Translate this page into:
Ectopic extramammary Paget's disease on the face
2 Department of Pathology, School of Medicine, Pontificia Universidad Cat�lica de Chile, Chile
Correspondence Address:
Echeverr�a Ximena
Vicu�a Mackenna, Macul, Santiago
Chile
| How to cite this article: Ximena E, del Puerto C, Mario P, Sergio G. Ectopic extramammary Paget's disease on the face. Indian J Dermatol Venereol Leprol 2012;78:760-762 |
Sir,
In 1989 Crocker described Extramammary Paget′s Disease (EMPD) as a skin apocrine gland neoplasm. However, ectopic EMPD (E-EMPD) at skin places lacking apocrine glands has been described. [1]
There are 29 cases of E-EMPD reported in English and Japanese literature. [1] We describe a new case.
A 76 year-old woman with hypertension and dyslipidemia came to our center because of an itchy, erythematous-skin colored lesion on her right cheek that has been slowly enlarging since the last year. The patient noticed that the lesion appeared after a wax-depilation burn. Physical examination showed an erythematous star-shaped macule of size 25 × 20 mm on her cheek [Figure - 1] and an atypical nevus on her leg. Actinic keratosis, Bowen′s disease, and in situ melanoma were suspected so excisional biopsies were performed.
 |
| Figure 1: Ectopic extramammary Paget's disease. Star shaped, erythematous plaque of 20 × 25 mm on her left cheek |
Histological study concluded in situ melanoma on the leg; and histological examination of cheek′s macule showed intraepithelial accumulation of large cells, with eosinophilic cytoplasm, vesicular nucleus and prominent nucleolus [Figure - 2]a. In the dermis there was a superficial infiltrate of lymphocytes and plasmocytes. On immunohistochemistry epidermal cells were cytokeratin 7 (Ck7) positive [Figure - 2]b and carcinoembryonic antigen (CEA) and cytokeratin 20 (Ck20) negative. The adnexal structures were preserved. Histopathological findings were consistent with E-EMPD therefore a wide margin excision was performed.
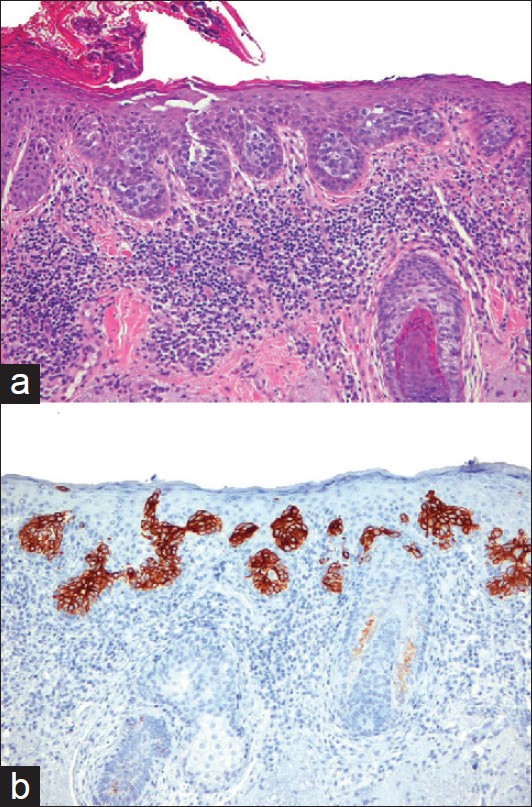 |
| Figure 2: (a) Ectopic extramammary Paget's disease on the face. Intraepithelial big cells accumulate, with eosinophilic cytoplasm, vesicular nucleus, and prominent nucleolus. Adnexal structures were preserved. (H and E stain, x 200). (b) Ectopic Extramammary Paget's Disease on the face. Infiltrating cells stain positive for CK7 (200 x) |
Gynecological examination, mammography, upper and lower endoscopy and laboratory tests excluded an internal neoplasm. After four months of follow up, no recurrences have been detected.
EMPD is considered as an intraepithelial adenocarcinoma. It affects elderly people, with a mean age of 67.9 years. [1] It affects more frequently women than men. [2] It′s most common locations are first the vulva [2] and secondly the perineum. [3] Its etiology is unknown. However, some authors believe E-EMPD would be secondary to an abnormal transformation of skin stem cells, producing abnormal keratinocytes with apocrine markers at locations that usually lack apocrine glands. [1]
Although no predisposing factors have been reported, our case had a clear correlation with local burn, which suggests that local trauma may trigger EMPD.
EMPD presents as an erythematous, hypo pigmented or skin colored plaque [1],[3] which may be pruritic (73%), [3] eczematous or asymptomatic; 49% has an erosion or ulceration. [3] Because of its nonspecific clinical manifestations, mean delay in diagnosis ranges from 1 to 3 years. [3] Histologically EMPD is an intraepithelial infiltration of Paget′s cells with glandular differentiation. [1] The cells invade epidermis and rarely the dermis. [3] EMPD present a lymphocytic infiltrate in upper dermis. [4]
Differential diagnosis of intraepidermal malignancies with pagetoid cells include EMPD, Pagetoid Bowen′s Disease (pBD) and pagetoid in situ melanoma (pISM). [4] These entities can′t be distinguished just by clinical characteristics, therefore histology and immunohistochemistry are mandatory to make the correct diagnosis.
