Translate this page into:
Efficacy of fixed duration multidrug therapy for the treatment of multibacillary leprosy: A prospective observational study from Northern India
Corresponding author: Dr. Mallika Lavania, ICMR-National Institute of Virology, Pune, Maharashtra, India. mallikalavania@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singh I, Ahuja M, Lavania M, Pathak VK, Turankar RP, Singh V, et al. Efficacy of fixed duration multidrug therapy for the treatment of multibacillary leprosy: A prospective observational study from Northern India. Indian J Dermatol Venereol Leprol 2023;89:226-32.
Abstract
Background:
In endemic regions of several countries, the prevalence of leprosy has not come down to the level of elimination. On the contrary, new cases are being detected in large numbers. Clinically, it is frequently noted that despite completion of multibacillary multidrug therapy for 12 months, the lesions remain active, especially in cases with high bacteriological indices.
Aim:
The present study focused on finding out the viable number of Mycobacterium leprae during the 12-month regimen of multibacillary multidrug therapy, at six and 12 months intervals and, attempting to determine their role in disease transmission.
Methods:
Seventy eight cases of multibacillary leprosy cases were recruited from leprosy patients registered at The Leprosy Mission hospitals at Shahdara (Delhi), Naini (Uttar Pradesh) and Champa (Chhattisgarh), respectively. Slit skin smears were collected from these patients which were transported to the laboratory for further processing. Ribonucleic acid was extracted by TRIzol method. Total Ribonucleic acid was used for real-time reverse transcription-polymerase chain reaction (two-step reactions). A standard sample with a known copy number was run along with unknown samples for a reverse transcription-polymerase chain reaction. Patients were further assessed for their clinical and molecular parameters during 6th month and 12th month of therapy.
Results:
All 78 new cases showed the presence of a viable load of bacilli at the time of recruitment, but we were able to follow up only on 36 of these patients for one year. Among these, using three different genes, 20/36 for esxA, 22/36 for hsp18 and 24/36 for 16S rRNA cases showed viability of M. leprae at the time of completion of 12 months of multidrug therapy treatment. All these positive patients were histopathologically active and had bacillary indexes ranging between 3+ and 4+. Patients with a high copy number of the Mycobacterium leprae gene, even after completion of treatment as per WHO recommended fixed-dose multidrug therapy, indicated the presence of live bacilli.
Limitations:
Follow up for one year was difficult, especially in Delhi because of the migratory nature of the population. Patients who defaulted for scheduled sampling were not included in the study.
Conclusion:
The presence of a viable load of bacilli even after completion of therapy may be one of the reasons for relapse and continued transmission of leprosy in the community.
Keywords
Leprosy
fixed duration multidrug therapy
efficacy
multibacillary leprosy
absolute quantification
Plain Language Summary
In endemic regions of several countries, the prevalence of leprosy has not come down to the level of elimination. On the contrary, new cases are being detected in large numbers from most of these areas in the majority of the endemic countries. Clinically, it is frequently noted that in spite of completion of a full course of multidrug therapy for 12 months, the lesions remain active, especially in cases with high bacteriological indices. Considering the above, the present study aimed at finding out the viability of Mycobacterium leprae strains from multidrug therapy-treated leprosy cases to find out their role in the transmission of disease. A total of 78 samples were collected initially to build up data on the viability of Mycobacterium leprae during multidrug therapy; samples were also collected at six months and 12 months intervals. Slit skin smears were collected from bacillary index (BI) positive new multibacillary leprosy cases in RNA Later vials (Sigma Co, USA.). RNAs were extracted from all the samples and were used for real-time polymerase chain reaction (two-step reaction). In our analysis, we observed that patients after one year of multibacillary multidrug therapy showed good signals for 16S rRNA, hsp18 and esxA genes, indicating that cases released from treatment were still harbouring viable bacilli in their system. We also observed that in this cohort of 36 patients, the Ct values of some of these samples increased for hsp18 and esxA genes (genes known to correlate with the growth of Mycobacterium leprae) even after 12 months of multidrug therapy. Presently, the multidrug therapy regimen has been shortened from two years to one year for multibacillary cases. It has been shown that the majority of relapses occur in multibacillary patients with Bl > 3+. By the time the patient was recognized as relapse, he/she might have infected several household contacts and neighbours. Viable Mycobacterium leprae from patients who have been released from treatment might have acted as the source for transmission of disease in the community, thus affecting the success of the leprosy eradication programme. The main aim of fixed duration multidrug therapy is to cure leprosy patients and to interrupt the transmission of leprosy to the community. Our study showed the positivity of viable bacilli in many patients after the completion of 12 months of multidrug therapy. Thus, it strongly suggests that the treatment regimen has to be redesigned for highly bacillated cases.
