Translate this page into:
Effectiveness and safety of autologous platelet-rich plasma therapy with total contact casting versus total contact casting alone in treatment of trophic ulcer in leprosy: An observer-blind, randomized controlled trial
2 Department of Pharmacology, Rampurhat Government Medical College, Rampurhat, Birbhum, West Bengal, India
Correspondence Address:
Aparesh Chandra Patra
Department of Dermatology, Bankura Sammilani Medical College, Kenduadihi, Bankura - 722 102, West Bengal
India
| How to cite this article: Saha S, Patra AC, Gowda SP, Mondal N, Rahaman S, Ahmed SK, Debbarma S, Vitthal KP, Sarkar S, Sil A, Das NK. Effectiveness and safety of autologous platelet-rich plasma therapy with total contact casting versus total contact casting alone in treatment of trophic ulcer in leprosy: An observer-blind, randomized controlled trial. Indian J Dermatol Venereol Leprol 2020;86:262-271 |
Abstract
Background: Trophic ulcers secondary to leprosy pose a great stigma to patients and remain a challenge to the treating dermatologists. Platelet-rich plasma (PRP) introduces growth factors directly into the wound and aids in rapid healing. The role of PRP in the treatment of trophic ulcers in leprosy patients has not yet been established by randomized controlled trials.
Aims: To study the effectiveness and safety of autologous PRP therapy with total contact casting versus total contact casting alone in the treatment of trophic ulcers in leprosy.
Methods: In an observer-blind, randomized (1:1) controlled study, 118 patients were enrolled. PRP was prepared by the manual double-spin method (1600 rpm for 10 min followed by 4000 rpm for 10 min). After wound bed preparation, activated PRP was injected intra- and perilesionally, and platelet-poor plasma gel was applied over the ulcer bed. Occlusive dressings and total contact casting were then applied in Group A, and only total contact casting was applied in Group B. The same procedure was repeated every 2 weeks for 8 weeks.
Results: In all, 56 patients were analyzable in Group A and 52 in Group B. The surface area of the ulcer decreased significantly from first follow-up onward in both the groups (P < 0.001 in both the groups). Intergroup comparison showed that the reduction in the surface area of the ulcer was significantly more in Group A than in Group B from the first follow-up onward (P = 0.038) and the difference was maintained till the fifth follow-up (P < 0.001). At the end of the study, 91.10 ± 9.65% ulcer surface area reduction had occurred in Group A, whereas it was 79.77 ± 17.91% in Group B (P < 0.001). Trophic ulcers healed completely more often in paucibacillary leprosy patients (P < 0.001) and in those with a lower initial surface area of the ulcer (P < 0.001).
Limitation: Short duration of treatment (8 weeks).
Conclusion: PRP combined with total contact casting accelerates the healing of trophic ulcers of leprosy and is more effective than total contact casting alone. Complete remission is more likely to occur when the duration and surface area of ulcer are less and in the paucibacillary spectrum.
Introduction
Plantar ulceration is one of the major disabilities that can occur in patients with leprosy. Price introduced the term “plantar,” trophic, or perforating ulcer and defined it as a “chronic ulceration of the anaesthetic sole of the foot, situated in well-defined areas overlying bony prominences, resistant to local or systemic therapy and characterized by a marked tendency to recurrence.”[1] Anesthesia of the foot is the central factor in the pathogenesis of plantar ulcers and an anesthetic foot is said to be “ulcer-liable.” The moment an ulceration occurs, this foot becomes “ulcer-prone” and a vicious cycle of scar-ulcer-scar sets in.[2] Plantar ulcers recur because of plantar anesthesia, walking barefoot, poor quality of scar from previous ulceration, undue load on the scar, and enduring pockets of infection.[3]
Clinicians are faced with the persisting therapeutic challenge of improperly healing neuropathic ulcers in leprosy. Chronic ulcers not only impinge upon patient health, emotional state and quality of life but also lead to out-of-pocket expenses. Healing of these wounds can be slow due to their chronic inflammatory state and senescence of local reparative cells. Offloading pressure from the ulcer is key to successful management of a trophic ulcer.[4] Offloading can be in the form of strict bed rest, use of crutches, wheelchairs, walkers, pressure-reducing measures such as aircushions, waterbeds, plaster boots (total contact casting), removable contact casting, half-shoes, or specialized footwear.[5] Apart from offloading, various methods of treatment have been tried to improve wound healing, for example, saline or collagen dressings, topical phenytoin[6] or metronidazole[7] application, topical growth factors such as platelet-derived growth factor[8] (becalpermin), epidermal growth factor, and other reconstructive surgical procedures. However, all these treatments are not evidence-based. There is a need to find a simple, safe and effective means to reduce the duration of treatment, decreasing the number of dressings and shortening inpatient hospital stay, thereby improving patients' quality of life. One such treatment is the use of platelet-rich plasma (PRP).
Autologous PRP is prepared from the patient's own blood by centrifugation and platelet activation. On application to the wound, it directly introduces growth factors and cytokines, thereby normalizing the metabolic process, promoting neoangiogenesis, improving cellular metabolism, and activating local immunity.[9] There is decreased activity of multiple growth factors in chronic wounds, more so in poorly healing lower leg ulcers, and exogenous delivery of such factors seems a logical strategy. Autologous PRP may restore the healing process, leading to a reparative phase.
