Translate this page into:
Efficacy and safety of intense pulsed light in rosacea: A systematic review
Corresponding author: Dr. Cintia Cristina Santi Martignago, Department of Biosciences, Federal University of São Paulo - Unifesp, Silva Jardim, Santos, Brazil. csantimartignago@yahoo.com.br
-
Received: ,
Accepted: ,
How to cite this article: Martignago CCS, Bonifacio M, Ascimann LT, Vassão PG, Parisi JR, Renno AP et al. Efficacy and safety of intense pulsed light in rosacea: A systematic review. Indian J Dermatol Venereol Leprol. 2024;90:599-605. doi: 10.25259/IJDVL_1029_2022
Abstract
Background
Rosacea is a chronic inflammatory disease of the skin characterised by facial erythema, oedema, telangiectasias, papules, pustules and nodules. There is a paucity of effective therapeutic modalities for the management of rosacea. Intense Pulsed Light (IPL), a modality in which flash lamps installed in an optical treatment device (head or tip) with mirrors to reflect light, has in recent times gained popularity in the management of this condition.
Aim
This systematic review aims to evaluate the efficacy, safety and adverse effects of IPL treatment for rosacea.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Item for Systematic Reviews and Meta-Analysis. The electronic databases searched were Medline, PubMed and Scopus databases. The Risk of bias in non-randomised studies of interventions (ROBINS-I) and risk-of-bias tools for randomised trials (RoB-2) was employed to assess the risk of bias.
Results
Of a total of 233 articles retrieved from Medline, Scopus and PubMed databases, 14 studies qualified for final analysis. The studies included patients with Fitzpatrick skin types I to IV, with ages ranging from 15 to 78 years. Although the included studies showed heterogeneity between the parameters used, most studies demonstrated positive effects of IPL treatment on telangiectasia and erythema in rosacea and that the adverse effects presented were transitory.
Limitation
The methodological quality of the included studies was poor.
Conclusion
Although most studies showed the efficacy of IPL in the treatment of rosacea, the poor quality of the studies was of concern.
Keywords
Intense pulsed light therapy
rosacea
systematic review
skin
Introduction
Rosacea is a chronic inflammatory cutaneous disorder affecting the face, especially the cheeks, chin, nose and forehead.1,2 Cutaneous signs of rosacea include flushing, erythema, telangiectasia, oedema, papules, pustules and rhinophyma.3 More than 50% of patients with rosacea also experience ocular symptoms such as dryness, irritation, blepharitis, conjunctivitis, and compromised vision.4 It is more common in women and its prevalence varies across populations, ranging from less than 1% to 22%.5
The pathophysiological mechanisms of rosacea are unclear, but they involve genetic factors, vascular and neural abnormalities, dermal matrix degeneration, microorganisms and environmental factors, such as heat, nutrition and ultraviolet light.2,6 The inflammatory process in the skin may be worsened by pro-inflammatory substances and degradative enzymes released by inflammatory cells, leading to dermal destruction.7
The primary focus of rosacea treatment is to alleviate symptoms and improve facial appearance. Educating patients about their skin condition and potential exacerbating factors is an important aspect of management. This helps them identify and avoid triggers that can worsen their condition.3,8 Beta-blockers, α2-adrenergic agonists and brimonidine tartrate are frequently used pharmacological interventions.3,7,9
Various light-based therapies such as low laser therapy and intense pulsed light (IPL) have been used for treating the erythema and telangiectasia of rosacea.8,3 IPL uses non-collimated, non-coherent light of different wavelengths to target specific chromophores making it a versatile therapy for hair removal, skin rejuvenation and the treatment of pigmented or vascular lesions.10 The 577 nm wavelength of IPL corresponding to the third absorption peak of oxyhaemoglobin is absorbed by haemoglobin inducing photothermolysis. This selectively destroys blood vessels and causes thermal damage to the papillary and upper reticular dermis.11,12 IPL destroys abnormal vessels in patients with rosacea and improves the dermal connective tissue disorganisation of the vascular component of rosacea (erythema and telangiectasia).13,14
While the positive effects of IPL in treating rosacea are well-documented, its use is still controversial, particularly with regard to the parameters required to achieve optimal results. Despite advances in research on the use of light for managing rosacea, no systematic review of the exclusive use of IPL in rosacea has been conducted. The present study aimed to analyse literature on the effects and safety of IPL for treating rosacea-related symptoms in clinical studies.