On histology, pBD present single pagetoid cells with intercellular communicating bridges; and cells with maturation defects at all levels of epidermis. [4] pBD does not present lymphocytic infiltrates in dermis. [4] EMPD does not involve all epidermal levels and it′s cells does not have intercellular bridges. [4] EMPD paget′s cells may be seen in stratum corneoum, which are not found in pBD. [4] Finally, pISM present follicular involvement. [4]
Immunohistochemical differences are detailed in [Table - 1]. EMPD cells stain positive for CEA and Ck7, and negative S-100 protein, Ck10. [5] Contrary to EMPD, pBD cells stain positive for Ck10 but negative for CEA and Ck7; and pISM are S-100 and HMB-45 positive but negative for CK7 and CK10. [5]
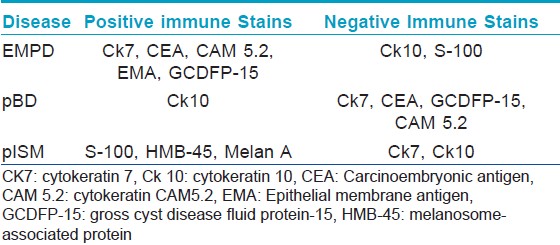
However, cases of pBD positive for CK7 and cases of EMPD that do not stain for CEA have been described. [4],[5] Therefore it is mandatory to make an immune profile with all markers and correlate this with histological findings. [5]
Other entities may occasionally present pagetoid differentiation: sebaceous carcinoma, malignant eccrine poroma, trichilemmal carcinoma, pagetoid dyskeratosis and epidermotropic carcinoma. [4]
Regarding our case, findings were suggestive of EMPD because there were pagetoid cells in the stratum corneum, a lymphocytic infiltrate in the upper dermis, no adnexal involvement; and finally cells stained Ck7 (+). To our knowledge, this is the third reported case of EEMP arising on the face. [6],[7]
Although Paget′s disease (PD) and EMPD share histological morphology, probably they′re two different entities and consequently their association with neoplasms is different. In fact, while 100% of PD cases present internal neoplasm, the association of EMPD with internal neoplasms is much lower (16- 48%). [1],[3]
First line treatment is surgery. Mohs surgery is the best choice and wide margin excision is the second. [8] Medical therapies include topical 5 FU, bleomycin, 5% imiquimod, CO 2 laser ablation and radiotherapy. [1],[8]
EMPD has good prognosis, with overall survival similar to general population. [1],[3] However, prognosis worsens when EMPD infiltrates dermis and lymphatics, has increased CEA or an internal malignancy. [1],[8]
| 1. |
Sawada Y, Bito T, Kabashima R, Yoshiki R, Hino R, Nakamura M, et al. Ectopic extramammary Paget's disease: Case report and literature review. Acta Dermatol Venereol 2010;90:502-5.
[Google Scholar]
|
| 2. |
Banerjee S, Chatterjee M, Chand K. Extramammary Paget' disease. Indian J Dermatol Venereol Leprol 2005;71:417-20.
[Google Scholar]
|
| 3. |
Pierie JP, Choudry U, Muzikansky A, Finkelstein DM, Ott MJ. Prognosis and management of extramammary Paget's disease and the association with secondary malignancies. J Am Coll Surg 2003;196:45-50.
[Google Scholar]
|
| 4. |
Williamson JD, Colome MI, Sahin A, Ayala AG, Medeiros LJ. Pagetoid bowen disease: A report of 2 cases that express cytokeratin 7. Arch Pathol Lab Med 2000;124:427-30.
[Google Scholar]
|
| 5. |
Aslan F, Demirkesen C, Caðatay P, Tüzüner N. Expression of cytokeratin subtypes in intraepidermal malignancies: A guide for differentiation. J Cutan Pathol 2006;33:531-8.
[Google Scholar]
|
| 6. |
Cohen MA, Hanly A, Poulos E, Goldstein GD. Extramammary Paget's disease presenting on the face. Dermatol Surg 2004;30:1361-3.
[Google Scholar]
|
| 7. |
Chilukuri S, Page R, Reed JA, Friedman J, Orengo I. Ectopic extramammary Paget's disease arising on the cheek. Dermatol Surg 2002;28:430-3.
[Google Scholar]
|
| 8. |
Chiu TW, Wong PS, Ahmed K, Lam SC, Ying SY, Burd A. Extramammary Paget's disease in Chinese males: A 21-year experience. World J Surg 2007;31:1941-6.
[Google Scholar]
|
Fulltext Views
4,933
PDF downloads
2,582





