Translate this page into:
Disseminated cutaneous phaeohyphomycosis due to Cladophialophora bantiana
2 Department of Dermatology and Venereology, Govt Medical College, Thrissur, Kerala, India
3 Department of Pathology, Govt Medical College, Kozhikode, Kerala, India
4 Department of Microbiology, Govt Medical College, Kozhikode, Kerala, India
Correspondence Address:
Anza Khader
5/1986 B,"Maskan" Rajiv Nagar Colony, PO Puthiyara - 673 004, Kozhikode, Kerala
India
| How to cite this article: Khader A, Ambooken B, Binitha MP, Francis S, Kuttiyil AK, Sureshan DN. Disseminated cutaneous phaeohyphomycosis due to Cladophialophora bantiana. Indian J Dermatol Venereol Leprol 2015;81:491-494 |
Abstract
Cladophialophora bantiana is a neurotropic dematiaceous fungus which only rarely affects the skin. We report a case of disseminated cutaneous phaeohyphomycosis caused by Cladophialophora bantiana in an immunocompromised female who presented with multiple pyogenic granuloma-like nodules, dermatophytosis-like plaque, and subcutaneous cysts on the upper and lower extremities without systemic involvement. Biopsy revealed black yeasts resembling sclerotic bodies and culture yielded irregular, velvety, grey colonies with black reverse. Excisionof the nodules and treatment with oral itraconazole 100 mg twice daily resulted in complete clinical resolution within two months, following which itraconazole was administered for another 4 months.INTRODUCTION
Phaeohyphomycosis was a term introduced by Ajello et al. in 1974 to denote infections caused by a variety of dematiaceous fungi characterized by pigmented hyphae in the tissue. Many cases were previously misdiagnosed as chromoblastomycosis especially in the absence of tissue cultures. There are very few reports of localized cutaneous phaeohyphomycosis due to Cladophialophora bantiana, a neurotropic fungus. [1]
Case Report
A 38-year-old female presented with multiple skin tumors of 2 months duration, with recurrent episodes of bleeding from the lesions. There was no previous history of trauma. Her medical history included membranous glomerulonephritis and nephrotic syndrome for which she had been on oral corticosteroids and cyclosporine for the past 8 months.
General examination showed features of Cushing′s syndrome with truncal obesity and facial hypertrichosis. Dermatological examination revealed multiple reddish dome shaped and flat surfaced nodules of size ranging from 2 × 2 cm to 7 × 8 cm over both lower limbs resembling pyogenic granulomas [Figure - 1]. There was an erythematous plaque with scaling along the borders and a clear centre over the lateral border of the left foot mimicking dermatophytosis [Figure - 2]. In addition, there were two cystic swellings on the base of the left middle finger and the dorsum of the left hand [Figure - 3].
 |
| Figure 1: Reddish dome shaped nodule resembling pyogenic granuloma |
 |
| Figure 2: Erythematous plaque mimicking dermatophytosis |
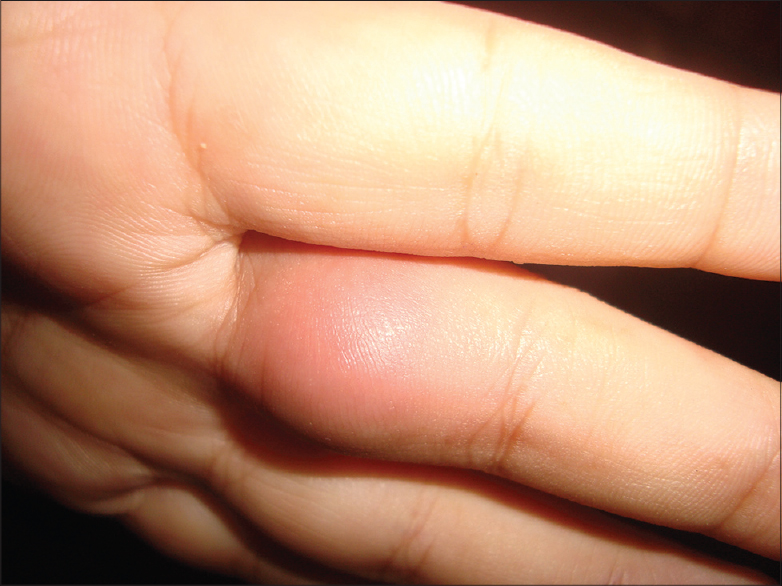 |
| Figure 3: Subcutaneous cyst of the finger |
Laboratory investigations including complete blood cell count, liver and renal function tests were within normal limits except for a raised erythrocyte sedimentation rate (ESR) of 80mm/h. Screening for hepatitis B, hepatitis C and human immunodeficiency virus, as well as serology for antinuclear and anti double-stranded DNA antibodies were negative. Chest X-ray and electrocardiogram were normal. An ultrasonogram of the abdomen and computed tomography scan of the brain and chest were normal indicating that there was no systemic dissemination.