Materials and Methods
This systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines15 at the Federal University of the State of São Paulo, Brazil in October 2022. It was registered on the online International Prospective Register of Systematic Reviews (PROSPERO) of the National Institute for Health Research (Registration ID: CRD42021285751).
We used the Medline, PubMed and Scopus electronic databases to systematically search for articles on IPL and rosacea in clinical trial studies. The Medical Subject Headings (MeSH) terms and Boolean operator in the electronic search strategy were “intense pulsed light” and “rosacea”. Articles were selected based on their titles and abstracts meeting the eligibility criteria. The methodological quality of all included studies was assessed using the Cochrane Risk of Bias (RoB 2.0)16 scale for randomised clinical trials and Risk of Bias in Non-randomised Studies of Interventions (ROBINS-I).17
Inclusion criteria
We included only complete trials conducted in patients with rosacea and published in English. No publication date or publication status restrictions were imposed. The presence or absence of a control group (a group without treatment, a placebo IPL or a group with a different treatment modality) did not influence selection. Digital photographs in the articles were also evaluated.
Exclusion criteria
We excluded in vivo and in vitro studies, systematic reviews and meta-analyses, case reports and experimental studies, studies that used other interventions besides IPL, follow-ups of previously published trials and conference abstracts.
Outcomes Assessment
Data was extracted from the studies by two reviewers (ACMR and CCSM), who independently analysed the title and abstract. The selection was based on the inclusion and exclusion criteria and all differences were solved through discussion.
The study database included:
-
Basic characteristics of qualified studies
-
Characteristics of the subjects (number of participants, age, gender, etc.)
-
Interventions (treated group, control group, or other treatment group and analyses)
-
Details of the IPL used (spot size, mode, wavelength (λ), pulse rate, energy density and application area)
-
Outcome measures that included the level of symptom improvement evaluated before and after treatment
Adverse effects were also assessed.
Results
The flow diagram shown in Figure 1 illustrates the search strategy used in the study. A total of 233 articles were retrieved from the Scopus and PubMed databases (147 and 86 articles, respectively). After excluding 64 duplicated records, 134 articles were excluded after reading the title and 8 after reading the abstract. The remaining 27 full-text articles were assessed for eligibility and finally 14 studies were selected for the systematic review. The classification of rosacea was not a criterion for the inclusion/exclusion of studies.
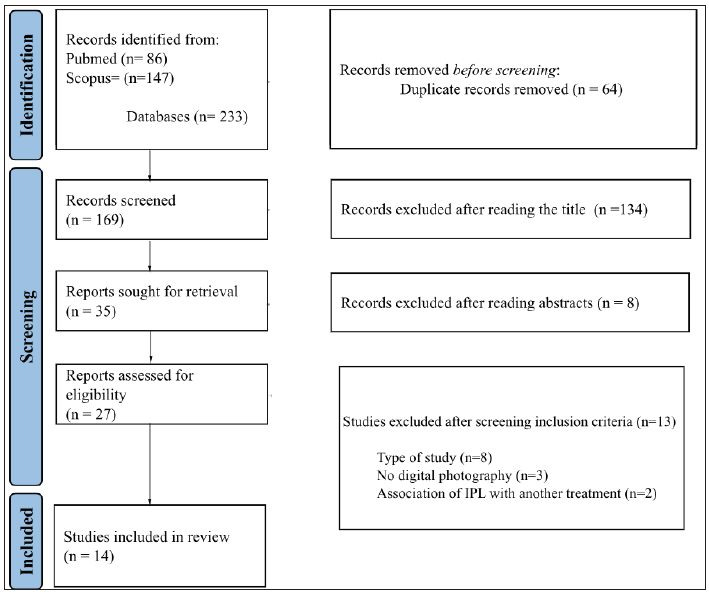
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of the studies included in the systematic review.