Given that the application of autologous PRP has been shown to decrease healing times in various different studies on chronic skin ulcers such as diabetic ulcers, venous leg ulcers, stasis ulcers, claw foot, traumatic ulcers, trophic ulcers, and pressure ulcers, we decided to assess this treatment along with offloading using total contact casting in neuropathic leprosy ulcers.[10],[11] A case report by Conde-Montero et al. on four leprosy ulcers treated by PRP also showed a satisfactory benefit.[12]
Consequently, we have compared the safety and effectiveness of autologous PRP therapy with total contact casting versus total contact casting alone in the treatment of trophic ulcers in leprosy in this observer-blind, randomized controlled trial.
Methodology
The study was designed as a unicentric, observer-blind, randomized controlled trial at the Bankura Sammilani Medical College, a tertiary care center in Bankura, West Bengal. Institutional Ethics Committee permission was obtained prior to the start of the study and written informed consent was obtained from all study participants. The study was done from August 2016 to May 2018.
All consecutive trophic ulcer patients of either sex, age 18–85 years, suffering from clinically diagnosed trophic ulcers due to leprosy located on the plantar, medial, or lateral aspects of the foot (including all toe surfaces), and wound area (length × width) of <10 cm2 attending the dermatology outpatient department were included. Patients with trophic ulcers due to any other etiology (diabetes, peripheral neuropathy, trauma), patients immunocompromised due to drug or disease, pregnant and lactating women, and nonconsenting patients were excluded from the study.
Randomization and blinding
Randomization was done by a computer-generated random number table by balanced unstratified randomization using WINPEPI software ETCETERA version 2.32 (PEPI-for-Windows). Concealment of randomization allocation was done by the sequentially numbered opaque sealed envelopes technique.
The study was rendered observer blind since the assessing physician was different from the treating physician and the former was unaware of the treatment. The patients were counselled not to mention any treatment details to the assessing physician who was seated in a separate room other than the treating physician to keep the blinding in place.
Visits
Screening visit
At the screening visit, patients were enrolled based on inclusion and exclusion criteria, and written informed consent was obtained from them. All patients were referred to the Information Counseling and Testing Centre (ICTC), and only those who were HIV nonreactive were included. A thorough clinical examination was done.
Baseline visit
This visit was done 1 week after the screening visit allowing 1 week as the wash-out period to remove residual effects of prior antibiotic or any other medicine use. The patients were randomized equally into two groups. Group A received autologous PRP therapy with total contact casting and Group B received only total contact casting. Detailed history taking and meticulous clinical examination (palpation of peripheral nerves for thickening and tenderness, appearance of new hypopigmented patches or sensory loss or increase in size of existing lesion) were carried out with reference to the ulcer and activity of Hansen's disease. Multibacillary (MB) or Paucibacillary (PB) status was determined from previous records [patients' treatment card of National Leprosy Eradication Programme (NLEP)] in case of previously treated cases. Laboratory tests (routine hemogram, fasting blood glucose, serum urea, creatinine, and liver function tests) were done. All the patients who were not immunized against tetanus were given injection tetanus toxoid 0.5 mL intramuscularly at this baseline visit. Oral ciprofloxacin 500 mg twice daily was prescribed for 5 days. PRP and total contact casting were done according to randomization. The patients were advised to come after 2 weeks. All the patients had completed the multidrug therapy (MDT) of World Health Organization (WHO) regime and were released from treatment. None of them showed any sign of activity so anti leprosy treatment was not started.
Follow-up visits
Five follow-up visits were carried out at 2 week intervals. In the initial three follow-up visits, active treatment with PRP and total contact casting was done according to randomization. The next two visits were done to evaluate the effect after completion of active treatment. Wound documentation was done by photography. Photographs were not used in assessment of outcome.
Accredited Social Health Activist (ASHA) workers helped in ensuring compliance with follow-up. ASHA workers made house to house visit with help of district leprosy team and helped in compliance.
Treatment procedures
PRP preparation and innoculation
Twenty milliliters of venous blood was collected from the patient under aseptic precautions in centrifuge test tubes labeled with identification data (name and age) and mixed with 2 mL of sodium citrate dextrose. PRP was separated by manual double-spin method at temperature 22°C–26°C.[13] Different researchers have used different rotation speeds for preparing PRP. For example, Anandan et al. used 2000 rpm for the first spin and 300 rpm for the second spin.[14] We tried many combinations and optimized it to 1600 rpm for the first spin and 4000 rpm for the second spin as it yielded the highest platelet concentration according to the piloting performed in the department.
The tube was placed for the first centrifugation at a rate of 1600 rpm for 10 min when plasma was separated; plasma, buffy coat, and upper layers of red blood cells were pipetted into another test tube. This was subjected to a second centrifugation at the rate of 4000 rpm for 10 min. The upper two-third portion was then separated as platelet-poor plasma (platelet-poor plasma; 8 mL) while the lower one-third was taken as PRP (2 mL). About 0.8 mL of calcium gluconate was added to the platelet-poor plasma to form platelet-poor plasma gel.
