Translate this page into:
Early clinical and histological changes induced by microneedling in facial melasma: A pilot study
2 Department of Dermatology and Radiotherapy, FMB-UNESP, Botucatu, SP, Brazil
3 Santa Casa de Misericórdia, Recife, PE, Brazil
Correspondence Address:
Daniel Pinho Cassiano
Rua Borges Lagoa, 508, São Paulo, SP, CEP: 04038-000
Brazil
| How to cite this article: Cassiano DP, Esp�sito AC, Hassun KM, Lima EV, Bagatin E, Miot HA. Early clinical and histological changes induced by microneedling in facial melasma: A pilot study. Indian J Dermatol Venereol Leprol 2019;85:638-641 |
Sir,
Melasma is a common, relapsing pigmentary disorder that has a major impact on the quality of life of the affected patients. Its pathology is heterogeneous, involving not only the epidermal layers but also upper dermal changes such as solar elastosis, collagen disruption, and basement membrane damage.[1] Gentle skin microneedling has been reported as a successful adjuvant approach for treating melasma. It decreases epidermal melanin density, produces epidermal thickening and restores the basement membrane and the upper dermal collagen.[2] However, the key role of microneedling in the improvement of melasma has not been thoroughly investigated, especially with respect to the associated histological changes.
The objective of this study was to evaluate the early histological changes caused by micro needling, as well as the clinical improvement: 7 days after a single session treatment for facial melasma.
We performed a quasi-experimental trial that enrolled 20 women with facial melasma who were evaluated at baseline (T0) and after 7 days of the treatment session (T7) through standardized photography (VISIA ™; Canfield; Parsippany, NJ, USA), melasma quality of life questionnaire for brazilian portuguese language (MELASQoL-BP), and colorimetry. Quasi experimental trial = non random allocation. Ten first participants were allocated to the microneedling group and submitted to a biopsy (punch 3 mm) of the facial melasma lesions, followed by one session of 1.5mm micro needling (Dr. Roller ™; Derma Rolling System; Gyeonggi Province, Korea) according to Lima protocol.[3] After 1 week, the microneedling group was subjected to a new biopsy. All participants used broad-spectrum sunscreen (Color SPF 50 Ideal Soleil ™; Vichy). Skin samples were stained with periodic acid–Schiff, Fontana-Masson, and Herovici and marked with Ki67 immunohistochemistry. A blinded examiner analyzed the photographs and the histologic slides.
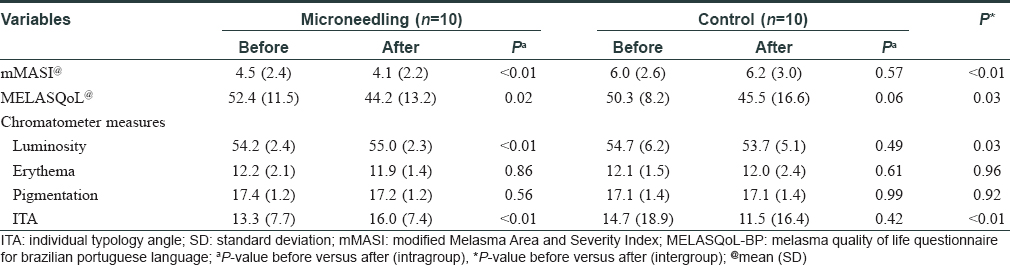
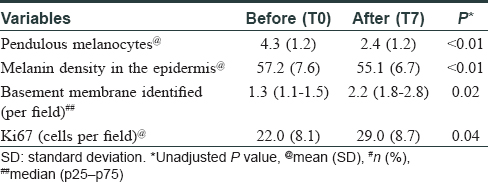
The two groups were comparable (P > 0.1) regarding age, skin phototype, pregnancies, sun exposure, and severity of melasma [Table - 1]. Clinical severity assessed by modified Melasma Area and Severity Index (mMASI), colorimetry, and quality of life parameters improved only in the microneedling group [Table - 2]. There was a significant reduction in melanin density, pendulous melanocytes and basement membrane damage per histological field. In addition, microneedling induced slight epidermal hyperplasia, subepidermal deposition of extracellular substances (glycosaminoglicans and fibrin), fibroblast proliferation, and increase in Ki67 marked keratinocytes after 7 days [Table - 3] and [Figure - 1].

