Translate this page into:
Early-onset sarcoidosis and juvenile idiopathic arthritis:A diagnostic dilemma
2 Department of Dermatology, Gauhati Medical College and Hospital, Guwahati, Assam, India
3 Department of Medicine, Assam Medical College and Hospital, Dibrugarh, Assam, India
Correspondence Address:
Kumud Agarwal
Department of Dermatology, Assam Medical College and Hospital, Dibrugarh - 786 002, Assam
India
| How to cite this article: Agarwal K, Barua S, Adhicari P, Das S, Marak R. Early-onset sarcoidosis and juvenile idiopathic arthritis:A diagnostic dilemma. Indian J Dermatol Venereol Leprol 2016;82:542-545 |
Sir,
Early-onset childhood sarcoidosis occurs commonly in children below 5 years with a classical triad of skin rash, uveitis and arthritis. In older children, the disease is almost similar to the adult form with frequent pulmonary involvement and lymphadenopathy associated with fever, malaise and weight loss.[1]
A 7-year-old girl presented with a history of redness and scaling almost all over the body for 10 months. There was boggy swelling of the elbow, wrist, ankle and knee joints for the last 6 months associated with deformity of the small joints of the hands and feet [Figure - 1] and [Figure - 2]. She also had diminution of vision of the left eye with opacity of the peripheral part of the cornea. She initially attended the outpatient departments of pediatrics and rheumatology, and an initial diagnosis of juvenile idiopathic arthritis (previously known as juvenile rheumatoid arthritis) was made. The patient was treated with oral corticosteroids. There was no history of fever, dyspnea, chest pain, abdominal pain, muscle weakness or photosensitivity. The family history was unremarkable.
 |
| Figure 1: Skin-colored papular lesions on bilateral distal upper extremities with multiple deformities of the interphalangeal joints |
 |
| Figure 2: Boggy swelling of bilateral knee joints |
On examination, there was erythema and small off-white adherent scales present all over the body. The skin was xerotic with ichthyosiform lesions on the lower legs. There were a few grouped, tiny, flat-topped scaly papules around the bilateral knee joint and the upper third of both thighs [Figure - 1] and [Figure - 2].
After 8-weeks of irregular therapy with oral corticosteroids, the erythema and scaling decreased but tiny. Flat-topped papular lesions appeared all over the body while there was little improvement in joint swelling and vision. Ocular examination revealed anterior uveitis with visual acuity reduced to light perception in the left eye.
All routine laboratory investigations were normal. Antinuclear antibodies, rheumatoid factor and anti-cyclic citrullinated peptide (CCP) antibody were negative. Serum angiotensin-converting enzyme was 110 U/L (normal 8–65 U/L). The chest radiograph was normal and radiographs of bilateral hands and knee joints revealed narrowing of joint spaces with no destructive changes. Skin biopsy from the papular lesions on thigh revealed multiple non-caseating epithelioid granulomas with a paucity of lymphocytes in the dermis [Figure - 3] and [Figure - 4]. Special stains for fungi and mycobacteria were negative. A synovial biopsy from the knee joint showed non-specific inflammation without epithelioid granulomas.
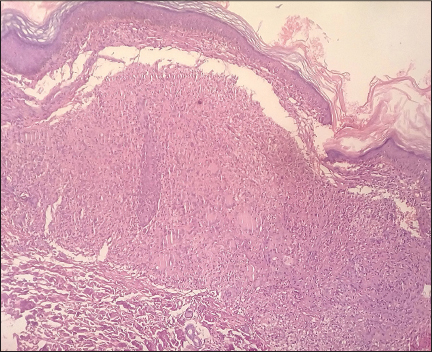 |
| Figure 3: Multiple non-caseating epithelioid granulomas with paucity of lymphocytes in the dermis (H and E, ×100) |
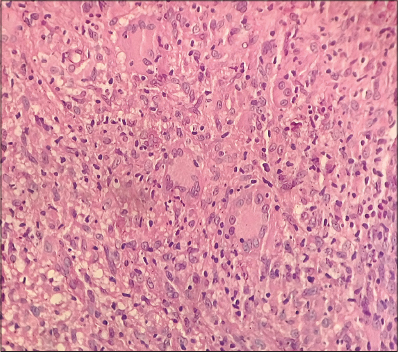 |
| Figure 4: Multiple Langhans giant cells (H and E, ×400) |
The patient was treated with systemic corticosteroids at a dose of 1 mg/kg body weight, tapered to 0.5 mg/kg after 4 weeks and gradually tapered off thereafter. Subsequently methotrexate was added at a dose of 0.5 mg/kg body weight. The skin lesions responded well, with a decrease in the size and number and the joint swelling improved considerably but there was no change in the ocular symptoms.
