Translate this page into:
Disseminated cutaneous leiomyomatosis treated with oral amlodipine
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Dipankar De
Departments of Dermatology, Venereology, and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh
India
| How to cite this article: Aggarwal S, De D, Kanwar AJ, Saikia UN, Khullar G, Mahajan R. Disseminated cutaneous leiomyomatosis treated with oral amlodipine. Indian J Dermatol Venereol Leprol 2013;79:136 |
Sir,
The cutaneous leiomyomas most commonly manifest as piloleiomyoma, which present clinically as solitary or multiple painful tumors (leiomyomatosis). Rarely, these may present in a disseminated or zosteriform/segmental distribution. We report an unusual case of cutaneous leiomyomatosis characterized by multiple scattered papulonodular lesions present over entire body. A 32-year-old male presented with multiple painful, elevated lesions over the trunk, upper and lower limbs since 3 years. The lesions were painful on cold exposure. On examination, multiple brownish to erythematous papuloplaque and nodular lesions of 1-10 mm were scattered over whole of the trunk, upper, and lower extremities over a background of indurated skin [Figure - 1]a and b. Few were dome shaped and pedunculated. The lesions were firm in consistency and tender on palpation. The induration of the background skin was more prominent over the chest and back. General physical and systemic examinations were normal. Histopathological examination from one of the papules revealed a well-circumscribed, non-encapsulated tumor. The dermis composed of interlacing fascicles of bland spindle cells with elongated nuclei, below a clear subepidermal Grenz zone [Figure - 2]a and b. Smooth muscle actin (SMA) stain was positive [Figure - 2]c. These findings were consistent with cutaneous leiomyoma. Ultrasonography of the abdomen was normal. There was significant symptomatic relief with oral amlodipine. During the follow-up, patient developed abdominal swelling which was suspected to be of renal origin. Computerized tomography (CT) scan of abdomen and pelvis was advised but the patient was lost to follow-up. Because of the disseminated nature of the disease, we termed it as disseminated cutaneous leiomyomatosis. The patient was treated with amlodipine, 10 mg daily for 2 months with which he had a significant relief from pain although there was only marginal regression of the lesion [Figure - 3]a and b.
 |
| Figure 1: (a) Multiple scattered cutaneous leiomyomas present over the whole of the chest (b) Multiple scattered cutaneous leiomyomas present over back |
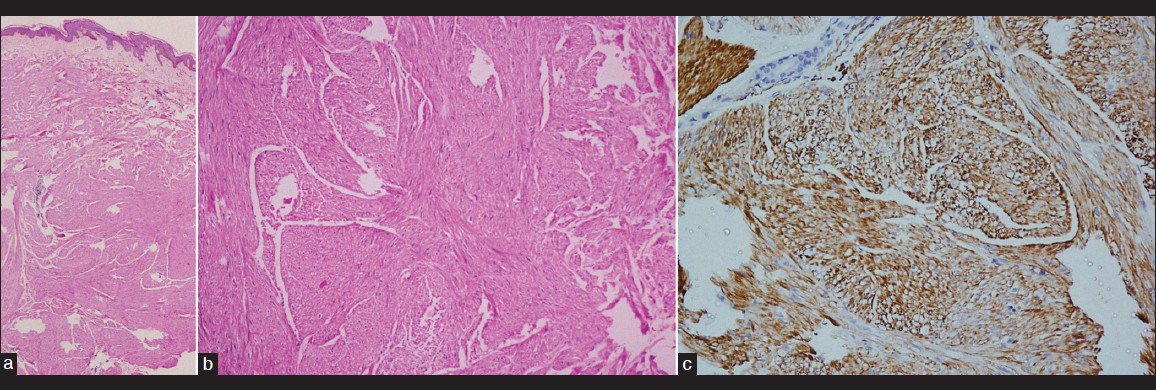 |
| Figure 2: (a) Interlacing fascicles of bland spindle cells with elongated nuclei (H and E, ×280), (b) Smooth muscle cells with blunt-shaped nuclei and eosinophilic cytoplasm (H and E, ×540), (c) Smooth muscle actin stain (H and E, ×280) showing positive staining for smooth muscle fiber |
 |
| Figure 3: (a) Marginal decrease in size of the lesions over chest, (b) Minimal decrease in size of leiomyomas over back |
Cutaneous leiomyoma is a benign smooth muscle tumor. It can occur either at arrector pilorum muscles of hair follicle, the tunica dartos of the scrotum, muscle of the areola, muscles of vulva, or vascular smooth muscles. The most common cutaneous leiomyoma is piloleiomyoma, [1] and the most common presentation is multiple lesions on the body, but the generalized presentation is rare.