The general characteristics of patients and experimental groups from these 14 articles are summarised in Table 1. The studies included patients with Fitzpatrick skin types I to IV, with ages ranging from 15 to 78 years. Three studies recruited only females.18,19,20 While 11 studies recruted both male and female patients.12,13,21–29
| Authors | Number of participants/Gender | Age (years) | Skin type | Intervention group | Control or other treatment group | Study design |
|---|---|---|---|---|---|---|
| Mark et al.18 | 4 (female) | 43 to 55 | * | 5 sessions every 3 weeks with the IPL | & | Case series |
| Schroeter et al.23 | 60 (55 female and 5 male) | Mean age of 44.2 | Fitzpatrick I–IV | 1 session of IPL (reevaluation after 1, 2, 4 and 12 weeks) | & | Case series |
| Kawana et al.19 | 6 (female) | 37 to 66 | Fitzpatrick skin type III | 3 sessions of IPL (interval of 4 weeks) | & | Case series |
| Papageorgiou et al.24 | 34 (25 female and 9 male) | Mean age of 47 (18–65) | Fitzpatrick skin type I–IV | 4 sessions of IPL (interval of 3 weeks) | & | Case series |
| Neuhaus et al.29 | 30 (20 female and 9 male) | Mean age of 45.8 | Fitzpatrick skin types I–III | 3 sessions of IPL (interval of 4 weeks) | 4 patients received Pulsed Dye Laser to one side of the face and no treatment to the other side (control) | Clinical Trial |
| Campolmi et al.25 | 85 (64 female and 21 male) | 28 to 75 | Fitzpatrick skin types I–IV | 5 sessions of IPL (range 4–6) at 3-weekly intervals | & | Case series |
| Kassir et al.26 | 102 (94 female and 8 male) | 15 to 69 | Fitzpatrick skin types I–IV | 7 sessions (interval of 1-3 weeks) | & | Case series |
| Liu et al.13 | 32 (6 female and 8 male) | 18–47 (median, 35.8) | Fitzpatrick skin phototype III–V | 3 sessions (3-week intervals) | & | Case series |
| Lim et al.27 | 50 (male and female) | 50.17 | * | 4 sessions (interval of 3 weeks) | & | Case series |
| Marques et al.28 | 9 (female and male) | 36 to 59 | Fitzpatrick skin types I to III | 3 sessions (interval of 30 days) | & | Case series |
| Kim et al.21 | 9 (female and male) | 20 to 59 | Fitzpatrick skin types II–IV | 4 sessions with an interval of 4 weeks(evaluation period baseline and at weeks 3, 6, 9, 12, and 15) | Pulsed dye laser | Clinical Trial |
| Tsunoda et al.20 | 13 (female) | 36 to 78 | * | 4 sessions of IPL with an interval of 4-16 weeks | & | Case series |
| Luo et al.22 | 260 (female and male) | 18 to 60 | Fitzpatrick skin types III to IV | 3 sessions of IPL with an interval of 4 weeks | Control group with no treatment | Clinical Trial |
| Tirico et al.12 | 5 (4 female and 1 male) | 48 to 61 | Fitzpatrick skin types I to III | 2 sessions of IPL (patient’s face was divided into left and right sides) | Pulsed dye laser | Clinical Trial |
IPL: Intensed Pulsed Light; * data not described in the study; &: Only one treatment group
All studies used IPL alone as an intervention group. Ten studies did include any control groups.13,18–20,23–28 three studies12,20,28 used a group of pulsed dye laser (PDL) treated patients and 1 study used untreated patients as controls.29 In the study conducted by Neuhaus et al.,29 patients were treated with IPL on one side of the face and PDL on the other.29
The IPL protocols used in the studies are detailed in Table 2. Spot sizes were mentioned in 7 studies and varied from 1 × 4 mm to 15 × 40 mm.19,20,22–24,26,28 The pulse duration was specified in all studies and varied from 1.5 to 25 ms and the wavelengths used ranged from 420 to 1200 nm. In 4 studies, 2 separate handpieces emitting different wavelengths were used [Table 2].20,23,27 The energy density applied also varied widely from 15 J/cm2 to 90 J/cm2.