Introduction
Leprosy is a chronic infectious disease caused by Mycobacterium leprae inflicting skin and peripheral nerves and if left untreated may lead to disabilities due to nerve damage.1 Although administration of multidrug therapy has drastically brought down the prevalence rate to a state of elimination (<1 case per 10,000 population size), the rate/ratio of new case detection has not yet declined even though the figures of a WHO report show a decline in the detection on new cases since 2008.2 Out of the total new cases of the global population of leprosy, India alone had the major share of ≈ 60% cases (1,14,451 new cases) on record during the year 2019.3 In the recent past, the National Leprosy Eradication Programme carried out an innovative leprosy case detection campaign, which resulted in the detection of 34,000 new cases in 2016 from high endemic districts of the country. These cases accounted for 25% of new cases detected by the national programme in a year.4 In 2018, India reported 436 relapse cases out of a total number of 3361 in the world. It has been noted that relapse cases are mostly arising from multibacillary patients with high bacillary index ranging between 3+ and 5+ and who have completed the full regimen of multidrug therapy. This population of high bacillary index cases who are designated as “released from treatment” in an endemic region should ideally be free from viable bacilli but there will always remain dormant viable bacilli called “persisters,” which could be responsible for the occurrence of relapse. Moreover, by the time a relapse case is identified either in a field situation at a public health centre or in a tertiary care hospital, the patient might have transmitted infection to the household and neighboring contacts.
It has been mentioned that 99.9% Mycobacterium leprae are killed by rifampicin in active lepromatous patients.5 A highly bacillated (BI = 5+ to 6+) leprosy case has been estimated to have a Mycobacterium leprae load of 1010 to 1012 bacilli per gram of tissue.6 In such cases after a full course of multidrug therapy even after 99.9% bacillary killing, ≈107 to 109 per gram of tissue Mycobacterium leprae will remain viable and grow uninhibitedly because Mycobacterium leprae specific cell-mediated immunity does not get restored in such cases.7 It is known that most of the time in paucibacillary and lower BI multibacillary cases the remaining bacilli disappear progressively over several years due to the immune response of the individuals, which is why the relapse rate has been around 2% in most places. However, in highly bacillated cases, cellular immunity is negligible, and these 2% will be responsible for the transmission of the disease and might progress to reactional episodes, leading to disability. Further, even after completion of treatment with adequate doses of multidrug therapy, cases of drug resistance and multidrug resistance of Mycobacterium leprae are being reported from various countries.8-13 Relapse might occur either due to inadequate therapy, or after completing a full course of chemotherapy, which may vary from 0.6 to 3% in paucibacillary and 0.02– 0.8% in multibacillary cases due to wrong classification and insufficient therapy of PB cases. Further, a study has shown a relapse rate of 1.97/100 persons in multibacillary patients after 12 months of multi-drug therapy.14 Due to the occurrence of relapse in fully treated cases, questions arise about the efficacy of multidrug therapy in killing Mycobacterium leprae and in fully curing leprosy. At present, there is no satisfactory scientific method available for monitoring the efficacy of treatment in leprosy patients who relapse. As is well known, leprosy can also cause permanent damage if the patient remains without complete treatment or full cure.