A 32-year-old male presented with multiple painful, elevated lesions over the trunk, upper and lower limbs since 3 years. The lesions first appeared on the chest and over a period of 6 months, he developed similar lesions over the rest of the trunk and extremities. The lesions were painful on cold exposure. His family history was non-contributory. On examination, multiple brownish to erythematous papuloplaque and nodular lesions of 1-10 mm were scattered over whole of the trunk, upper, and lower extremities over an indurated skin [Figure - 1]a and b. Few were dome shaped and pedunculated. The lesions were firm in consistency and tender on palpation. The induration of the background skin was more prominent over the chest and back. General physical and systemic examinations were normal. Histopathological examination from one of the papules revealed a well-circumscribed, non-encapsulated tumor. The dermis composed of interlacing fascicles of bland spindle cells with elongated nuclei, below a clear subepidermal Grenz zone [Figure - 2]a and b. SMA stain was positive [Figure - 2]c. These findings were consistent with cutaneous leiomyoma. Ultrasonography of the abdomen was normal. Because of the extensive nature of the disease, surgery or any destructive therapy was avoided and to provide symptomatic relief, the patient was initially treated with 10 mg nifedipine twice daily for 1 week. Due to headache caused by nifedipine, it was replaced with amlodipine, 5 mg twice daily for 2 months. There was significant relief from pain although there was marginal regression of the lesion [Figure - 3]a and b. Two months later, the patient presented with insidious onset of pain in the abdomen along with loss of weight. On abdominal palpation, a firm to hard mass was palpable in the left hypochondrium and lumbar region extending to the umbilicus. Consultation from general surgeon was sought, and it was suspected to be a tumor of abdominal origin, possibly originating from the left kidney. A CT of the whole abdomen and pelvis was advised to the patient. But patient did not return for follow-up.
Piloleiomyomas usually present as multiple tumors (leiomyomatosis), but it can be solitary, disseminated, or zosteriform/segmental. Zosteriform and disseminated cutaneous leiomyomas have been reported simultaneously in the same patient. [2] They typically appear during second to fourth decades of life as grouped papules or nodules on the trunk and limbs and are characteristically painful on exposure to pressure or low temperature. Multiple leiomyomas usually have a progressive course with gradual increase in size. [1] Our case is atypical as the lesions were present almost all over the whole body. Mitra et al[3] proposed the term diffuse pilar leiomyoma for a new clinical variant that was exceptionally large (15 cm in diameter) and was diffuse. Multiple cutaneous leiomyomata are found to be associated with uterine leiomyomata referred as multiple cutaneous and uterine leiomyomatosis (MCUL), inherited as an autosomal-dominant trait. A small proportion of families with MCUL also show aggressive renal cancer; MCUL is then known as hereditary leiomyomatosis and renal cell carcinoma (HLRCC). [4] Both MCUL and HLRCC have been found to be associated with heterozygous germline mutation in fumarate hydratase gene (FH), a tumor suppressor gene. [4] A number of reports have been published with multiple leiomyomas without uterine leiomyoma/renal tumor, but none of these cases had such striking diffuse involvement of the body. Our patient did not have any evidence of renal tumor or any family history of similar skin lesions/renal tumors at initial presentation. Subsequently, he developed signs and symptoms of abdominal malignancy which could not be confirmed. Due to unavailability of FH mutation studies, it could not be done in our patient.
Treatment of choice for solitary cutaneous leiomyoma is excision but for extensive lesions, medical treatment has been used with variable results. Various drugs, include calcium channel blockers (nifedipine), α-adrenoceptors blockers (phenoxybenzamine), nitrates, analgesics, antidepressants, and gabapentin. A new therapeutic approach for leiomyoma has been the use of botulinum toxin. [5] Calcium channel blockers (nifedipine) have been used previously with good results in painful cutaneous leiomyomas. Long-term therapy with nifedipine (up to 3 years) leads to almost total suppression of pain. [6] Amlodipine may act through similar mechanism of action, but it has lesser incidence of side effects like headache, and flushing than nifedipine. Thus, amlodipine can be used as first-line treatment to reduce the morbidity associated with this relatively benign condition. A regular follow-up along with appropriate imaging is necessary at initial stage for early detection of any internal malignancy associated with these lesions.
| 1. |
Fisher WC, Helwig EB. Leiomyomas of the skin. Arch Dermatol 1963;88:510-20.
[Google Scholar]
|
| 2. |
Agarwalla A, Thakur A, Jacob M, Joshi A, Garg VK, Agrawal S. Zosteriform and disseminated lesions in cutaneous leiomyoma. Acta Derm Venereol 2000;80:446.
[Google Scholar]
|
| 3. |
Mitra A, Gudgeon PW, Merchant W, Shah M. A case of diffuse pilar leiomyoma or acquired smooth muscle hamartoma? Clin Exp Dermatol 2009;34:e145-7.
[Google Scholar]
|
| 4. |
Launonen V, Vierimaa O, Kiuru M, Isola J, Roth S, Pukkala E, et al. Inherited susceptibility to uterine leiomyomas and renal cell cancer. Proc Natl Acad Sci U S A 2001;98:3387-92.
[Google Scholar]
|
| 5. |
Onder M, Adiºen E. A new indication of botulinum toxin: Leiomyoma-related pain. J Am Acad Dermatol 2009;60:325-8.
[Google Scholar]
|
| 6. |
Biltz H, Uerlich M, Kreysel HW. Long-term therapy of multiple piloleiomyomas with nifedipine. Z Hautkr 1987;62:1596, 1599-600.
[Google Scholar]
|
Fulltext Views
3,093
PDF downloads
2,060





