Translate this page into:
Dyschromatosis symmetrica hereditaria with neurological abnormalities
2 Department of Dermatology, Venereology, and Leprosy, RG Kar Medical College, Kolkata, West Bengal, India
3 Department of Dermatology, Venereology, and Leprosy, North Bengal Medical College, Darjeeling, India
Correspondence Address:
Sudip Kumar Ghosh
Department of Dermatology, Venereology, and Leprosy, RG Kar Medical College, 1, Khudiram Bose Sarani, Kolkata - 700 004, West Bengal
India
| How to cite this article: Dutta A, Ghosh SK, Mandal RK. Dyschromatosis symmetrica hereditaria with neurological abnormalities . Indian J Dermatol Venereol Leprol 2014;80:549-551 |
Sir,
Dyschromatosis symmetrica hereditaria (DSH) is a pigmentary genodermatosis of autosomal dominant inheritance which is characterized by a combination of hyperpigmented and hypopigmented macules on the face, back of the hands, and feet. [1] The condition primarily affects the skin and has rarely been associated with neurologic manifestations.
A 2-year old boy, born to non-consanguineous parents presented with hyperpigmented and hypopigmented spots on his hands and feet that began at 3 months of age. Till 18 months of age, he achieved normal developmental milestones but 6 months prior to presenting to us, the parents noted regression in language development and behavioral problems like unaccustomed laughing and crying. There was no history of associated seizures or jaundice and his perinatal history was uneventful. No one else in the family had similar skin lesions or any neurological abnormality. Examination revealed freckle-like pigmented macules on his face. In addition, hyperpigmented and hypopigmented macules arranged in a reticulate pattern were present over the dorsa of hands and feet [Figure - 1]. The surface of skin lesions did not show telangiectasia, atrophy, or scaling. Palms, soles, and mucosa were spared. There were no similar lesions elsewhere on his body. He was able to stand without support and walked with an abnormal gait with inverted feet. A dystonic (hypertonic) posture was observed in both upper and lower limbs (right more than left) along with brisk deep tendon reflexes. Rest of the systemic examination including ophthalmological examination was normal. Laboratory investigations, including routine blood and metabolic screening, calcium, phosphorus, magnesium, serum lactate, thyroid and parathyroid function, hepatic function, and serum ceruloplasmin level, TORCH screening [Toxoplasmosis, Other (syphilis, varicella-zoster, parvovirus B19), Rubella, Cytomegalovirus (CMV), and Herpes infections], and urine examination was normal. Histopathological examination of a 4 mm punch biopsy specimen of a hyperpigmented area showed increased pigmentation of the basal layer. Based on the clinical features and the histopathological findings, a diagnosis of dyschromatosis symmetrica hereditaria was made. Computed tomographic (CT) scan of the brain showed bilaterally symmetrical calcifications in the region of basal ganglia [Figure - 2]. No other structural change of brain was identified. Electroencephalography (EEG) was normal. Clinical and radiological (CT scan of brain) evaluation of his parents showed no abnormality. We could not perform any genetic analysis to confirm the mutation in the involved gene in the present case due to non-availability of required facilities and financial constraints.
 |
| Figure 1: Pigmentary changes on dorsum of feet |
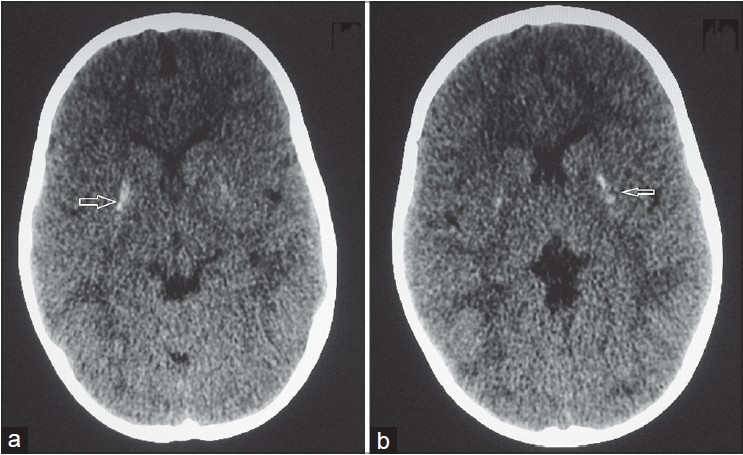 |
| Figure 2: (a and b) Computed tomographic scan of brain showing bilateral basal ganglia calcification (marked by arrows) |
Dyschromatosis symmetrica hereditaria, synonymously known as reticulate acropigmentation of Dohi, has been reported mainly in the Japanese and Chinese population. It occurs due to a mutation in the adenosine deaminase, RNA specific gene ADAR1 which catalyzes the hydrolytic deamination of adenosine to inosine in double-stranded RNA. [2] To date, more than 100 mutations of ADAR1 have been reported in patients with this condition, and the catalytic domain deaminase is believed to be crucial to the activities of this gene. [3],[4],[5] The disease is usually restricted to the skin and only a limited number of cases have been reported in association with extra-cutaneous abnormality. [3],[6] An extensive search of the English language literature in PubMed, Medline, and Google Scholar database revealed only a few cases showing an association with neurological abnormalities. Pigmentation begins in infancy or childhood and gradually increases in depth and extent. Once these hypopigmented and hyperpigmented lesions are fully established, they persist life long without