Sarcoidosis and juvenile idiopathic arthritis are both multisystem disorders with poorly understood etiologies. The diagnosis of juvenile idiopathic arthritis depends on the history, clinical features and radiological findings. For both disease entities, the diagnosis is one of exclusion. Juvenile idiopathic arthritis is a disease or group of diseases characterized by chronic synovitis and is associated with a number of extra-articular manifestations. Almost 90–95% of patients are rheumatoid factor-negative while rheumatoid factor-positive juvenile idiopathic arthritis occurs in late childhood and resembles adult-onset rheumatoid arthritis.[2]
Early-onset sarcoidosis tends to be underdiagnosed as it closely mimics systemic-onset juvenile idiopathic arthritis. The skin involvement in juvenile idiopathic arthritis is a transient erythematous macular rash whereas sarcoidosis can present with varied skin eruptions including erythema, papules, plaques and ichthyosiform lesions.[3] As skin lesions may appear before joint or eye involvement, an early skin biopsy may help arrive at a definitive diagnosis.
Juvenile idiopathic arthritis can be clinically distinguished from sarcoid arthritis in children. Large, painless, boggy synovial and tendon sheath effusions with little limitation of motion characterize sarcoid arthritis; in contrast, joint involvement in juvenile idiopathic arthritis presents with pain, limitation of movement and destructive changes on radiographs. However, the signs and symptoms of joint involvement in sarcoidosis may become more like those of juvenile idiopathic arthritis during its clinical course. The eye is commonly involved in both diseases. Anterior uveitis is a frequent finding in early-onset sarcoidosis and may present as keratic precipitates, iris nodules and focal posterior synechiae; in contrast, uveitis, which rarely occurs in juvenile idiopathic arthritis, involves the posterior compartment of the eye.
Yotsumoto et al. and Sahn et al. also reported similar cases of early-onset sarcoidosis with the classical triad of the eye and joint involvement with papular skin lesions showing non-caseating granulomas on histopathology.[4],[5]
Early-onset sarcoidosis being a rare entity, a high index of clinical suspicion is required for early diagnosis and it must be differentiated from juvenile idiopathic arthritis. Skin lesions provide an early clue in differentiating the two diseases and a skin biopsy may provide a definite early diagnosis as in our case. The peculiarity of our case is that the onset was around 6 years of age while the previous articles that we found reported an onset earlier than 4 years of age.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hoffmann AL, Milman N, Byg KE. Childhood sarcoidosis in Denmark 1979-1994: Incidence, clinical features and laboratory results at presentation in 48 children. Acta Paediatr 2004;93:30-6.
[Google Scholar]
|
| 2. |
Schaller JG. Juvenile rheumatoid arthritis. In: Nelson WE, Behrman RE, Kliegman RM, Arvin AM, editors. Nelson Textbook of Paediatrics. 15th ed. Philadelphia: WB Saunders; 1996. p. 661-70.
[Google Scholar]
|
| 3. |
Paller AS, Roenigk AH Jr., Caro WA. Extensive ichthyosiform sarcoidosis in a patient with juvenile rheumatoid arthritis. Arch Dermatol 1985;121:171-2.
[Google Scholar]
|
| 4. |
Yotsumoto S, Takahashi Y, Takei S, Shimada S, Miyata K, Kanzaki T. Early onset sarcoidosis masquerading as juvenile rheumatoid arthritis. J Am Acad Dermatol 2000;43 (5 Pt 2):969-71.
[Google Scholar]
|
| 5. |
Sahn EE, Hampton MT, Garen PD, Warrick J, Smith D, Silver RM. Preschool sarcoidosis masquerading as juvenile rheumatoid arthritis: Two case reports and a review of the literature. Pediatr Dermatol 1990;7:208-13.
[Google Scholar]
|
Fulltext Views
3,392
PDF downloads
1,047