| Authors | Spot size | Pulse duration | Wavelength (nm) | Energy density |
|---|---|---|---|---|
| Mark et al.18 | * | a single pulse duration of 3 ms | 515 | 22 and 25 J/cm2 |
| Schroeter et al.23 | 8 × 35 mm2 | 4.3 and 6.5 ms | 515 to 1.200 | 15 and 90 J/cm2 |
| Kawana et al.19 | 10 × 15mm2 | 20 ms | 550–670 | 21 J/cm2 |
| Papageorgiou et al.24 | 34 × 8 mm2 | 15 ms | 560 | 24–32 J/cm2 |
| Neuhaus et al.29 | * | 6 ms | 560 | 25 J/cm2 (increase of 1 J/cm2 at each subsequent session) |
| Campolmi et al.25 | * | Double pulse of 3 to 8 ms | 500 to 550 | 9 to 13 J/cm2 |
| Kassir et al.26 | 10 × 40 mm2 | 2.5 to 5 ms | 420–530 | 25 J/cm2 for skin type 1, 21 J/ cm2 for skin type 2, 17 J/cm2 for skin type 3, 13 J/cm2 for skin type 4, 10 J/cm2 for skin type 5. |
| Liu et al.13 | 6.4cm2 | 12 msec | 540 | 10–12 J/cm |
| Lim et al.27 | * | 6-7 ms | 560 | 12∼16 J/cm2 |
| Marques et al.28 | * | 12 and 25 ms | 535–680 and 860–1,200 | 10 to 20 J/cm2 |
| Kim et al.21 | 7 mm | 1.5 ms | 555 | 8 J/cm2 |
| Tsunoda et al.20 | Two devices: 4 × 1 mm2 and 6.35-mm mm2 | * | 590–1200 wavelength and 500–635 | 22–24 J/cm2 and 14–15 J/cm2 |
| Luo et al.22 | 1.5 × 4 cm2 | 12 ms | 540 | 10–16 J/cm2 |
| Tirico et al.12 | 10 × 48 mm | 1.5 ms | 595 | 4 J/cm2 (with an increase of 0.5 J/cm2 per section) |
* data not available in the article
Various evaluation methods were employed to assess the effects of IPL [Table 3]. All studies used digital photography to assess the area of telangiectasia, erythema, and the number of lesions.12,18,20–23,25,26,28,29 Blood flow analysis was used in one study,18 while two studies used spectrophotometer analysis.19,29 Questionnaires and scales employed in these studies included various visual analogue scales (4, 5, 6, and 10 point VAS) and patient global assessment (PGA).
| Authors | Evaluations | Results | Outcomes | Adverse effects |
|---|---|---|---|---|
| Mark et al.18 | Blood flow and digital photographs (telangiectasia area and erythema colour). |
- 30% decrease in blood flow; - There was a decrease of 29% in the area of telangiectasia and a 21% decrease in the intensity of erythema. |
+ | * |
| Schroeter et al.23 | Digital photographs analysing facial clearance of telangiectasia and lesions on the forehead. | 77.8% clearance of facial telangiectasia. 87% demonstrated clearance of the lesions on the forehead. | + | Erythema and purpure. Some patients complained of pain and oedema. |
| Kawana et al.19 | Measurement of skin colour by spectrophotometer; Self-efficacy evaluation. | Improved values for spectrophotometer analysis and improved index of self-satisfaction. | + | Mild erythema in the same patients but disappeared several days later—some complaints of weak pain. |
| Papageorgiou et al.24 | Colour digital photographs of the face; 10-point VAS (severity of erythema and severity of telangiectasia). Patients and doctor’s assessments of rosacea using a six-point VAS. | The erythema reduction was 39% on the cheeks and 22% on the chin. Erythema improved by 46% and telangiectasia by 55%—reducing the severity of rosacea. The patient self-reported improvement of rosacea and reported a reduction of their flushing. | + | Side effects were minimal (bruising). |
| Neuhaus et al.29 | Full-face digital photographs; Spectrophotometer of overall erythema grade and telangiectasia grade on a 4-point scale; quantitative telangiectasia counts of the face. |
- No improvements in erythema in the malar region but an improvement in the cheek region. - Reductions in erythema Score. - Lower erythema and telangiectasia grade. - The reduced value of telangiectasia counts. |
+ | * |
| Campolmi et al.25 | Photographs of the lesions; Clinical observations; Patient’s subjective evaluation; Anthology-system photographs. |
- All patients observed global improvements in their lesions; - 72 (80.9%) lesions achieved a marked improvement, 14 (15.7%) lesions a moderate improvement and 3.4%, a slight improvement. - 69 (81.2%) patients were very satisfied, 14 (16.5%) patients were satisfied and 2 (2.3%) patients were not satisfied. |
+ |