Total contact casting
After proper debridement of the wound, a dressing was applied over it. Bandaging was done over the whole foot and part of the leg. Roller cotton was applied over the bandage and total contact casting was done by moulding a cast over the entire surface of the roller cotton. Total contact casting was done with window over the ulcer for 8 weeks.
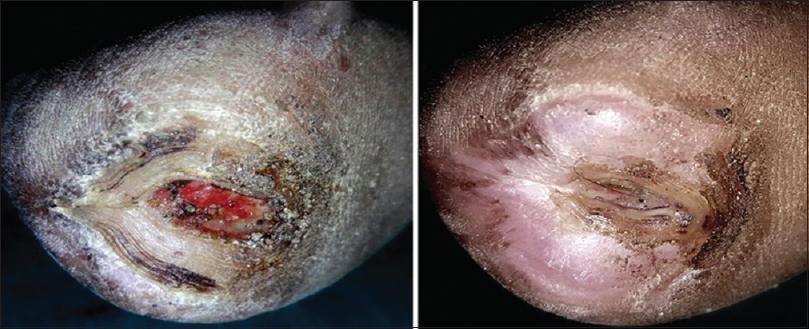
Trial medications and procedures
Group A: After proper debridement of the wound as needed, PRP was injected intra- and perilesionally [Figure - 1], and platelet-poor plasma gel applied over the lesion. Four injections of PRP, 0.5 ml each were given at one point in each quadrant of the ulcer. The injection of PRP was done by using a 2 cc syringe fitted with IM needle (Dispovan™ 2 cc) at the base of the ulcer inserting the needle 0.5 cm away from the edge of the ulcer. Withdrawal technique was followed and the injection was given from inside out. After that, total contact casting was done as described above 30 mins after the injection and gel was applied with window over the ulcer. In subsequent visits, debridement of the ulcer was done through the cast window and PRP injection with platelet-poor plasma gel application was done through the cast window. Aseptic precautions were taken throughout the entire procedure.
 |
| Figure 1: Process of injecting platelet.rich plasma intra. and perilesionally in the ulcer |
Group B: Only total contact casting with window was done. Debridement of the ulcer was done through the window at subsequent visits.
Effectiveness parameters
The primary effectiveness parameter was percentage reduction in ulcer surface area. Ulcer surface area was measured with the help of tracing paper and cm[2] graph paper at each visit. The tracing paper was placed over the ulcer and the margin was marked using a permanent marker. The tracing paper was then immediately placed over a graph paper and the area was calculated. The area was measured at every visit prior to application of platelet-poor plasma gel and PRP injection by the same assessing physician at all visits.
Safety parameters
Vital signs, spontaneously reported adverse events, and those elicited by the clinician were assessed and recorded at each follow-up. Routine hemogram, fasting blood glucose, serum urea, creatinine, and liver function tests were recorded at baseline and at third follow-up, to look for any significant changes.
Statistical analysis
The target sample size was 118, with 59 evaluable subjects in each group. This was calculated using mean reduction in size of 7.022 ± 0.204 mm, null hypothesis value of 7.1 with 80% power, 5% probability of Type 1 error, and considering possible 10% dropouts in a superiority trial.[15] Normality testing was done by D'Agostino-Pearson test. Continuous variables were compared between groups by independent samples t-test and within each group by paired t-test. Mann–Whitney U-test and Wilcoxon's matched pairs signed rank test were used for comparison of unpaired and paired nonparametric data. Friedman's analysis of variance was carried out with nonparametric data for within-group repeated measures comparisons, followed by post hoc Dunn's test. Categorical data were compared between groups by chi-square test or Fisher's exact test, as appropriate. MedCalc version 11.6 (MedCalc Software, 2011; Mariakerke, Belgium) was used for statistical analysis.
Effectiveness analysis was done on a modified intention-to-treat basis with subjects reporting for at least one post-baseline follow-up visit. Missing values were dealt with by the last observation carried forward strategy. Pre- and posttreatment laboratory values were compared in patients for whom both sets of data were available. For other safety analysis, all subjects who had received at least one intervention (essentially all 118 subjects) were considered.
Results
The participant flow is depicted in [Figure - 2]. Of 139 patients screened, 118 were randomized equally into two groups. Each group had 59 participants, of whom 56 were analyzable in Group A and 52 were analyzable in Group B because 10 participants in all were lost to follow-up.
