Translate this page into:
Effect of intravenous pulse dexamethasone versus daily oral prednisolone on bone mineral density in dermatology patients: Is it a site-specific response?
2 Department of Radiodiagnosis, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Sanjeev Handa
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Sector 12, Chandigarh - 160 012
India
| How to cite this article: Handa S, Singh G, Arora AK, Khandelwal N, Gupta V. Effect of intravenous pulse dexamethasone versus daily oral prednisolone on bone mineral density in dermatology patients: Is it a site-specific response?. Indian J Dermatol Venereol Leprol 2018;84:174-178 |
Abstract
Background: The use of glucocorticoids in various forms of administration is complicated by their systemic side effects. Although intravenous pulse therapy is considered to have lesser systemic side effects, there are few studies in literature comparing the effects of intravenous pulse glucocorticoids versus oral daily glucocorticoids on bone mineral density.Aim: To compare the effects of intravenous pulse glucocorticoids and oral daily glucocorticoids on bone mineral density with the aim of finding any site-specific osteopenic side effect.
Methods: The study was conducted by the department of dermatology of Postgraduate Institute of Medical Education and Research, Chandigarh, India. The study comprised of two groups of patients. Group A consisted of 28 patients with pemphigus vulgaris who received intravenous pulses of dexamethasone at 4 weekly intervals. Group B consisted of 21 patients with airborne contact dermatitis who received oral daily prednisolone therapy. All the patients had a dual X-ray absorptiometry scan at baseline, and at 3 and 6 months of follow-up. The results were analyzed as changes in bone mineral density.
Results: There was loss of bone mineral density at lumbar spine and the head of radius in both the groups. At the lumbar spine, Group B showed more reduction in bone mineral density at 3 months whereas in Group A it was more at the head of radius. In patients on oral steroids, the lumbar spine was significantly more affected than the head of radius at both 3 and 6 months of follow-up. However, in patients on intravenous pulse steroids, both the sites were equally affected at 3 and 6 months.
Limitations: In our study, we used different glucocorticoids in the two groups: prednisolone in the oral daily group and dexamethasone in the intravenous pulse steroids group. A similar reduction in bone mineral density in both the groups may have been due to a longer half-life or more bone-directed side effects of dexamethasone as compared to prednisolone.
Conclusion: Dermatologists need to be aware of the detrimental effects of high-dose intravenous pulsed glucocorticoids on bone mineral density and assessment of this parameter should be done before the initiation of therapy and also at regular intervals thereafter. During follow up, either the lumbar spine or the head of radius can be used to assess the osteopenic effect of intravenous pulse steroids, whereas the lumbar spine is a better site for this evaluation in patients on oral steroids.
Introduction
Dermatologists, along with rheumatologists and pulmonologists, are among the leading prescribers of systemic glucocorticoids in the world. The efficacy of glucocorticoids is well known, but their use is associated with numerous adverse effects. The most predictable and debilitating of these adverse effects is rapid loss of bone mineral density, with an increase in osteoporotic fracture risk, particularly on long-term use. The intravenous pulse form of glucocorticoids came into clinical practice to minimize the adverse effects of daily systemic glucocorticoids. A decreased incidence of common side effects such as weight gain, Cushingoid obesity, diabetes mellitus and hypertension makes intravenous pulse administration more acceptable to the patient.[1] In this study, we compared the effects of these two routes of steroid administration on bone mineral density and tried to identify whether the response was site specific.
Methods
Ethical clearance was obtained from the Ethical Committee of our Institute. The study comprised of two groups of patients recruited from the outpatient department of dermatology of Postgraduate Institute of Medical Education and Research, Chandigarh, India. Twenty-eight patients with pemphigus vulgaris on intravenous pulse dexamethasone (140 mg for 3 consecutive days at 4 weekly intervals) were assigned to Group A, and 21 patients with airborne contact dermatitis on oral daily prednisolone (at a dose calculated according to patient's body weight and tapered according to response) were assigned to Group B. The patients in the intravenous steroid group were not given intermittent oral steroids and were managed with steroid-sparing immunosuppressants such as azathioprine and cyclophosphamide, as and when required. The patients in both the groups were matched for age and sex. However, matching for mobility, physical activity and occupation could not be done due to practical difficulties. Postmenopausal women, pregnant women, patients with osteoporosis or with a low bone mineral density (T-scores ≤2.5 at baseline dual X-ray absorptiometry scan), patients on treatment with drugs which could affect bone metabolism such as bisphosphonates, calcitonin, hormone supplements, methotrexate, cyclosporine, lithium and antiepileptic drugs in the preceding 6 months, and patients who had taken >7.5 mg/day of prednisolone or its equivalent for >3 months during the past 6 months or who had taken vitamin D or calcium supplements, were all excluded from the study.
