Translate this page into:
Disseminated cutaneous glomuvenous malformation
2 Department of Pathology, Indian Council of Medical Research, Safdarjung Hospital, New Delhi, India
Correspondence Address:
V Ramesh
Department of Dermatology and Sexually Transmitted Diseases, 5th Floor, OPD Block, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi - 110 029
India
| How to cite this article: Jha A, Ramesh V, Singh A. Disseminated cutaneous glomuvenous malformation . Indian J Dermatol Venereol Leprol 2014;80:556-558 |
Sir,
Glomuvenous malformations (GVMs) also known as glomangiomas are proliferations of cells of the glomus body, a specialized form of arteriovenous anastomosis involved in thermal and baroregulation. They usually present as asymptomatic pink-to-blue nodules or plaques in childhood and adolescence. [1] Multiple lesions are uncommon, representing less than 10% of all reported cases, [2] and involvement of mucous membranes is even rarer.
A 30-year-old male presented with multiple bluish to dusky red plaques and nodules since 12 years of age. The first lesion appeared over the right medial canthus and bridge of the nose as an erythematous papule. There was a gradual increase in the number of lesions thereafter, involving the nose, upper lip, arms, buttocks and trunk. Some of the lesions were painful with scant bleeding on trauma. There was no history of any systemic complaints or bleeding from visceral sites. No one else in the family was affected Cutaneous examination revealed 25-30 non-compressible to partially compressible tender plaques and nodules ranging in size from 1 cm to 5 cm over the trunk, face, arms, and buttocks. [Figure - 1] and [Figure - 2] There was no associated bruit or thrill. Over the left arm the papules were grouped to form a plaque. [Figure - 1]b Similar lesions were also present over the inner aspect of the upper lip, gingiva, and right vestibule. Keeping the provisional possibilities of glomus tumor, blue rubber bleb nevus, and venous malformation, a skin biopsy was taken from a nodule. Histological examination showed acanthosis and papillomatosis of the epidermis along with multiple ectatic dilated vascular channels in the dermis. These vascular channels were surrounded by