Erythema, edema, swelling, mild purpura and pain. |
| Kassir et al.26 | Digital photograph to measure redness, flushing, acne and telangiectasia. | 80% of patients had reduced redness, 78% noted reduced flushing and improved skin texture, and 72% reported fewer acneiform breakouts. Photo Documentation showed a 51% reduction in telangiectasias. | + | * |
| Liu et al.13 | Digital photographs Severity of erythema; Patient’s satisfaction (10-point visual scale) | All patients showed clinical improvements and higher satisfaction after the treatment. | + | No noticeable side effects, except for transient erythema/oedema with resolution within a few days. |
| Lim et al.27 | Rosacea severity; Physician’s global assessment and patient’s global assessment (4-point scale). | Significant differences in severity scores between pre-treatment and post-treatment were significantly observed. | + | Four patients complained of erythema, six pain during treatment, and one hyperpigmentation. |
| Marques et al.28 | Digital photographs; Questionnaire to assess the treatment’s efficacy using a scale; flushing, persistent erythema and telangiectasia. | Improvements in erythema and telangiectasia Significant improvement in skin texture and flushing; 50% were classified as having had more than 75% improvement in the overall clinical picture. | + | Burning sensation was reported by 50% of patients. |
| Kim et al.21 | Photographic for evaluating erythema and melanin indices; Changes in investigator’s Global Assessment (IGA); Subjective patient global assessment. |
- Improvement of erythema and melanin indices; - Clinical improvement in erythema, telangiectasia and papules and pustules; - Improved values of IGA; - Clinical improvement of > 50% clearance; - 77.8% of patients reported being very satisfied or satisfied. |
+ | Transient erythema and oedema (symptoms resolved within a few hours without special management). |
| Tsunoda et al.20 | Photographic assessments of facial telangiectasia used for quantitative evaluation; Clinical photographic a 4-point scale. | Improvement of the clearance of telangiectasia on the face. | + | * |
| Luo et al.22 | Photographs allow the measurement of the severity of telangiectasia. |
- 1 month after the initial IPL treatment, 19 (17.8%) patients with facial telangiectasia were characterised as improved. At 3 months, the total efficacy rate had increased to 39.2%; - 4 months, 72 (67.3%) patients showed some degree of improvement, while 35 (32.7%) patients showed effective treatment. - 6 months, 102 (95.3%) patients showed improvement, whereas 71 (66.4%) patients were effective. |
+ | Mild burning sensation, temporary skin flushing and local skin oedema faded spontaneously. |
| Tirico et al.12 | Digital photographs. | Redness was reduced by an average of 60% on the IPL side and 45% on the PDL side. | * | Modest pain. |
IPL: Intense Pulsed Light; PDL: Pulsed dye Laser; VAS: Visual Analogue Scale; *data not available in the article; +positive results for the outcomes evaluated
The positive effects of IPL persisted after treatment in all the studies. The area of telangiectasia and erythema as well as the number of lesions were significantly reduced after treatment.18,20–26,28,29 Kassir et al.26 observed that 80% of patients had reduced redness, 78% noted reduced flushing and improved skin texture, 72% reported fewer acneiform breakouts, and 51% demonstrated a reduction in telangiectasias. Tirico et al.12 noted decreased redness after IPL treatment, Marques et al.28 observed improvement in flushing and skin texture and Kim et al.21 observed clinical improvement in erythema, telangiectasia, papules, and pustules. Improvement after IPL treatment was demonstrated by spectrophotometer analysis in two studies.19,29
Improvement in signs and symptoms after IPL treatment were confirmed through the use of scales and questionnaires. In the study of Campolmi et al.25 Neuhaus et al.29 noted an improvement in patient-rated signs and symptoms.
Adverse effects were transitory and included pain, oedema, minimal bruising, and burning sensations.