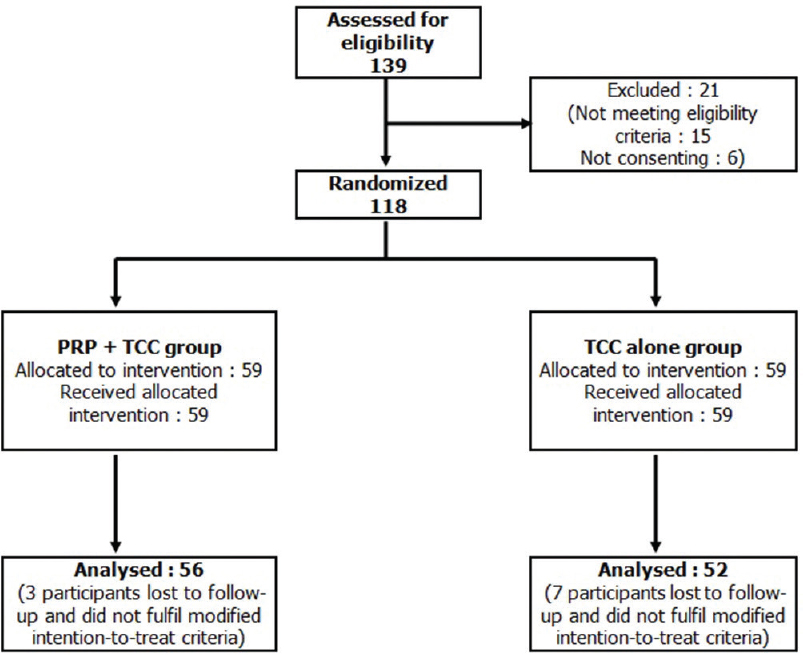 |
| Figure 2: Flowchart of study participants |
Males outnumbered females and patients were mostly in their late 40s (average age, 49.5 ± 8.9 years). Both the groups were comparable with respect to age, sex, residence (rural/urban status), and income (above poverty line/below poverty line). The duration of trophic ulcer was 13.2 ± 8.5 months in Group A and 13.6 ± 7.8 months in Group B, with no significant difference between them (P = 0.51) [Table - 1]. The patients were all treated cases of Hansen's who were released from treatment and clinical examination revealed no sign of activity of the disease; thus MDT was not started.
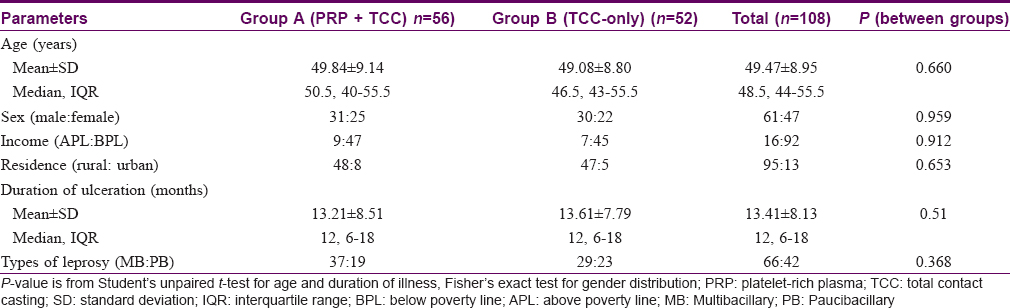
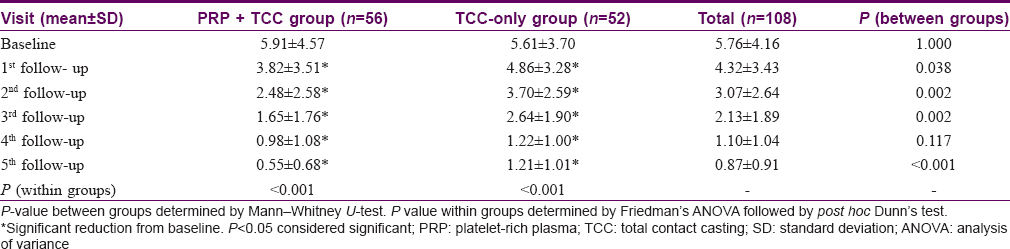
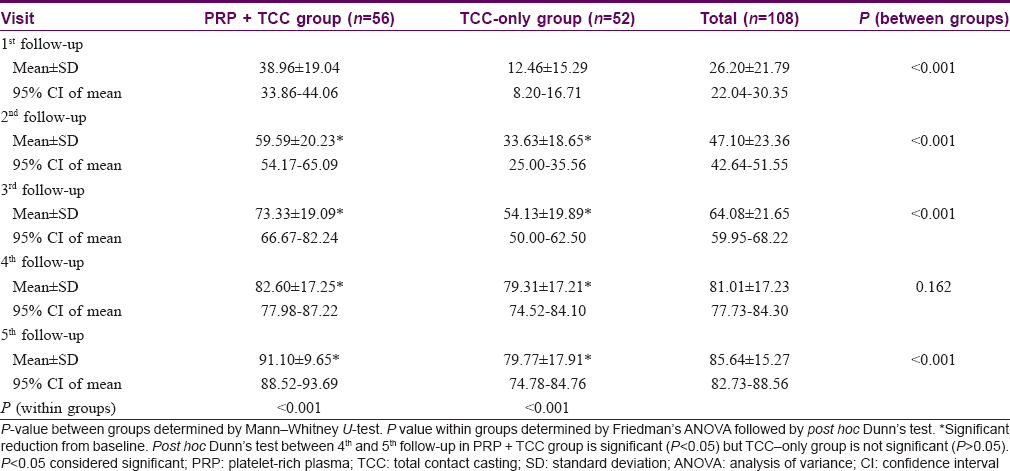
Compared to the baseline, the surface area of ulcers decreased significantly from first follow-up onward in each of the two groups (P < 0.001 in both groups). However, when both the groups were compared, it was found that the reduction in the surface area of the ulcer was significantly more in Group A (PRP + total contact casting) than in Group B (total contact casting alone) from the first follow-up onward (P = 0.038) and this was maintained till the third follow-up (P = 0.002). Although there was no significant difference (P = 0.117) in the mean ulcer surface area between the two groups at fourth follow-up, at fifth follow-up the mean ulcer surface area was again significantly (P < 0.001) less in Group A than Group B which means improvement continued in Group A even after the last treatment session [Table - 2] and [Figure - 3], [Figure - 4], [Figure - 5], [Figure - 6].