multiple layers of cuboidal glomus cells with ovoid nuclei and eosinophilic cytoplasm. [Figure - 3] and [Figure - 4] These features were consistent with the diagnosis of glomuvenous malformation. Hemogram, liver function tests, renal function tests, urine routine microscopy, stool for occult blood, coagulation profile, and X-ray paranasal sinuses were within normal limits. At present, the patient has undergone 2 sessions of sclerotherapy with polidocainol for symptomatic lesions with minimal improvement. The patient has been counseled about the nature and usual course of the disease, and an informed decision will be made regarding planning of future sessions.
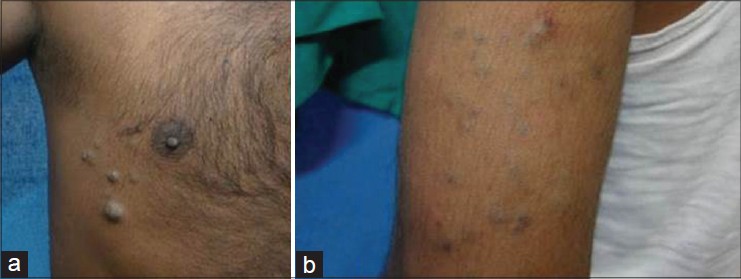 |
| Figure 1: (a) Multiple bluish nodules over the trunk (b) Bluish to erythematous papulonodules forming a plaque over the left arm |
 |
| Figure 2: Skin colored to bluish swelling on the nose |
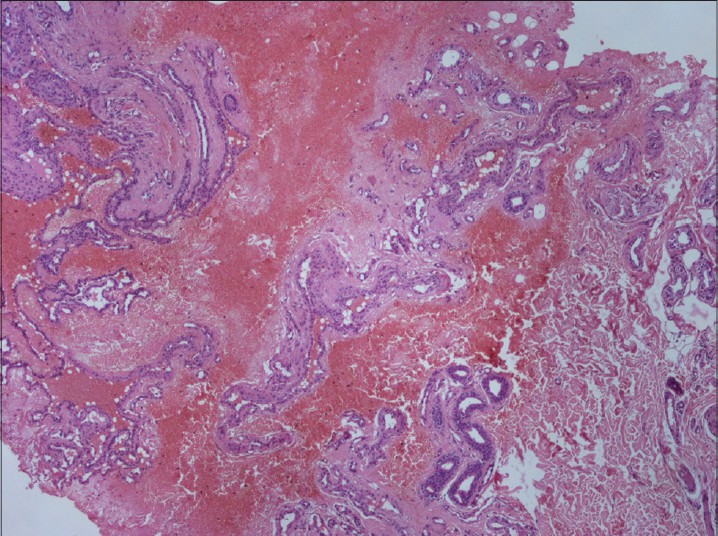 |
| Figure 3: Congested ectatic vascular channels lined by multiple layers of glomus cells |
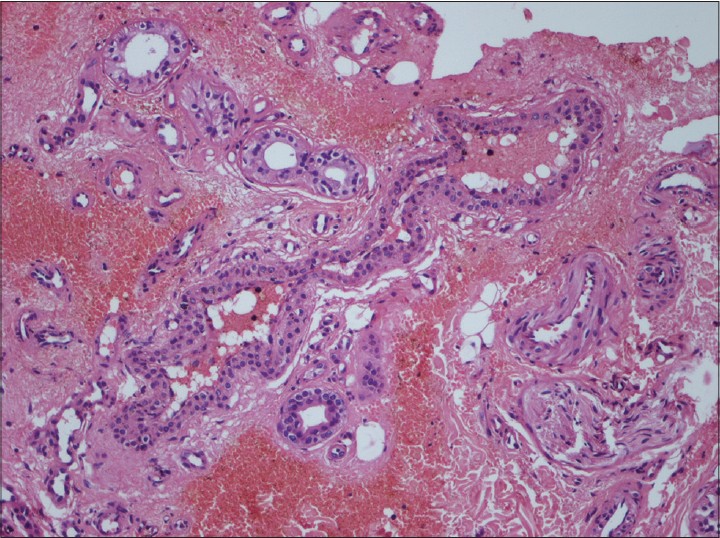 |
| Figure 4: Multiple layers of cuboidal glomus cells with ovoid nucleus and eosinophilic cytoplasm |
Glomus tumors are thought to represent neoplastic proliferations of glomus cells which are modified smooth muscle cells located in the walls of the Sucquet-Hoyer canal, a specialized arteriovenous anastomosis found most often in the fingers, and play an important role in thermoregulation. [1] Our case is unusual because the presence of bluish nodules and plaques with cobblestoning in a disseminated pattern is a rare pattern of presentation in glomangiomas. Glomus tumors can be subdivided into localized, disseminated, and congenital plaque-type forms. Localized pattern of lesions is the most common, and they present as blue-to-purple, partially compressible papules or nodules that are grouped and limited to a specific area, most commonly to an extremity. The disseminated type is less common, presenting as multiple lesions distributed over the body with no specific grouping, and the congenital plaque-like form is the rarest, consisting of either grouped papules that coalesce to form indurated plaques or clusters of discrete nodules [Table - 1].