Scrapings from the plaque and wet mount examination revealed septate hyphae. Biopsy from a nodule revealed hyperkeratosis, acanthosis, hemorrhage, and ulceration with a dense inflammatory infiltrate in the dermis. There were large black spores within and outside giant cells suggestive of chromoblastomycosis [Figure - 4]a and b. Pigmented fungal elements in the form of pseudohyphae were detected with Periodic acid Schiff and Masson-Fontana stains [Figure - 4]c. Fungal culture of aspirate and tissue samples from the cysts, nodules, and plaque yielded irregular, velvety, gray colonies with black reverse within 7 days of incubation [Figure - 5]a. Microscopy showed plenty of septate hyphae with unicellular microconidia branching at acute angles surviving incubation upto 40°C [Figure - 5]b. All these features were characteristic of Cladophialophora bantiana.
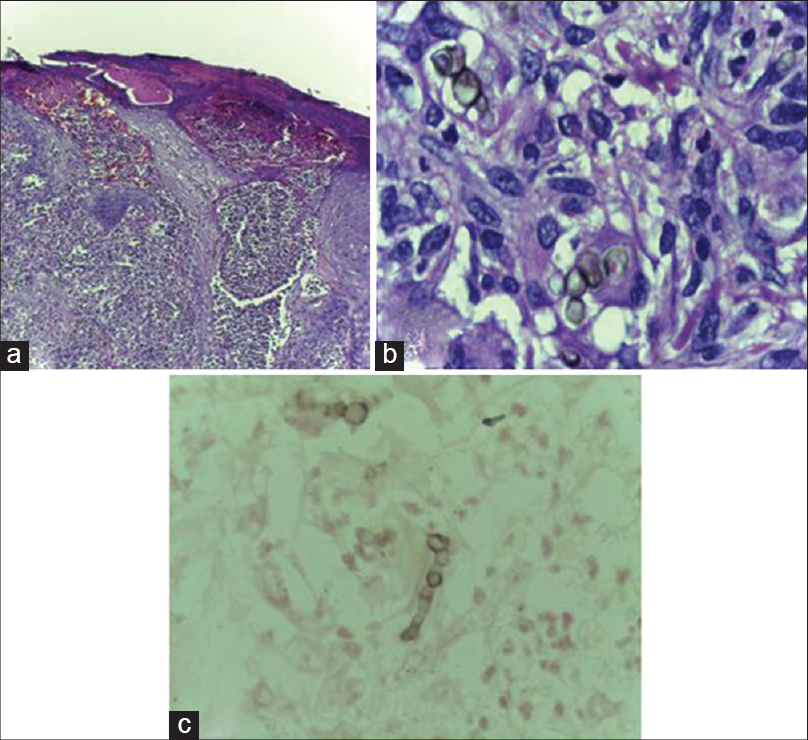 |
| Figure 4: (a)Hyperkeratosis, acanthosis, hemorrhage in the epidermis, and dense inflammatory infiltrate in the dermis, H and E, ×100 (b) Large black spores within and outside giant cells, H and E, ×400 (c) Pseudohyphae, Masson– Fontana stain ×400 |
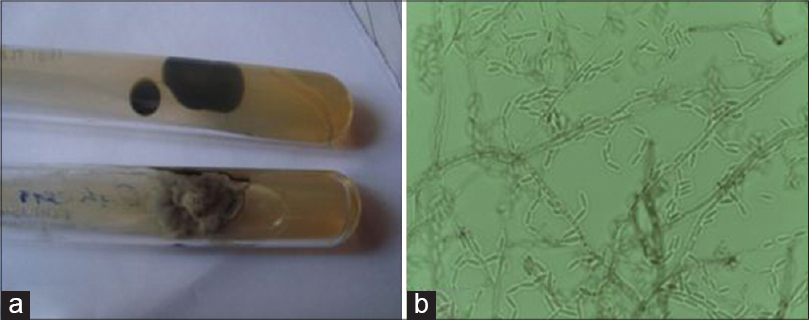 |
| Figure 5: (a) Irregular, velvety, gray colored colonies with black reverse, (b) septate hyphae with unicellular microconidia branching at acute angles, ×400 |
The two larger nodules were surgically excised and the patient was treated with oral itraconazole, 100mg twice daily. Two months after initiating treatment, there was complete resolution of all the lesions. However, itraconazole was continued for a total of 6 months in order to ensure eradication of the infection. There has been no sign of recurrence during 1 year of follow-up.
DISCUSSION
Fungal infections produce diverse clinical features that pose difficulty in diagnosis and management. Phaeoid or pigmented fungi cause a diverse group of infections which includes chromoblastomycosis producing sclerotic bodies, eumycetomas producing grains and phaeohyphomycosis which forms yeast-like cells, pseudohyphae, hyphae or a combination of these in the infected tissues. Most infections follow inoculation of the fungus from soil or wood into abraded skin. [2]
Phaeohyphomycosis is known to occur in four clinical categories: superficial, cutaneous or corneal, subcutaneous, and visceral forms. Superficial infections include black piedra and tinea nigra. Cutaneous diseases are similar to dermatophytosis. Subcutaneous infection causes a solitary abscess, "phaeohyphomycotic cyst" usually over the extremities. More than 100 species have been implicated as causative agents of which the most common are Exophiala, Alternaria, Bipolaris, Curvularia, and Wangiella. [3]