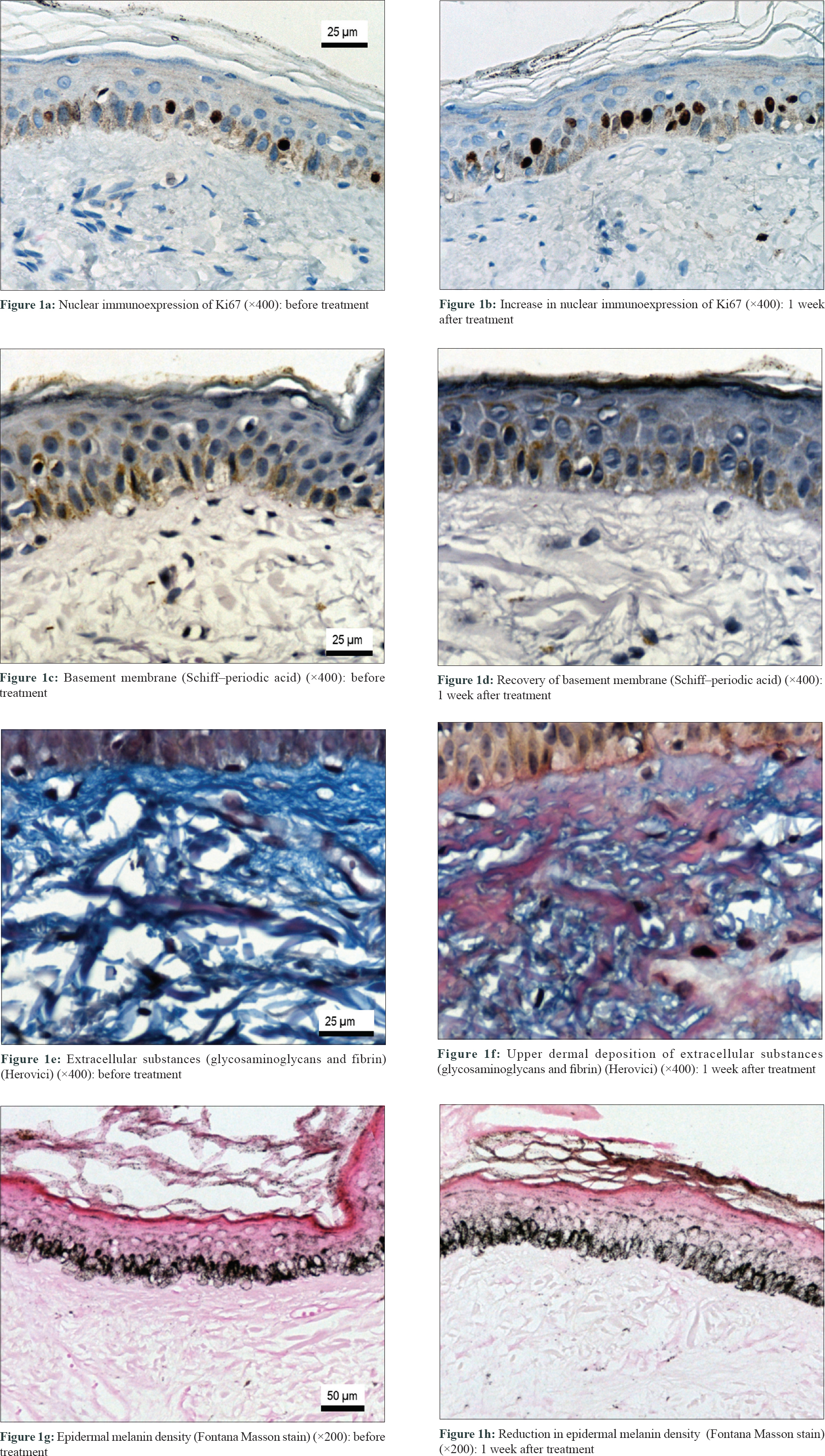 |
| Figure 1: |
This pilot study demonstrated that gentle microneedling promoted early changes in epidermis and upper dermis that led to reverse some structural patterns in melasma, substantiating its clinical improvement. The indications of microneedling are widening in dermatology, especially in inducing neocollagenesis.[4],[5] However, its effects on the epidermis regarding the increase in keratinocyte proliferation and basement membrane restoration have been rarely explored.
As micro needling causes little epidermal damage, it hastens skin recovery and limits the risks of infection, post inflammatory pigmentation and scarring, while stimulating upper dermal wound healing. There is fibroblast proliferation, fibronectin deposition, neocollagenesis, and the release of growth cytokines related to repair.[4] The restructuring of upper dermis, basement membrane and increase in epidermal turnover disfavor the contact of melanocytes with dermal released melanogenic stimuli like endothelins, stem-cell factor, and hepatocyte growth factor as well as promote an increase in the clearance of epidermal melanin.[2]
The main limitations of the study were the modest sample size and the short follow-up, which did not hinder the detection of changes. Further, randomized controlled studies comparing sunscreens, triple-combination agents, oral tranexamic acid and microneedling to explore the role of each treatment regimen in clinical and histological improvement of melasma is warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
FAPESP (2018/10827-3).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kwon SH, Hwang YJ, Lee SK, Park KC. Heterogeneous pathology of melasma and its clinical implications. Int J Mol Sci 2016;17. pii: E824.
[Google Scholar]
|
| 2. |
Lima EV, Lima MM, Paixão MP, Miot HA. Assessment of the effects of skin microneedling as adjuvant therapy for facial melasma: A pilot study. BMC Dermatol 2017;17:14.
[Google Scholar]
|
| 3. |
Lima Ede A. Microneedling in facial recalcitrant melasma: Report of a series of 22 cases. An Bras Dermatol 2015;90:919-21.
[Google Scholar]
|
| 4. |
Alster TS, Graham PM. Microneedling: A review and practical guide. Dermatol Surg 2018;44:397-404.
[Google Scholar]
|
| 5. |
Cohen BE, Elbuluk N. Microneedling in skin of color: A review of uses and efficacy. J Am Acad Dermatol 2016;74:348-55.
[Google Scholar]
|
Fulltext Views
8,756
PDF downloads
2,443