The risk of bias assessment for both the randomised and non-randomised trials is illustrated in Figures 2a and 2b. The RoB-2 assessment [Figure 2a] revealed an unclear risk of bias in all studies due to missing outcome data. This arose from the randomisation process in 3 studies and in the measurement of the outcome in one study. A high risk of bias was noted in one study due to deviations from intended interventions29 and in 2 studies in the bias domain in selecting the reported result.12,21 A low risk of bias arising from the randomisation process was noted in a single study,29 in 2 in the selection of the reported result,22,29 and in 3 studies each due to the deviations from intended interventions12,21,22 or in the measurement of the outcome.21,22,29
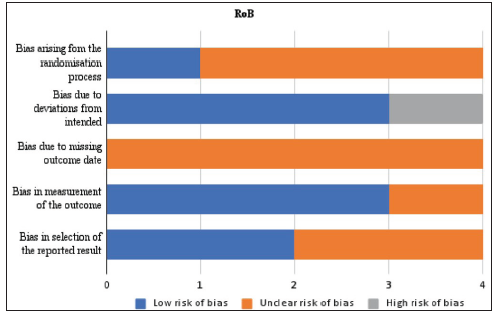
- Risk of bias assessment for the randomised clinical trials (RoB-2).
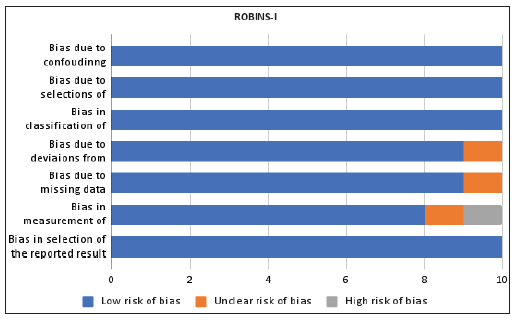
- Risk of bias assessment for the non-randomised intervention studies (ROBINS-I).
In the ROBINS-I assessment [Figure 2b], one study had a high risk of bias in the field of measurement of outcomes.26 Additionally, an unclear risk of bias was found in the domains of deviations from intended interventions,26 missing data,24 and measurement of outcomes.23 All studies had a low risk of bias classification in the domains of confounding, selection of participants, type of interventions, and selection of the reported result.
Discussion
IPL is an effective non-invasive therapeutic intervention for the treatment of port wine stains, haemangiomas, and facial telangiectasia.30,31,32 It has also been demonstrated to reduce erythema, papules and pustules and improve skin texture in patients with rosacea.33,34 Multiple sessions (up to 15) at 1-to-3-week intervals may be necessary, and parameters need to be adjusted individually according to the phototype, severity and tolerance to minimise side effects.26
Our systematic review found that IPL was effective in managing the symptoms of rosacea in both males and females of Fitzpatrick skin types I to IV aged between 15 and 78 years. However, due to the wide range of IPL parameters used in these studies (wavelengths varying from 420 nm26 to 1200 nm,23 energy density from 15 J/cm2 to 90 J/cm2,23 and number of sessions from 1 to 7)23,26, and the different methods used to evaluate the effects of IPL (digital photos, patient self-reported perception, scales, and questionnaires), the end results are not strictly comparable.
The optimal use of IPL parameters such as fluence, pulse duration, wavelengths, treatment time, and spot size in clinical settings is crucial for achieving the best tissue responses and minimising the risk of tissue damage.31,35 Shorter wavelengths (400 to 585 nm) and shorter pulse durations (450 ms) are thought to have a better effect on skin owing to the limited depth of penetration (up to 1.5 mm).33
Papagerogiu et al, using a 560 nm a wavelength observed an average reduction of 3.5 points in the severity of rosacea pain measured with the 10-point VAS.24 In this same study, over 50% improvement was seen in 73% and 83% of patients as per the evaluation of the patients and physicians respectively. The results were sustained for 6 months. Other authors used higher wavelengths (e.g., 1200 nm) and also noted good results.30 These effects may be due to the absorption of wavelengths in the 900 to 1200 nm spectrum by water in the dermis triggering a cytokine reaction that stimulates the formation of elastin and collagens I and III.