Informed consent was taken from all the patients before recruitment into the study. Detailed clinical history and examination were recorded. Baseline investigations including serum albumin, calcium, phosphate, alkaline phosphatase, thyroid-stimulating hormone, T3 and T4 were done. All women in reproductive age group had to undergo a urine pregnancy test before dual X-ray absorptiometry scan.
All patients had dual X-ray absorptiometry scan at baseline, at 3 months and at 6 months of starting treatment and bone mineral density was measured at the lumbar spine and the head of radius [Figure - 1] and [Figure - 2]. Dual X-ray absorptiometry scan was performed using Norland dual X-ray absorptiometry scanner ( first generation), which uses Samarium filter producing a pencil beam to give energy peaks at 46.8 keV and 80 keV. Two sodium iodide scintillation detectors 0.3 mm and 7.0 mm thick were used. The data were expressed as bone mineral density (g/cm [2]), T- and Z-scores. T-score is defined as individual bone mineral density values compared to those in a young healthy adult matched for race and gender. Osteoporosis, as per the WHO guidelines, is defined as a T-score ≤−2.5. Z-scores are defined as individual bone mineral density values compared to those of an age-matched population that is also matched for race and gender. The results were analyzed as a change of bone mineral density (change of T- and Z-score) as compared to baseline within each group. Furthermore, among the two sites, the site at which reduction in bone mineral density occurred at the earliest was identified. The results were analyzed using Statistical Product and Service Solutions (SPSS) version IBM SPSS Statistics 22.0. (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: USA; IBM Corp.)
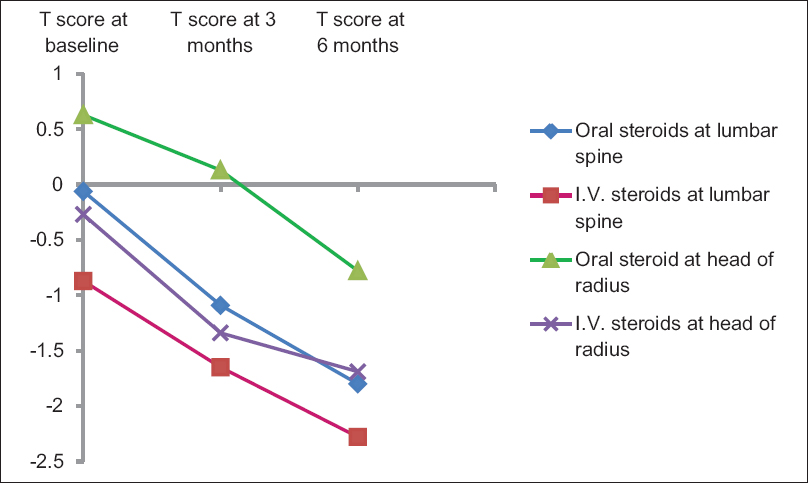 |
| Figure 1: Trends of fall in bone mineral density in the oral corticosteroid and intravenous pulse steroid groups at lumbar spine and head of radius |
 |
| Figure 2: Bar chart demonstrating the site specificity of osteopenic effect of oral steroids and intravenous pulse steroids |
Results
The patients in Group A were given a total cumulative dose of 2520 mg of dexamethasone (equivalent to 16,800 mg of prednisolone). The mean cumulative dose in Group B was 6308.57 ± 1342.75 mg of prednisolone with a mean dose of 35 ± 7.45 mg/day.
The mean T- and Z-score at baseline, at 3 months and at 6 months in both the groups is given in [Table - 1]. The mean change of T- and Z-score at lumbar spine and head of radius for both the groups is given in [Table - 2] and [Table - 3]. At 3 months of therapy, the fall in T-score at lumbar spine was significantly more in patients on daily oral steroids (P = 0.049), whereas at the head of radius, it was more in patients on intravenous pulse glucocorticoids (P < 0.001) as shown in [Figure - 1]. At 6 months, however, there was no statistically significant difference between the two groups in the magnitude of reduction of T-score at either site (P > 0.05).