Considering the above, the present work aimed at studying the efficacy of fixed duration multidrug therapy for multibacillary using real-time reverse transcription-polymerase chain reaction technology along with parameters of histopathological evidence of disease activity in high bacillary index cases.
Methods
Recruitment of patients
Seventy-eight new clinically confirmed leprosy patients were included in this study after taking written informed consent. These patients were recruited from the hospitals of The Leprosy Mission Trust India. Forty-two from Champa (Chhattisgarh), 20 from Naini (Uttar Pradesh) and 16 from Delhi (Delhi). The bacillary index in each sample was determined by acid-fast staining. Slit skin smear scrapings were collected in ribonucleic acid later from patients in field area and transported to the laboratory for further molecular diagnosis.
Inclusion and exclusion criteria
Newly diagnosed leprosy patients with bacillary index 2+ and above were included while leprosy patients with bacillary index less than 2+ were excluded from study [Table 1].
| Stage | BI 2+ to 3 | BI 3+ to 4 | BI 4+ to 5 | BI > 5+ | Total samples |
|---|---|---|---|---|---|
| Initial stage | 20 | 19 | 23 | 16 | 78 |
| After six months (follow-up) | 10 | 10 | 15 | 15 | 50 |
| After 12 months (follow-up) | 6 | 7 | 11 | 12 | 36 |
Histopathological investigation
The skin biopsies were processed for histopathological investigation. Biopsies were embedded in paraffin and serially sectioned at 5 µm thickness on a microtome. Sections of the skin biopsies were examined by haematoxylin and eosin (H&E) staining and modified Fite-Faraco technique for Mycobacterium leprae. Acid-fast bacilli were graded according to Ridley scale of 0 to 6+ as bacillary index of granuloma. The biopsy assessments were done using a standardized set of definitions for histological features.
Extraction of ribonucleic acid and preparation of complementary deoxyribonucleic acid from slit skin scrapings
Extraction of ribonucleic acid from slit skin scrapping of all patients was done by using TRIzol method15 with some minor modifications. Samples with ribonucleic acid later were centrifuged at a maximum speed of 14000 rpm and pellets were dissolved in TRIzol reagent (TRIzol® Reagent; Invitrogen) and Glycogen (20 µg/mL) (in 4:1 ratio) followed up by vortexing for proper mixing. Overnight precipitation of ribonucleic acid was done by using 0.75 volume of isopropanol at -20°C. Then the pellet of precipitated ribonucleic acid was washed with 70% ethanol. Extracted ribonucleic acid was dissolved in DEPC treated water and treated with DNase (Promega) before complementary deoxyribonucleic acid preparation. Complementary deoxyribonucleic acid was prepared as per the manufacturer’s instructions.
Real-time polymerase chain reaction analysis
Real-time polymerase chain reaction analysis was performed using genes targeting 16SrRNA, hsp18 and esxA [Table 2]. SYBR green assays were performed in 25 µL using SYBR green master mix (Agilent SYBR green mix). Primer concentration used in the reaction was 10 mM. Real-time polymerase chain reaction analyses were performed using the following optimized conditions: 10 minutes at 95°C followed by 30 seconds at 95°C, 60 seconds at 57°C and 30 seconds at 72°C for 40 cycles. Thai-53 reference strain as positive control and sterile water as a negative control was used for the individual experiment.