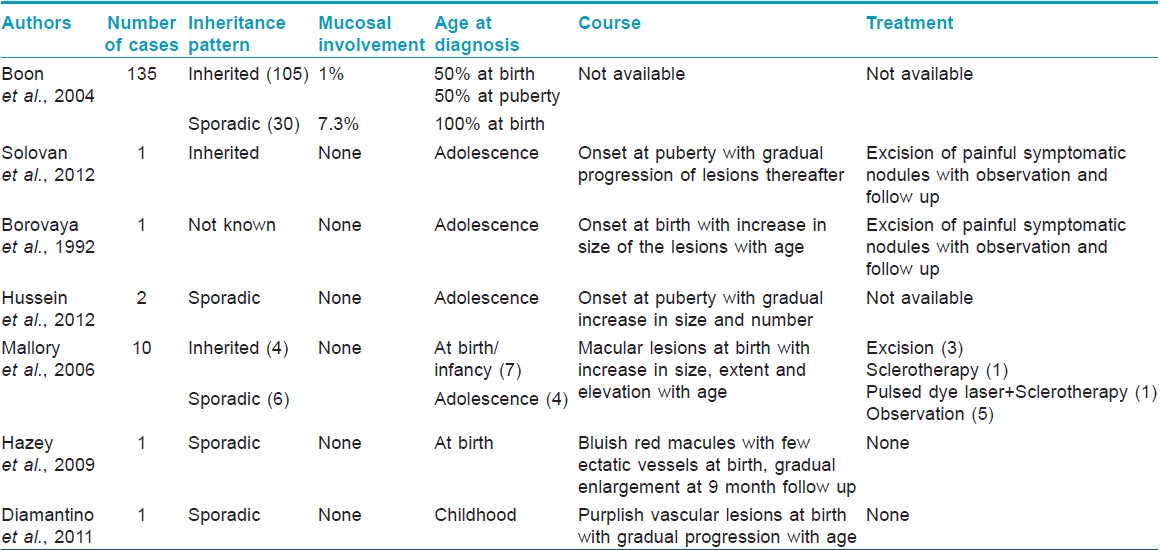
Our case had lesions involving the mucosal aspect of upper lip and right nasal vestibular area. Mucosal involvement is very rare with only occasional case reports with oral cavity, nasal cavity, and paranasal sinus involvement. [3],[4] In a large case series of 135 patients, only 1% of inherited cases had mucosal involvement whereas 7.3% of sporadic cases showed involvement of the mucosal sites. [1]
Glomuvenous malformations can be sporadic or inherited. They are thought to result from mutations in the glomulin gene. This generates a truncated glomulin protein that interferes with vascular smooth muscle differentiation and late maturation of vascular smooth muscle cells resulting in the formation of glomus cells. These cells stain positively for smooth muscle cell α actin, vimentin, and calponin but are negative for desmin, von Willebrand factor, and S-100. [5] Our patient was a sporadic case who presented with generalized lesions at puberty. Mutation analysis for glomulin gene could not be performed because the facility is not available at our centre.
Histologically, glomuvenous malformations contain multiple irregular, dilated, endothelium-lined vascular channels that are surrounded by small aggregates of cuboidal glomus cells having a round ovoid nucleus and scant eosinophilic cytoplasm. These cells are also present in the adjacent stroma. [6] In patients with multiple glomangiomas, excision should be limited to symptomatic lesions only, and asymptomatic lesions should be kept under periodic observation. [6] Other modalities that have been used are argon and carbon dioxide laser therapy, electron-beam radiation, and sclerotherapy with hypertonic saline or sodium tetradecylsulfate. However, sclerotherapy has been found to be less effective in glomuvenous malformations than in venous malformations. The prognosis for these patients is usually excellent and most patients never experience any related medical problems.
| 1. |
Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: Distinct clinicopathologic and genetic entities. Arch Dermatol 2004;140:971-6.
[Google Scholar]
|
| 2. |
Goodman TF, Abele DC. Multiple glomus tumors. A clinical and electron microscopic study. Arch Dermatol 1971;103:11-23.
[Google Scholar]
|
| 3. |
Ficarra G, Merrell PW, Johnston WH, Hansen LS. Intraoral solitary glomustumor (glomangioma): Case report and literature review. Oral Surg Oral Med Oral Pathol 1986;62:306-11.
[Google Scholar]
|
| 4. |
Constantinidis J, Kiefer A, Reitnauer K, Iro H. Glomangioma of the nasal cavity and paranasalsinuses. Rhinology 2000;38:136-9.
[Google Scholar]
|
| 5. |
Brouillard P, Boon LM, Mulliken JB, Enjolras O, Ghassibé M, Warman ML, et al. Mutations in a novel factor, glomulin, are responsible for glomuvenous malformations ("glomangiomas"). Am J Hum Genet 2002;70:866-74.
[Google Scholar]
|
| 6. |
Leger M, Patel U, Mandal R, Walters R, Cook K, Haimovic A, et al. Glomangioma. Dermatol Online J 2010;16:11.
[Google Scholar]
|
Fulltext Views
3,014
PDF downloads
2,011