A comparison of change in T- and Z-score at 3 and 6 months for either treatment group at lumbar spine and the head of radius is given in [Table - 4] and [Table - 5]. Patients on daily oral prednisolone had a significantly greater reduction of T-score at the lumbar spine as compared to the head of radius at 3 and 6 months (P < 0.001; P = 0.016), whereas patients on intravenous pulse glucocorticoids, had a comparable reduction in T-score at 3 and 6 months at both the lumbar spine and the head of radius (P > 0.05) as shown in [Figure - 2].


Discussion
Glucocorticoid-induced osteoporosis is a leading cause of secondary osteoporosis and is a major risk factor for fractures. Even doses of 7.5 mg/day of oral glucocorticoids have resulted in a rapid reduction of bone mineral density as early as 3 months after the commencement of therapy.[2] Although there are various studies, especially by pulmonologists and rheumatologists, establishing the osteoporotic effect of oral corticosteroids, studies reporting the osteoporotic side effects of intravenous pulse steroids are scarce.[3],[4] Loss of bone mineral density has been observed at various skeletal sites of the body, but it is most marked at lumbar spine, perhaps, as it is a metabolically active trabecular bone.[5],[6] The results of our study indicate that 3 months after the commencement of treatment, the lumbar spine shows a higher degree of bone mineral density loss in patients on oral glucocorticoids whereas the head of radius is affected more by intravenous pulse glucocorticoids. However, at the end of 6 months, the degree of reduction in bone mineral density at both the sites is similar for both oral and intravenous pulse glucocorticoids. When comparing the two treatment modalities, it was found that oral steroids caused a significantly greater reduction in bone mineral density at the lumbar spine as compared to the head of radius both at 3 and 6 months, while intravenous pulse glucocorticoids affected both the sites equally. This suggests that either of these two sites, that is, lumbar spine or the head of radius, can be used to assess the reduction in bone mineral density in patients on intravenous pulse glucocorticoids, however, the lumbar spine is a more sensitive site to detect the osteoporotic adverse effects of oral glucocorticoids.
Our results are in agreement with the study by Salem et al. who compared daily oral prednisolone (mean: 24.79 ± 18.47 g) with intravenous dexamethasone pulse therapy (mean 5.43 ± 2.08 g dexamethasone; 37.46 ± 14.35 g of prednisolone).[6] They found that after 6 months of respective therapies, a significant reduction in bone mineral density occurred in both the groups, however, oral corticosteroids produced a statistically significant reduction in bone mineral density at the lumbar spine which was greater than that at the left hip and the head of radius, whereas intravenous pulsed glucocorticoids produced a statistically significant reduction in bone mineral density of a similar magnitude at all the three sites. In the same study, in the oral glucocorticoids group, reduction in the bone mineral density of trabecular bones such as lumbar spine was not found to be affected by the cumulative doses of corticosteroids, while that of cortical bones had an inverse correlation with the cumulative dose. However, the duration of daily oral corticosteroid intake, or the number of intravenous dexamethasone pulses did not correlate directly with the osteoporotic effect observed.
Various studies in the past, which established the safety of intravenous pulse glucocorticoids in relation to osteoporosis, relied on various different markers for assessment of bone and calcium metabolism, such as serum calcium, parathyroid hormone, vitamin D, alkaline phosphatase, osteocalcin and urinary excretion of calcium, hydroxyproline, deoxypyridinoline and pyridinoline. They did not measure the bone mineral density by any densitometric technique.[7],[8],[9] Such studies, therefore, cannot be fully relied upon. However, there are some studies which have measured bone mineral density and these have advocated the relative safety of intravenous pulse glucocorticoids with respect to osteoporosis.[10],[11]
In a study by Dovio et al., intravenous pulse methylprednisolone in a dose of 15 mg/kg/day was given for 10 days to 13 patients of multiple sclerosis.[10] They concluded that even though high-dose, short-term intravenous glucocorticoid regimens cause an immediate and persistent decrease in bone formation and a rapid and transient increase in bone resorption, these parameters return to baseline values within 6 months. However, intravenous pulse glucocorticoids are not used for such short durations by dermatologists but as monthly pulses usually prolonged over a year and a half. Therefore, it is difficult to comment if the conclusions by Dovio et al. hold true for intravenous pulse glucocorticoids as used in dermatology.