| Gene name | Primer orientation | Primer sequence | Amplicon size | Reference |
|---|---|---|---|---|
| 16SrRNA | Forward | 5’CGGAAAGGTCTCTAAAAAATCTT-3’ | 171 bp | Jadhav et al.2005 |
| 5’-CCTGCACCGCAAAAAGCTTTCC-3’ | ||||
| esx A | Forward | 5’-GAACTGCAAGGAAGCCAGAG-3’ | 161 bp | Part of this study |
| 5’-CCCAGTGCATGGTTTATTCC-3’ | ||||
| hsp18 | Forward | 5’-CTGGACATTGACATCGAACG-3’ | 204 bp | Part of this study |
| 5’-CCTTTCGGCTACTGGTATCG-3’ |
Determination of bacterial load
A standard curve for each polymerase chain reaction assay was generated by using serial 10-fold dilutions of purified Mycobacterium leprae deoxyribonucleic acid ranging from 10 ng to 10 fg. Unknown values were extrapolated automatically for each sample using the standard curve method and normalised using the data for the individual gene for the same sample. The viability of Mycobacterium leprae in human slit skin scrapings was determined by comparing normalized values of genes for patients prior to and up to one year after the start of multidrug therapy treatment.
Copy number of each assay was calculated by using the formula by Schmittgen and Livak16:
Copy number (molecules/μL) = [concentration (ng/μL) × 6.022 × 1023 (molecules/mol)]/ [length of amplicon × 650 (g/mol) × 109 (ng/g)].
Statistical analysis
Statistical analysis was performed by using Graph-Pad Prism Software (Version 6). Non-parametric Mann-Whitney U test was used to analyze the significant level of mRNA copy number across the series of the samples. A difference with a P-value <0.05 was considered statistically significant. Real-time polymerase chain reaction data was analysed by Rotor-Gene Q Series Software (Software version 2.0.2)
Limitations
Because of the migratory nature of the population, follow up of one year was difficult, especially in Delhi. Patients who defaulted for scheduled sampling were not included in the data.
Results
In our study, we used a method of quantifying bacteria by mRNA-based quantification, using real-time Q PCR.
Histopathology results
Sections of the skin biopsies were examined by haematoxylin and eosin staining and modified Fite-Faraco technique for Mycobacterium leprae at the time of recruitment and after completion of chemotherapy according to their bacillary index [Figure 1]. We did histology of a few representative samples at six and 12 monthly intervals of multidrug therapy. All these cases showed diffuse dermal infiltration with foamy macrophages with multiple solid-staining acid-fast bacilli. We observed that these patients, who were showing a viable load of bacilli at the time of release from treatment after a full course of fixed duration multidrug therapy, were also showing cellular activity on histopathology which showed the presence of granulomas [Figure 1].

- Histological findings as per treatment duration: (A) At the time of recruitment. Arrows showing active granuloma. (B) At the time of release from treatment at the 12th month (H & E stain × 400). Arrows showing foamy macrophages with acid fast bacilli and active granuloma in panel B
Development of standard curve for absolute quantification by determination of copy number of viable Mycobacterium leprae
For enumeration of a standard–curve, we performed the conventional polymerase chain reaction with three primer sets specific for three genes namely, 16SrRNA, hsp18 and esxA followed by gel elution and 10-fold serial dilutions. Mean crossing over points of three reactions of each dilution was plotted against log copy numbers to generate standard curve for absolute quantification [Figure 2].

- Preparation of a standard curve for absolute quantification of (A) 16srRNA qPCR, (B) esxA qPCR and (C) hsp18 qPCR. Standard curves were obtained by plotting log copy number of eluted deoxyribonucleic acid carrying the target genes, ranging from 107 to single copy, against the Ct value of the respective dilution
Amplification efficiency of the assay for 16srRNA, hsp18 and esxA genes were found to be 95.184% (Amplification factor = 1.952), 99.05% (Amplification factor = 1.99), 96.14 % (Amplification factor = 1.96), respectively.
Bacterial load in leprosy patients
Mycobacterium leprae genome data showed the presence of a single copy of 16SrRNA, hsp18 and esxA gene per chromosome. The copy number was calculated by absolute quantification in each sample. To avoid the variation in the results, the same concentration of ribonucleic acid and complementary deoxyribonucleic acid was used for absolute quantification for all the three genes in each sample.