any change in color or distribution. Biopsy of hyperpigmented and hypopigmented macules shows basal layer melanosis and hypomelanosis, respectively. [11] Family history is present in 56-77.6% of patients with DSH. [3],[7] There is no definitive treatment for this condition. The disease needs to be differentiated from dyschromatosis universalis hereditaria (DUH), which is characterized by more extensive lesions including the non-acral and covered areas of the skin. Some other differential diagnoses include reticulate acropigmentation of Kitamura, mild variants of xeroderma pigmentosum, dyschromic amyloidosis, dyskeratosis congenita, and disorders due to exposure to chemicals or radiation, amongst others. [11] Neurological abnormalities in the form of seizure, dystonia and developmental regression, autistic disorder, and depression have been reported to be associated with dyschromatosis symmetrica hereditaria. [3],[4] In 1994, Patrizi et al., reported a 9-year-old Caucasian girl who developed cutaneous changes at the age of 2 years and torsion dystonia at the age of 7 years. [12] Kondo et al., reported a case which had similar neurologic and imaging findings as in our patient. [2] Tojo et al., described a familial case of this disease with dystonia, metal deterioration, brain calcification along with aortic root sclerosis. [13] Kaliyadan et al., described a case of dyschromatosis symmetrica hereditaria in a 9-year-old Indian girl who had progressive regression of developmental milestones, feeble vocalization, difficulty in walking, and dystonic posturing. [10] In 2013, Peng et al. reported a retrospective series of dyschromatosis symmetrica hereditaria, three of whom had neuro-psychiatric manifestations. [3]
Although a few cases of this condition have been reported from India, [7],[8],[9] we found only one previous report with associated neurological anomalies. [10] The exact etiology of the association with neurological manifestations in general and bilateral basal ganglia calcification and dystonia in particular is not known.
| 1. |
Oyama M, Shimizu H, Ohata Y, Tajima S, Nishikawa T. Dyschromatosis symmetrica hereditaria (reticulate acropigmentation of Dohi): Report of a Japanese family with the condition and a literature review of 185 cases. Br J Dermatol 1999;140:491-6.
[Google Scholar]
|
| 2. |
Kondo T, Suzuki T, Ito S, Kono M, Negoro T, Tomita Y. Dyschromatosis symmetrica hereditaria associated with neurological disorders. J Dermatol 2008;35:662-6.
[Google Scholar]
|
| 3. |
Peng AC, Chen AY, Chao SC. Dyschromatosis symmetrica hereditaria: A retrospective case series and literature review. Dermatol Sin 2013;31:19-24.
[Google Scholar]
|
| 4. |
Hayashi M, Suzuki T. Dyschromatosis symmetrica hereditaria. J Dermatol 2013;40:336-43.
[Google Scholar]
|
| 5. |
Chen YA, Chao SC, Lee JY. A novel deletion mutation in the adenosine deaminase RNA-specific gene in a Taiwanese patient with dyschromatosis symmetrica hereditary. Dermatol Sin 2011;29:109-10.
[Google Scholar]
|
| 6. |
Miyamura Y, Suzuki T, Kono M, Inagaki K, Ito S, Suzuki N, et al. Mutations of the RNA-specific adenosine deaminase gene (DSRAD) are involved in dyschromatosis symmetrica hereditaria. Am J Hum Genet 2003;73:693-9.
[Google Scholar]
|
| 7. |
Sharma R, Chandra M. Reticulate acropigmentation of dohi-a report of two unrelated families. Indian J Dermatol Venereol Leprol 2000;66:139-40.
[Google Scholar]
|
| 8. |
Mohana D, Verma U, Amar AJ, Choudhary RK. Reticulate acropigmentation of dohi: A case report with insight into genodermatoses with mottled pigmentation. Indian J Dermatol 2012;57:42-4.
[Google Scholar]
|
| 9. |
Rao KS, Shetty JN. Acropigmentation of dohi. Indian J Dermatol Venereol Leprol 1998;64:128-9.
[Google Scholar]
|
| 10. |
Kaliyadan F, Vinayan KP, Fernandes B, Jayasree MG. Acral dyschromatosis with developmental regression and dystonia in a seven-year-old child: Dyschromatosis symmetrica hereditaria variant or a new syndrome?. Indian J Dermatol Venereol Leprol 2009;75:412-4.
[Google Scholar]
|
| 11. |
James WD, Berger TG, Elston DM. Andrew's Diseases of the Skin. 10 th ed. Philadelphia: Saunders Elsevier; 2011.
th ed. Philadelphia: Saunders Elsevier; 2011.'>[Google Scholar]
|
| 12. |
Patrizi A, Manneschi V, Pini A, Baioni E, Ghetti P. Dyschromatosis symmetrica hereditaria associated with idiopathic torsion dystonia. A case report. Acta Derm Venereol 1994;74:135-7.
[Google Scholar]
|
| 13. |
Tojo K, Sekijima Y, Suzuki T, Suzuki N, Tomita Y, Yoshida K, et al. Dystonia, mental deterioration, and dyschromatosis symmetrica hereditaria in a family with ADAR1 mutation. Mov Disord 2006;21:1510-3.
[Google Scholar]
|
Fulltext Views
5,513
PDF downloads
1,844





