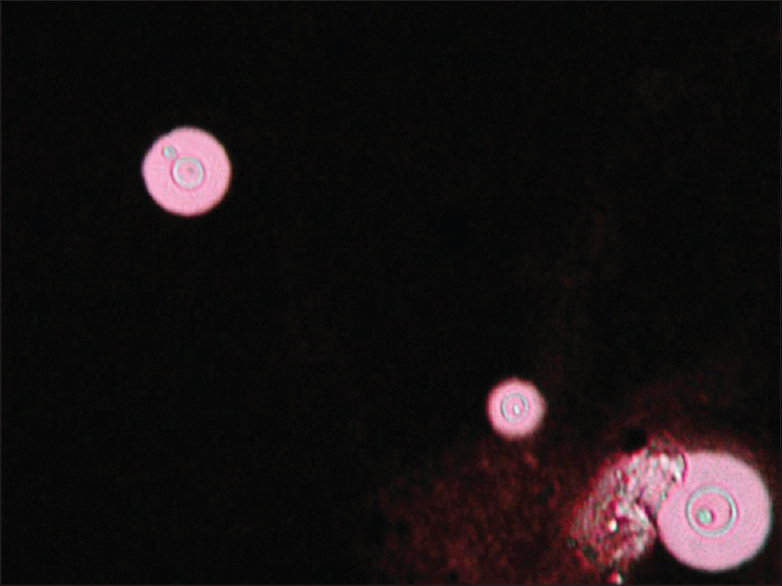 |
| Figure 4: India ink preparation showing gemmulate spores typical of Cryptococcus |
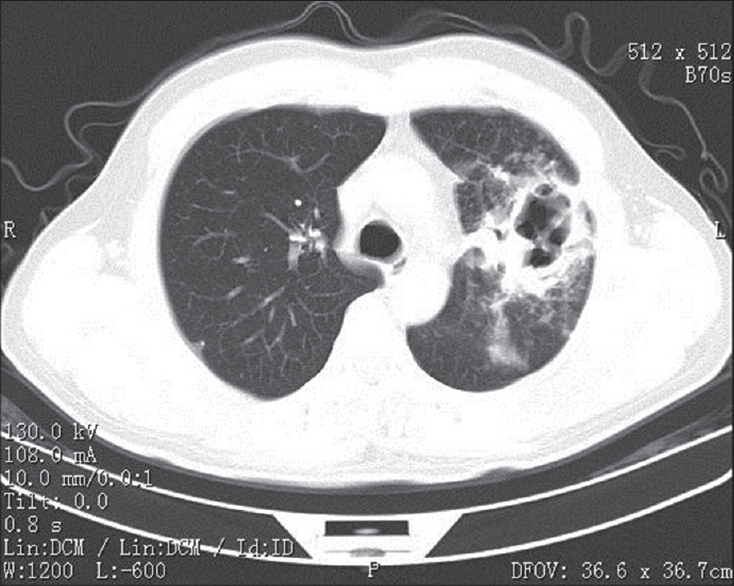 |
| Figure 5: CT scan of the chest showing multiple cavitary lesions in the left lung |
Risk factors for disseminated cryptococcosis include immunosuppression, malignancy, corticosteroid therapy, diabetes, and connective tissue disease. [2] None of these was present in our case, but he was a garbage collector and there might have been occupational exposure to Cryptococcus via soil, dust, sticks, or bird feces. Moreover, some case reports have reported disseminated cryptococcosis in immunocompetent patient. [3],[4] Manifestations of cutaneous cryptococcosis are varied. Lesions may resemble molluscum contagiosum, or appear acneiform, nodular, herpetiform, cellulitic, or keloid-like. [5]
The management of cryptococcosis is not well-defined. Amphotericin B with or without flucytosine was considered the standard treatment in patients with disseminated cryptococcosis. [6] Fluconazole has been reported to be the most utilized treatment for cutaneous cryptococcosis, with a 600 mg daily dose for 40-60 days. [5] One report describes four pulmonary cryptococcosis patients initially treated with amphotericin B developing adverse reactions to it, and oral fluconazole then being used (600 mg daily for 4-5 weeks, followed by 400 mg daily for 10-12 weeks). [7] Non-central nervous system infection in HIV patients can also be treated with oral fluconazole 200-400 mg daily. If fluconazole is not tolerated, itraconazole 200-400 mg daily for 6-12 months may be used. [8] Our patient was treated with itraconazole 200 mg daily, after he failed to respond to fluconazole, 150 mg daily for 12 days, 800 mg daily for 1 day, followed by 400 mg daily for 10 days. Response to itraconazole was evident, with the skin nodule clearing, the cough improving and the lung cavitary lesions found to have shrunk on a follow-up CT scan after 20 days of treatment. Unfortunately, he discharged himself against medical advice and was lost to follow up. This case suggests that itraconazole might be a good option for patients with lung and cutaneous involvement in C. neoformans infection.
Acknowledgment
Special thanks to MIN LI M.D. and Ph.D. (Institute of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College).
| 1. |
Chuang YM, Ho YC, Chang HT, Yu CJ, Yang PC, Hsueh PR. Disseminated cryptococcosis in HIV-uninfected patients. Eur J Clin Microbiol Infect Dis 2008;27:307-10.
[Google Scholar]
|
| 2. |
Lee JJ, Hsia RY. Cutaneous cryptococcal infection as a manifestation of disseminated disease. Cryptococcus neoformans. Ann Emerg Med 2011;57:100, 103.
[Google Scholar]
|
| 3. |
Suchitha S, Sheeladevi CS, Sunila R , Manjunath GV. Disseminated cryptococcosis in an immunocompetent patient: A case report. Case Rep Pathol. Avalilable at: http://dx.doi.org/10.1155/2012/652351. Accessed February 28, 2012.
[Google Scholar]
|
| 4. |
Godbole R, Nayar P, Pradhan A, Manchanda R. Disseminated cryptococcosis in an immunocompetent child. Indian J. Hematol. Blood Transfus 2007;23:122-24.
[Google Scholar]
|
| 5. |
Lortholary O, Nunez H, Brauner MW, Dromer F. Pulmonary cryptococcosis. Semin. Repir. Crit. Care Med. 2004;25:145-57.
[Google Scholar]
|
| 6. |
Nasser N, Nasser FN, Vieira AG. Primay cutaneous cryptococcosis in an immunocompetent patient. An Bras Dermatol 2011;86:1178-80.
[Google Scholar]
|
| 7. |
Nunez M, Peacock JE Jr, Chin R Jr. Pulmonary cryptococcosis in the immunocompetent host. Therapy with oral fluconazole: A report of four cases and a review of the literature. Chest 2000;118:527-34.
[Google Scholar]
|
| 8. |
Mehrabi M, Bagheri S, Leonard MJ, Perciaccante VJ. Mucocutaneous manifestation of cryptococcal infection: Report of a case and review of the literature. J Oral Maxillofac Surg 2005;63:1543-9.
[Google Scholar]
|
Fulltext Views
5,044
PDF downloads
2,123