In this study, we found a significant increase in copy numbers for all three gene sets, i.e., 16srRNA, hsp18 and esxA after the completion of multidrug therapy. The highest bacillary load in terms of maximum copy number was observed in cases with BI > 4+ at the time of recruitment for all three genes. There was consistent detection of viable load of bacilli during the course of treatment by 16S rRNA in 24 patients (66.6%), hsp18 gene in 22 patients (61.1%) and esxA in 20 patients (55.5%) [Figure 3].
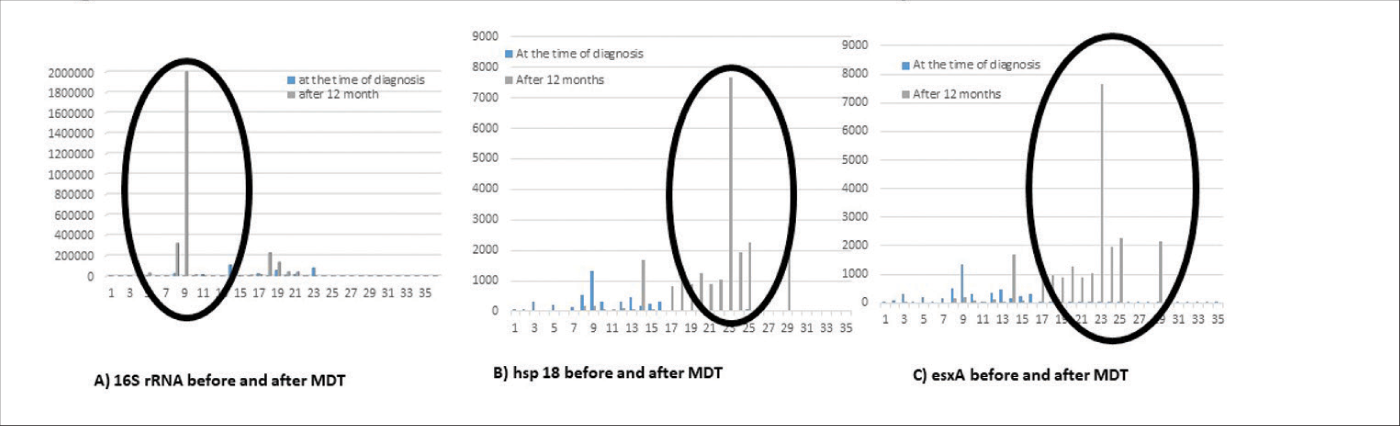
- Determination of viable load of bacilli before and after the completion of 12 months of multibacillary multidrug therapy. Total ribonucleic acid from 36 multibacillary leprosy patients was collected before the multidrug therapy treatment started and after 12 months of treatment completion. Copy numbers of 16SrRNA (A), hsp18 (B) and esxA (C) were calculated. The time point of the post-treatment stage (duration in months) at which the sample was collected from each patient is shown on the X-axis. Copy number of messenger ribonucleic acid before treatment and after multidrug therapy treatment is shown on the Y-axis
Discussion
Multidrug therapy has proved its effectiveness by bringing about a significant change in the prevalence of leprosy, both at the global and national level, by reducing the caseloads to the extent that leprosy no longer continues to be a major disease of public health importance. In addition, it has also been proved to be safe as well as acceptable to the patients.