 |
| Figure 3: |
 |
| Figure 4: |
 |
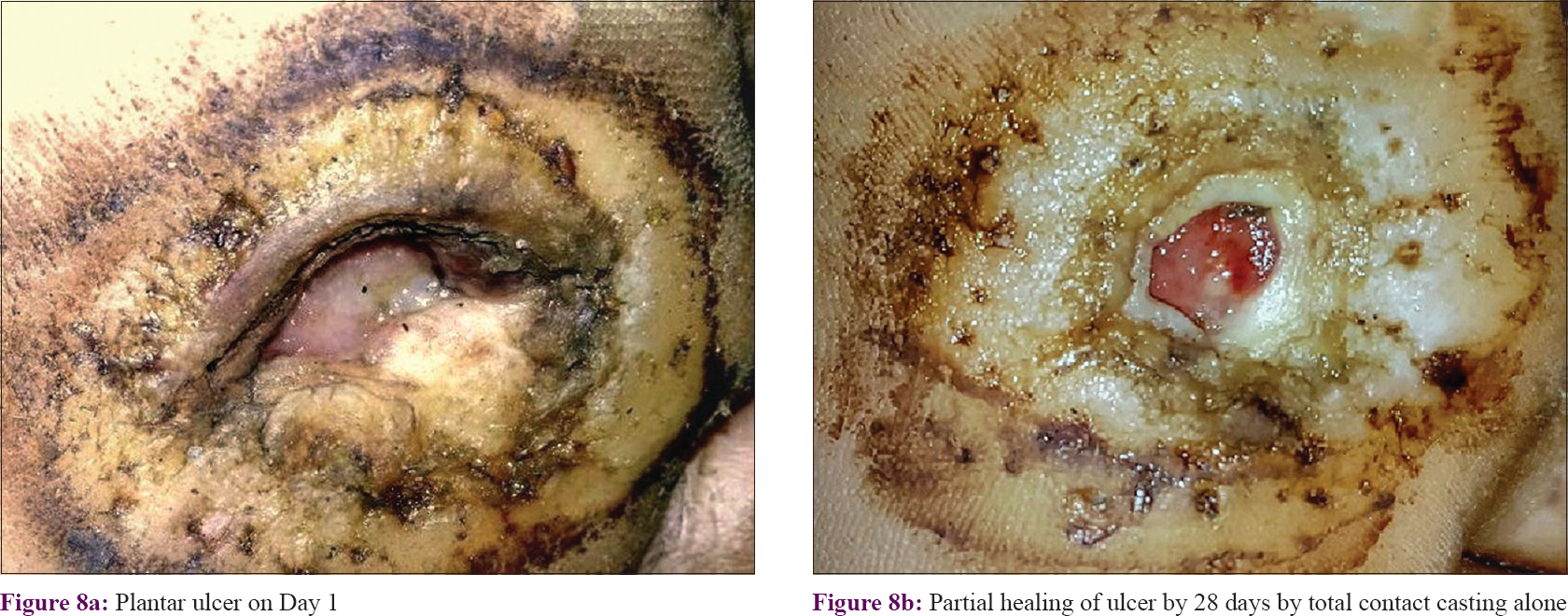
| Figure 5: Complete healing of ulcer by 14 and 28 days with platelet-rich plasma + total contact casting |
 |
| Figure 6: Complete healing of ulcer within 14 days by platelet-rich plasma + total contact casting |
Percentage reduction of surface area involved followed a similar pattern, with significant reductions seen from the second follow-up onward in both the groups. This significant reduction continued in Group A till the fifth follow-up, but in Group B there was no significant improvement after the fourth follow-up [post hoc Dunn's test between fourth and fifth follow-up in PRP + total contact casting group was significant (P < 0.05), but in the total contact casting -only group it was not significant (P > 0.05)]. Intergroup comparison showed that the improvement in Group A was significantly more than in Group B from the first follow-up onward (P < 0.001) till the third follow-up (P < 0.001). At the fourth follow-up visit, although percentage reduction was higher in Group A than in Group B, it was not statistically significant (P = 0.162). At the end of the study, 91.10 ± 9.65% surface area reduction had occurred in Group A, whereas it was 79.77 ± 17.91% in Group B, which means the effect continued for 4 weeks after active treatment with PRP was stopped; between-group comparison showed PRP to be significantly more efficacious (P < 0.001) [Table - 3] and [Figure - 7] and [Figure - 8].