Disseminated phaeohyphomycosis with multiple cystic lesions and systemic involvement is rare and is usually seen in immunocompromised patients. [3] A report from India describes disseminated lesions in four patients, of whom two patients had both cysts and warty plaques. The causative agents included Phialophora dermatidis, Exophiala jeanselmi, and Alternaria alternata. [1] Dissemination occurs as a result of hematogenous spread from a primary focal infection. Melanin is a virulence factor that acts as an antioxidant against oxidative bursts produced by phagocytes. It also binds to the host hydrolytic enzymes that target fungal plasma membrane. [4]
Phaeohyphomycosis differs from chromoblastomycosis in the appearance of the etiological agent as brown-black hyphae in the tissues of the former and sclerotic bodies in those of the latter. Among the etiological agents of phaeohyphomycosis, Exophiala dermatidis is known to produce sclerotic bodies - like rounded structures in the tissue. [1]
Cladophialophora bantiana is predominantly a neurotropic fungus causing phaeohyphomycosis in the central nervous system of both humans and animals. [4] There are very few reports of cutaneous infection due to Cladophialophora bantiana. [1] The skin lesions known to be caused by Cladophialophora bantiana include papulo-nodules, plaques, nodules with pustules, nodules with sinuses, and ulcerative lesions. [5],[6],[7],[8],[9]
Cladophialophora bantiana elicits a blastomycosis-like tissue reaction or forms a phaeomycotic cyst. The pigmented fungal elements seen with hematoxylin-eosin stain include septate hyphae, pseudohyphae, globose to oval yeast like cells, budding cells and spherical cells with prominent septations. The latter resemble sclerotic bodies but differ in having thinner cell walls, a single planate septum, and stain black with Masson-Fontana stain. [9] The fungus grows within 7-8 days on routine fungal culture media at room temperature, at 37°C and at temperatures higher than 40°C. The colonies mature within 15 days of incubation and show a velvety texture and olivaceous gray to brown colour with a black reverse. The fungus shows hyaline-to-brown, septate hyphae and have smooth walled, single-celled, pale olivaceous, ellipsoidal to spindle-shaped conidia arranged in long, strongly coherent chains. [10]
Our patient did not have a history of antecedent trauma but was immunocompromised due to long-term steroids and cyclosporine. Three types of morphological patterns, pyogenic granuloma-like nodules, dermatophytosis-like plaques, and subcutaneous cysts, coexisted in our patient. We were unable to find any previous reports of pyogenic granuloma - like lesions caused by Cladophialophora bantiana.