Similarly, in a study by Frediani et al., on patients with rheumatoid arthritis, daily oral methylprednisolone was compared to intravenous methyprednisolone pulse therapy (with a mean interval of 76 days between each pulse) over 1 year.[11] Their study showed a significant reduction in the bone mineral density at lumbar spine at 6 and 12 months in the oral group as compared to the intravenous group, even though the average yearly dose of intravenous pulse methylprednisolone was 18.9 g (equivalent to 23.4 g prednisolone) which was greater than that used by us. Again, this scenario is not comparable to the usual routine of intravenous pulse glucocorticoids followed by dermatologists where pulses are given every 28 days, which is less than half of the mean interval between pulses given by Frediani et al. A longer inter-pulse interval, as used in the latter study, might give the bones some time to regenerate.[11]
Conclusion
Our study aims to emphasize that high doses of intravenous pulse glucocorticoids do cause reduction in bone mineral density, at both the lumbar spine and the head of radius, and the magnitude of reduction is similar to that seen in patients taking daily oral glucocorticoids. Dermatologists need to be aware of the detrimental effects of high-dose intravenous pulse glucocorticoids on bone mineral density and its baseline and periodic assessment should be considered wherever long-term therapy is indicated. Prophylactic treatment against osteoporosis in the form of calcium supplements and bisphosphonates is essential for patients receiving corticosteroids orally as well as for those on intravenous pulse therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Victoria PW. Systemic glucocorticoids. In: Wolff K, Goldsmith LA, Katz SI, Gilshrist BA, Paller AS, Leffel DJ, editors. Fitzpatrick's Dermatology in General Medicine., New York: McGraw Hill; 2008. p. 2147-53.
[Google Scholar]
|
| 2. |
Kaur S, Kanwar AJ. Dexamethasone-cyclophosphamide pulse therapy in pemphigus. Int J Dermatol 1990;29:371-4.
[Google Scholar]
|
| 3. |
Li EK, Tam LS, Young RP, Ko GT, Li M, Lau EM. Loss of bone mineral density in Chinese pre-menopausal women with systemic lupus erythematosus treated with corticosteroids. Br J Rheumatol 1998;37:405-10.
[Google Scholar]
|
| 4. |
Jardinet D, Lefèbvre C, Depresseux G, Lambert M, Devogelaer JP, Houssiau FA. Longitudinal analysis of bone mineral density in pre-menopausal female systemic lupus erythematosus patients: Deleterious role of glucocorticoid therapy at the lumbar spine. Rheumatology (Oxford) 2000;39:389-92.
[Google Scholar]
|
| 5. |
Canalis E, Giustina A. Glucocorticoid-induced osteoporosis: Summary of a workshop. J Clin Endocrinol Metab 2001;86:5681-5.
[Google Scholar]
|
| 6. |
Salem D, Talaat S, Abdel-Halim MR, Mohsen KM. Assessment of bone mineral density by dual x-ray absorptiometry in dermatological patients treated by corticosteroids. Indian J Dermatol 2010;55:238-45.
[Google Scholar]
|
| 7. |
Bijlsma JW, Duursma SA, Huber-Bruning O. Bone metabolism during methylprednisolone pulse therapy in rheumatoid arthritis. Ann Rheum Dis 1986;45:757-60.
[Google Scholar]
|
| 8. |
van der Veen MJ, Bijlsma JW. Effects of different regimes of corticosteroid treatment on calcium and bone metabolism in rheumatoid arthritis. Clin Rheumatol 1992;11:388-92.
[Google Scholar]
|
| 9. |
Lems WF, Gerrits MI, Jacobs JW, van Vugt RM, van Rijn HJ, Bijlsma JW. Changes in (markers of) bone metabolism during high dose corticosteroid pulse treatment in patients with rheumatoid arthritis. Ann Rheum Dis 1996;55:288-93.
[Google Scholar]
|
| 10. |
Dovio A, Perazzolo L, Osella G, Ventura M, Termine A, Milano E, et al. Immediate fall of bone formation and transient increase of bone resorption in the course of high-dose, short-term glucocorticoid therapy in young patients with multiple sclerosis. J Clin Endocrinol Metab 2004;89:4923-8.
[Google Scholar]
|
| 11. |
Frediani B, Falsetti P, Bisogno S, Baldi F, Acciai C, Filippou G, et al. Effects of high dose methylprednisolone pulse therapy on bone mass and biochemical markers of bone metabolism in patients with active rheumatoid arthritis: A 12-month randomized prospective controlled study. J Rheumatol 2004;31:1083-7.
[Google Scholar]
|
Fulltext Views
3,607
PDF downloads
2,552