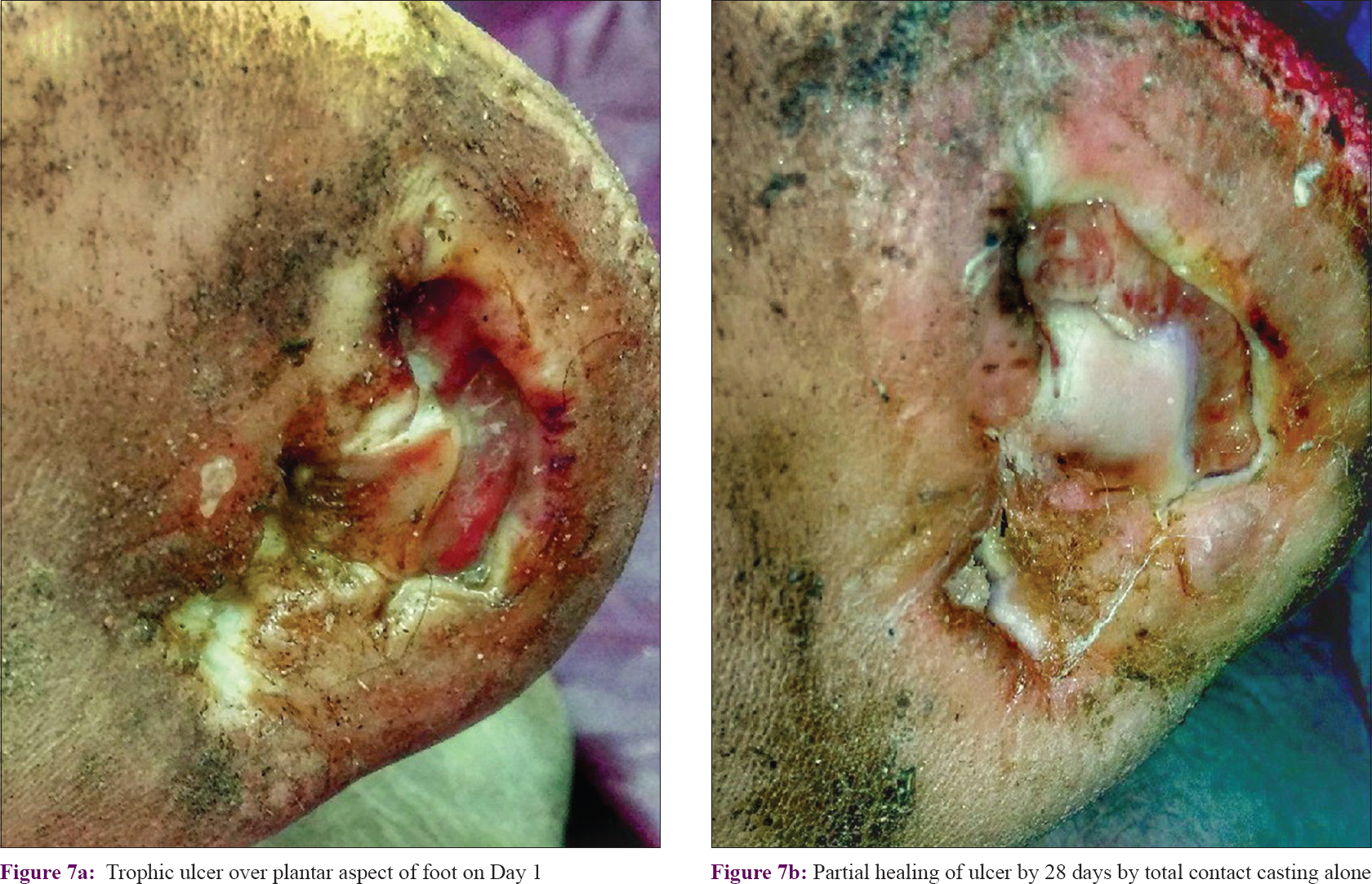 |
| Figure 7: |
 |
| Figure 8: |
Complete healing of the ulcer was obtained in 22 patients (39.29%) in Group A and 11 patients (21.15%) in Group B. Subgroup analysis of complete responders showed that age, sex and rural/urban status did not influence the outcome of the treatment. However, in complete responders, the duration of the ulcer was significantly shorter than in those with a partial response (P < 0.001). Also, the mean surface area was significantly lower (P < 0.001) in participants with complete healing (3.71 ± 3.81 cm2) than in those with partial healing of the lesion (6.67 ± 4.01 cm2). Trophic ulcers also healed completely in patients with paucibacillary leprosy significantly more (P < 0.001) than in patients with multibacillary leprosy. Therapy with PRP + total contact casting more often led to complete healing than total contact casting alone and the difference approached statistical significance (P = 0.059) [Table - 4].

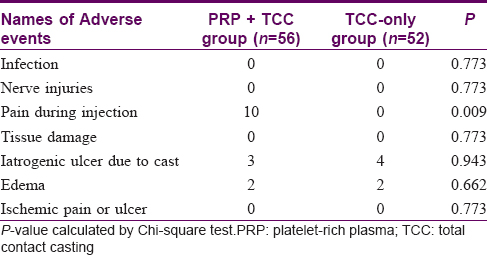
Adverse events were observed in 16 patients. Pain during injection was reported by 10 participants in the PRP + total contact casting group. No patient had any infection, tissue damage, nerve injury, or ischemic pain. There was no significant difference in occurrence of iatrogenic ulcers due to the cast or edema between the two groups. Laboratory parameters were within normal limits and comparable between the groups [Table - 5].