A wide range of energy densities (from 15 J/cm2 to 90 J/cm2) were used in the studies. High energy densities can cause burns, while lower fluences may not be effective.36 The spot size (area covered by the beam at the tip of the applicator) varied significantly among different machines, ranging from 4 to 64 mm2.20,28,37 The number of treatment sessions and the period of treatment were not uniform across the studies and between 1 and 7 treatment sessions at intervals of 3 to 4 weeks were used. Although standard IPL protocols suggest a 3–4 week interval between treatments, Papageorgiou et al. have proposed that a longer interval of 6 or 8 weeks may be more cost-effective.24
Most studies have reported an improvement in erythema and telangiectasia after IPL application.30,38–44 This may be due to the ablation of abnormally dilated vessels and the reduction of extravascular leakage of inflammatory mediators.13 IPL also stimulates new collagen deposition and collagen remodelling, which improves support for small blood vessels, dermal connective tissue disorganisation, and elastosis.23,24 The improvement in the vascular features of rosacea (erythema and telangiectasia) could subsequently lead to a decrease in inflammatory lesions.23,24,32
Limitations
Eight of the studies were of low methodological quality.18,19,23–28 Neither the investigators nor the subjects were blinded, and the treatments were not concealed.
Conclusion
IPL is a safe and effective treatment for rosacea. However, since all trials included in the studies show methodological limitations, more trials of better methodological quality must be conducted.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
This work is supported by the São Paulo Research Foundation (Grant Number 2021/02974-9 Recipient: Cintia Cristina Santi Martignago).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pathophysiology of rosacea: redness, telangiectasia, and rosacea. Annales de Dermatologie et de Vénéréologie. 2011;138:S184-91.
- [CrossRef] [PubMed] [Google Scholar]
- Rosacea treatment update: Recommendations from the global rosacea consensus (ROSCO) panel. Br J Dermatol. 2017;176:465-71.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema of rosacea impairs health-related quality of life: Results of a meta-analysis. Dermatol Ther. 2016;6:237-47.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Rosacea: Current state of epidemiology. J Am Acad Dermatol. 2013;69:S27-35.
- [CrossRef] [PubMed] [Google Scholar]
- Rosacea: Part I. introduction, categorization, histology, pathogenesis, and risk factors. J Am Acad Dermatol. 2015;72:749-60.
- [CrossRef] [PubMed] [Google Scholar]
- Rosacea: Part II. Topical and systemic therapies in the treatment of rosacea. J Am Acad Dermatol. 2015;72:761-72.
- [CrossRef] [PubMed] [Google Scholar]
- Rosacea - global diversity and optimized outcome: Proposed international consensus from the rosacea international expert group. J Eur Acad Dermatol Venereol. 2011;25:188-200.
- [CrossRef] [PubMed] [Google Scholar]
- Acne and rosacea. Dermatol Ther (Heidelb). 2017;7:43-52.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparative evaluation in intense pulsed light therapy combined with or without meibomian gland expression for the treatment of meibomian gland dysfunction. Curr Eye Res. 2021;46:1125-1131.
- [CrossRef] [PubMed] [Google Scholar]
- Intense pulsed light for evaporative dry eye disease. Clin Ophthalmol (Auckland, N.Z.). 2017;11:1167-1173.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Short pulse intense pulsed light versus pulsed dye laser for the treatment of facial redness. J Cosmet Laser Ther 2020:1-5. doi:10.1080/14764172.2020.1717540
- [CrossRef] [PubMed] [Google Scholar]
- Comparative efficacy of intense pulsed light for different erythema associated with rosacea. J Cosmet Laser Ther. 2014;16:324-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic monitoring of response to intense pulsed light in rosacea: A case report. Dermatol Pract Concept. 2020;10:e2020058.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
- [CrossRef] [PubMed] [Google Scholar]
- ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. . 2016;355:i4919.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Objective and quantitative improvement of rosacea-associated erythema after intense pulsed light treatment. Dermatol Surg. 2003;29:600-4.
- [CrossRef] [PubMed] [Google Scholar]
- Objective evaluation of the effect of intense pulsed light on rosacea and solar lentigines by spectrophotometric analysis of skin color. Dermatol Surg. 2007;33:449-454.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of erythematotelangiectatic rosacea with intense pulsed light: Report of 13 cases. J Dermatol. 2018;45:1113-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative efficacy of short-pulsed intense pulsed light and pulsed dye laser to treat rosacea. J Cosmet Laser Ther. 2019;21:291-296.