Physicians should consider cutaneous phaeohyphomycosis in the differential diagnosis of plaques, nodules, and cysts in the skin, especially in the setting of immunosuppression. The characteristic colonies and morphology of the fungus help to identify the species facilitating early diagnosis and management, which may prevent systemic dissemination and lead to a favorable outcome.
| 1. |
Sharma NL, Mahajan V, Sharma RC, Sharma A. Subcutaneous pheohyphomycosis in India-a case report and review.Int J Dermatol 2002;41:16-20.
[Google Scholar]
|
| 2. |
Pereira RR, Nayak CS, Deshpande SD, Bhatt KD, Khatu SS, Dhurat RS. Subcutaneous phaeohyphomycosis caused by cladophialophora boppii. Indian J Dermatol Venereol Leprol 2010;76:695-8.
[Google Scholar]
|
| 3. |
Shivaswamy KN, Pradhan P, Laxmisha C, Thappa DM, Jayanthi S. Disseminated pheohyphomycosis.Int J Dermatol 2007;46:278-81.
[Google Scholar]
|
| 4. |
Chester R, Cooper JR. Deep pheohyphomycosis. In: Merz GW and Hay RJ, editors. Topley and Wilsons microbiology and microbial infections, 10 th ed. Hoboken, New Jersey: John Wiley and Sons Publishers; 2005. p. 740-4.
[Google Scholar]
|
| 5. |
Jacyk WK, Bruyn JH, Holm N, Gryffenberg H, Karusseit VO. Cutaneous infection due to Cladophialophora bantianain a patient receiving immunosuppressive therapy. Br J Dermatol 1997;136:428-30.
[Google Scholar]
|
| 6. |
Neoh CY, Tan SH, Perera P. Cutaneous pheohyphomycosis due to Cladophialophora bantiana in an immunocompetent patient.Clin Exp Dermatol 2007;32:539-40.
[Google Scholar]
|
| 7. |
Patterson JW, Warren NG, Kelly LW. Cutaneous pheohyphomycosis due to cladophialophora bantiana. J Am Acad Dermatol 1999;40:364-6.
[Google Scholar]
|
| 8. |
Amma SM, Panicker CKJ, Iype PT, Rangaswamy S. Pheohyphomycosis caused by cladosporiumbantianum in Kerala (India). Sabouraudia 1979;17:419-23.
[Google Scholar]
|
| 9. |
Gugnani HC, Suseelan AV, Nwokolo C, Njoku-Obi AN.Cutaneous cladosporiosis due to cladosporium due to cladosporium trichoides. J Trop Med Hyg 1977;80:177-8.
[Google Scholar]
|
| 10. |
Ajantha GS, Kulkarni RD. Cladophialophora bantiana, the Neurotropic Fungus - A Mini Review. J Clin Diagn Res 2011;5:1301-6.
[Google Scholar]
|
Fulltext Views
4,086
PDF downloads
2,763