Discussion
Treatment of leprosy encompasses not only treatment of the disease but also minimisation of complications which could hinder the quality of life of the patient even after successful completion of multidrug therapy. One such complication is the neuropathic ulcer of leprosy which progresses relentlessly once the injury has occurred. Various modalities of treatment have failed to control its course. In our study, we have combined PRP with total contact casting and compared it with total contact casting alone in such ulcers. We found that there was a significant improvement of the size and surface area of the ulcer from 2 weeks onward in the combined therapy group with PRP. Complete healing of ulcers was found in twice as many participants in the PRP group as in the cast-only group. Though active treatment with PRP was only for 8 weeks, the improvement continued for another 4 weeks without treatment. It thus appears that PRP and platelet-poor plasma in association with offloading using total contact casting causes rapid improvement of the ulcers and the effect persists beyond the period of active treatment. The latter observation may be because growth factors released from platelets not only hastens the healing process but also have a residual effect after stoppage of therapy.
Faglia et al. in their study found that the mean ulcer surface area decreased from 1.41 to 0.21 cm2 by total contact casting only (P < 0.001).[16] In our study, we found that using total contact casting only the ulcer surface area reduced from 5.61 ± 3.70 to 1.21 ± 1.01 cm2, while on adding PRP it reduced from 5.91 ± 4.57 to 0.55 ± 0.68 cm2. This increased improvement with addition of PRP was found to be statistically significant (P < 0.001).
Frykberg et al.[17] found a 39.5% reduction in the mean surface area of trophic ulcers with PRP while Suryanarayan et al.[11] found 91.7% improvement. In our study, we have noted 91.1% reduction in the mean surface area which is comparable to Suryanarayan et al.'s[11] observation. However direct comparisons with these studies cannot be made as these studies included patients with leg ulcers from various etiologies, with only a few patients of leprosy trophic ulcers.
About 39.3% of the participants in the PRP group experienced complete resolution of lesions which was less than that obtained by Anandan et al.[14] (92% of 50 participants) or Rai et al.[18] (80% of 30 participants). This discrepancy may be due to different geographical and cultural strata of patients and occupational, socioeconomic differences among study populations and inclusion of non-leprosy cases.[18]
Pain at the injection site was found among 17.86% of patients in PRP + total contact casting group which subsided without any medication and did not produce any difficulty in the daily life of affected patients. Iatrogenic ulcers due to casting were found in only 6.5% among all patients which healed spontaneously within a few weeks after the removal of the final cast. Except for injection site pain, there was no significant difference in occurrence of adverse events among the two groups. There was no significant change in laboratory parameters indicating that the procedure of PRP and total contact casting is safe.
ASHA workers helped in ensuring the compliance with follow-up and the fact that ulcers started healing within 2 weeks also served as an additional factor for compliance. With regard to equipment, a centrifuge was already available in the department. Additional workforce was not required, except the orthopedician who was always available at the emergency ward. Extra cost was not incurred by the patient as PRP was separated from the patients' own blood and the cast was given free of cost at all government hospitals. With respect to feasibility, putting together a team of dermatologists and orthopedicians on a specific leprosy OPD day with a technician for separating PRP was done in the institute as an initiative of the disability management program running in the state under the Leprosy Division, Department of Health and Family Welfare, Govt. of West Bengal. It can hence be said that state-of-art care to leprosy ulcers can be provided with currently available facilities. With the World Health Organization's enhanced global strategy of disability prevention and management, the same model can be used in any district referral center. As an endeavor for disability management, the running program of National Leprosy Eradication Programme (NLEP) can use ASHA workers and the district nucleus team for arranging the referral system. The present project highlights a model which can be replicated and incorporated in the program.
A limitation of this study was the short duration of treatment restricted to 8 weeks due to logistic reasons. Increasing the number of sessions could have further increased the rate of complete cure. Further, we followed up patients only for a period of 4 weeks after treatment; longer follow-up might have given more information on the long-term effectiveness of the therapy.
Conclusion
PRP combined with total contact casting provides an effective and safe treatment modality of wound healing in trophic ulcers of leprosy. The improvement in reduction of the surface area of the ulcer is noted from 2 weeks from the commencement of therapy and holds promise in maintaining the efficacy even after discontinuation of treatment. The response is better if the duration and surface area of ulcer are less and the patient is in the paucibacillary spectrum, wherein it can lead to complete healing in 8 weeks.
What is known
Autologous PRP is effective in decreasing the healing times in diabetic ulcers, venous leg ulcers, stasis ulcers, claw foot, traumatic ulcers, trophic ulcers, and pressure ulcers. Total contact casting is an established method of offloading for the management of trophic ulcer in leprosy.
What is new
The present randomized controlled trial establishes the fact that autologous PRP can accelerate the process of healing in leprosy trophic ulcers when combined with total contact casting and is more effective in achieving faster relief than contact casting alone.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Acknowledgement
The study team acknowledges the untiring effort of the ASHA workers; District Leprosy team of Bankura, West Bengal; Dr. Swapan Kumar Sarkar, District Leprosy officer, Bankura; the Department of Orthopedics, Bankura Sammilani Medical College, Bankura. This study would not have been possible without the able guidance of Prof. Parthapratim Pradhan (Principal, Bankura Sammilani Medical College, Bankura); Prof. Arghyaprasun Ghosh (Head of the Department, Dermatology, Bankura Sammilani Medical College, Bankura); the faculty of the Department of Dermatology, Bankura Sammilani Medical College along with the residents, nurses, staff was an unerring support to the study.