- [CrossRef] [PubMed] [Google Scholar]
- Improved telangiectasia and reduced recurrence rate of rosacea after treatment with 540 nm-wavelength intense pulsed light: A prospective randomized controlled trial with a 2-year follow-up. Exp Ther Med. 2020;19:3543-3550.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effective treatment of rosacea using intense pulsed light systems. Dermatol Surg. 2005;31:1285-1289.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of rosacea with intense pulsed light: Significant improvement and long-lasting results. Br J Dermatol. 2008;159:628-32.
- [CrossRef] [PubMed] [Google Scholar]
- Intense pulsed light in the treatment of non-aesthetic facial and neck vascular lesions: report of 85 cases. J Eur Acad Dermatol Venereol. 2011;25:68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Intense pulsed light for the treatment of rosacea and telangiectasias. J Cosmet Laser Ther. 2011;13:216-22.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of intense pulsed light for treating erythematotelangiectatic rosacea is related to severity and age. Ann Dermatol. 2014;26:491-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Treatment of rosacea with dual-band wavelength intense pulsed light in a single shot. Surg Cosmet Dermatol. 2016;8:128-32.
- [Google Scholar]
- Comparative efficacy of nonpurpuragenic pulsed dye laser and intense pulsed light for erythematotelangiectatic rosacea. Dermatol Surg. 2009;35:920-28.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of a novel Flash Lamp System (FLS) incorporating optimal spectral filtration for the treatment of photoaging. Lasers Surg Med. 2005;37:108-13.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of intense pulsed light and laser treatment of telangiectases in patients with systemic sclerosis: A within-subject randomized trial. Rheumatol (Oxford). 2014;53:1422-30.
- [CrossRef] [PubMed] [Google Scholar]
- Single-session combination treatment with intense pulsed light and nonablative fractional photothermolysis: A split-face study. Dermatologic surgery: Official publication for American Society for Dermatol Surg. 2012;38:1002-9.
- [CrossRef] [PubMed] [Google Scholar]
- Current trends in intense pulsed light. J Clin Aesthet Dermatol. 2012;5:45-53.
- [PubMed] [PubMed Central] [Google Scholar]
- Intense pulsed light therapy for skin rejuvenation. Clin Plast Surg. 2016;43:535-40.
- [CrossRef] [PubMed] [Google Scholar]
- Nonablative treatment of rhytids with intense pulsed light. Lasers Surg Med. 2000;26:196-200.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring key parameters of intense pulsed light (IPL) devices. J Cosmet Laser Ther. 2007;9:148-60.
- [CrossRef] [PubMed] [Google Scholar]
- Intricacies of dose in laser phototherapy for tissue repair and pain relief. Photomed Laser Surg. 2009;27:387-93.
- [CrossRef] [PubMed] [Google Scholar]
- Photorejuvenation by intense pulsed light with objective measurement of skin color in Japanese patients. Dermatologic Surg. 2006;32:1380-87.
- [CrossRef] [PubMed] [Google Scholar]
- Split-face treatment of facial dyschromia: Pulsed dye laser with a compression handpiece versus intense pulsed light. Dermatologic Surg. 2008;34:672-80.
- [CrossRef] [PubMed] [Google Scholar]
- Ablative versus non-ablative treatment of perioral rhytides. A randomized controlled trial with long-term blinded clinical evaluations and non-invasive measurements. Lasers Surg Med. 2006a;38:129-36.
- [CrossRef] [PubMed] [Google Scholar]
- Intense pulsed light treatment of photoaged facial skin. Dermatologic Surg. 2004;30:1085-1090.
- [CrossRef] [PubMed] [Google Scholar]
- A split-face study of intense pulsed light on photoaging skin in Chinese population. Lasers Surg Med. 2010;42:185-91.
- [CrossRef] [PubMed] [Google Scholar]
- Hand rejuvenation using standard intense pulsed light (IPL) in Asian patients. Laser Ther. 2016;25:43-54.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Intense pulsed light and red light photo rejuvenation for skin rejuvenation: A split face clinical trial. J Lasers Med Sci. 2011;29:63-6.
- [Google Scholar]