Financial support and sponsorship
No formal sponsors were present in the study. The institution where the research was carried out, Bankura Sammilani Medical College, Bankura, West Bengal, India provided the patients and infrastructure required to carry out the study.
Conflicts of interest
The study was purely academic in nature The authors declare that there were no conflicts of interest.
| 1. |
Price EW. The problem of plantar ulcer. Lepr Rev 1964;35:267-72.
[Google Scholar]
|
| 2. |
Andersen JG. Plantar ulcers in leprosy. Their pathogenesis and natural history, and their therapy and prevention. Lepr Rev 1961;32:16-27.
[Google Scholar]
|
| 3. |
Srinivasan H. Trophic ulcers in leprosy III: Surgical management of chronic foot ulceration. Lepr India 1964;27:186-93.
[Google Scholar]
|
| 4. |
Barreto JG, Salgado CG. Clinic-epidemiological evaluation of ulcers in patients with leprosy sequelae and the effect of low level laser therapy on wound healing: A randomized clinical trial. BMC Infect Dis 2010;10:237.
[Google Scholar]
|
| 5. |
Puri V, Venkateshwaran N, Khare N. Trophic ulcers-practical management guidelines. Indian J Plast Surg 2012;45:340-51.
[Google Scholar]
|
| 6. |
Pitiakoudis M, Giatromanolaki A, Iliopoulos I, Tsaroucha AK, Simopoulos C, Piperidou C, et al. Phenytoin-induced lymphocytic chemotaxis, angiogenesis and accelerated healing of decubitus ulcer in a patient with stroke. J Int Med Res 2004;32:201-5.
[Google Scholar]
|
| 7. |
Mishra S, Singh PC, Mishra M. Metronidazole in management of trophic ulcers in leprosy. Indian J Dermatol Venereol Leprol 1995;61:19-20.
[Google Scholar]
|
| 8. |
Wieman TJ, Smiell JM, Su Y. Efficacy and safety of a topical gel formulation of recombinant human platelet-derived growth factor-BB (becaplermin) in patients with chronic neuropathic diabetic ulcers. A phase III randomized placebo-controlled double-blind study. Diabetes Care 1998;21:822-7.
[Google Scholar]
|
| 9. |
Birang R, Torabi A, Shahabooei M, Rismanchian M. Effect of plasma-rich in platelet-derived growth factors on peri-implant bone healing: An experimental study in canines. Dent Res J (Isfahan) 2012;9:93-9.
[Google Scholar]
|
| 10. |
Arshdeep, Kumaran MS. Platelet-rich plasma in dermatology: Boon or a bane? Indian J Dermatol Venereol Leprol 2014;80:5-14.
[Google Scholar]
|
| 11. |
Suryanarayan S, Budamakuntla L, Khadri SI, Sarvajnamurthy S. Efficacy of autologous platelet-rich plasma in the treatment of chronic nonhealing leg ulcers. Plast Aesthet Res 2014;1:65-9.
[Google Scholar]
|
| 12. |
Conde-Montero E, Horcajada-Reales C, Clavo P, Delgado-Sillero I, Suárez-Fernández R. Neuropathic ulcers in leprosy treated with intralesional platelet-rich plasma. Int Wound J 2016;13:726-8.
[Google Scholar]
|
| 13. |
American Association of Blood Banks Technical Manual Committee. Method 6.11: Preparation of platelets from whole blood. In: Vengelen-Tyler V, editor. AABB Technical Manual. 13th ed. Bethesda (MD): American Association of Blood Banks; 1999. p. 725.
[Google Scholar]
|
| 14. |
Anandan V, Jameela WA, Saraswathy P, Sarankumar S. Platelet rich plasma: Efficacy in treating trophic ulcers in leprosy. J Clin Diagn Res 2016;10:WC06-9.
[Google Scholar]
|
| 15. |
Sundaresan AN, Vikram M, Mohandas K, Nur Farhana MY, Potturi Gowri S, Mahendran J. Impact of total contact plaster boot via offloading practice in trophic ulcers of the feet: Case series. Med and Health 2014;9:80-84. Availbale from: https://pdfs.semanticscholar.org/3edd/2d4b4cd06378e9d0f5152e306d024506e814.pdf. [Last accessed on 2019 Sep 25].
[Google Scholar]
|
| 16. |
Faglia E, Caravaggi C, Clerici G, Sganzaroli A, Curci V, Vailati W, et al. Effectiveness of removable walker cast versus nonremovable fiberglass off-bearing cast in the healing of diabetic plantar foot ulcer: A randomized controlled trial. Diabetes Care 2010;33:1419-23.
[Google Scholar]
|
| 17. |
Frykberg RG, Driver VR, Carman D, Lucero B, Borris-Hale C, Fylling CP, et al. Chronic wounds treated with a physiologically relevant concentration of platelet-rich plasma gel: A prospective case series. Ostomy Wound Manage 2010;56:36-44.
[Google Scholar]
|
| 18. |
Rai S, Gupta AK, Kumar D, Aggarwal AK, Sharma VP. Total contact casting in the treatment of nonhealing plantar ulcers in anesthetic foot. Indian J Dermatol Venereol Leprol 2016;82:422-3.
[Google Scholar]
|
Fulltext Views
8,061
PDF downloads
3,813