Presence of viable Mycobacterium leprae in skin lesions has been noted after completion of the WHO fixed duration multidrug therapy regimen both in paucibacillary,17 and multibacillary patients.17-19 Jamil et al. have suggested that multibacillary cases with an initial average BI ≥ 4+ should receive at least four years of standard WHO multidrug therapy.20 Jethva et al. noted that 10% of the patients may continue to harbor live bacilli even after completion of two years of regular therapy.21 Some reports claim that the higher the bacillary index or shorter the duration of therapy, the higher the risk of relapse.22 Rigorous annual follow up for at least three years and even more for paucibacillary cases and nine years and even more for multibacillary cases must be observed.23
In our study, we targeted the 16srRNA, esxA and hsp18 genes, to determine the viability load in skin in patients at the time of their recruitment before introduction to multidrug therapy regimen (zero day), after six months and 12 months of multidrug therapy when released from treatment. In the recent past Davis et al.24 used quantitative real-time polymerase chain reaction expression for several gene targets of Mycobacterium leprae and correlated these with experimental mouse foot pad growth in both immunocompetent and immunosuppressed (nu/nu) mice and noted that hsp18 and esxA were the most expressive genes which correlated with the growth of Mycobacterium leprae. In our study, we observed a rise in expression of all three targets 16SrRNA, hsp18 and esxA gene targets in 24 (66.6%), 22 (61.1%) and 20 (55.5%), respectively, indicating that viable Mycobacterium leprae having the capacity to grow in a susceptible host are still present at the time of completion of treatment.
It was reported by Lini et al. that hsp18 gene is involved in the survival of pathogens under stressful conditions, which may account for the prolonged stability of hsp18 ribonucleic acid even during the period of chemotherapy.25 Earlier reports by Wakade & Shetty using the mouse foot pad system demonstrated the presence of viable bacilli in skin lesions of fully treated borderline tuberculoid patients.26 These results show that the presence of hsp18 mRNA in cases may indicate the viability of the pathogen. These findings support our findings of high levels of hsp18 mRNA in many patients at time of release from treatment.
The present finding demonstrates that this method could be adopted for specifically monitoring highly bacillated cases, to determine the need for continued multidrug therapy for longer periods. In addition to 16SrRNA, we included two more genes hsp18 and esxA in our study to know the viable load of bacilli having capacity to grow in lepromatous leprosy patients at the time of their release from treatment. We observed that the copy number of bacilli was up to ten,7 even at the time of release from treatment, in leprosy patients for both genes encoding hsp18 and esxA. A few studies have reported that the 16S rRNA signal remains for prolonged time even after the death of Mycobacterium leprae; because of that we included other two genes hsp18 and esxA in our study for the assessment of viability [Figure 3]. Increased copy number of hsp18 supports the findings of previous studies, which highlights the hsp18 gene association with stressful conditions. In all patients, the copy numbers of all the genes decreased gradually except for the group of 11 patients who were harbouring the viable load of bacilli, with BI > 4+ at the time of release from treatment [Figure 3]. Mouse foot pad assay has been used routinely to check the viability of the pathogen27 and it has been also shown that the prolonged presence of viable bacilli has the properties to resist antimicrobials. It has been recently shown that hsp18 of Mycobacterium leprae, a homologue in Mycobacterium tuberculosis expressed under stress conditions,28 and ESAT-6 protein expressing gene, esxA correlate with the exponential growth of Mycobacterium leprae in mouse foot pad. In the follow up cases after one year, some patients remained positive with viable bacilli having significant Mycobacterium leprae copy numbers with respect to 16SrRNA, hsp18 and esxA genes. These results highlight and support previous reports, which explain the role of hsp18 in stressful conditions, which may be one of the reasons for prolonged stability of ribonucleic acid after one year of multi-drug therapy.
From the present study, it could be concluded that borderline lepromatous/lepromatous leprosy patients with a high bacillary index could relapse after fixed-dose multidrug therapy for 12 months due to the growth of the remaining viable Mycobacterium leprae in these patients. As the Mycobacterium leprae specific cell-mediated immunity does not get restored in spite of fixed-dose multidrug therapy up to 12 months , the viable bacilli which are remaining find a favourable environment for their growth, which is noticed in nu/nu immunocompromised mice.24 Further, this incomplete therapy which is not destroying all bacterial cells and is responsible for relapse might also cause development of rifampicin resistant Mycobacterium leprae and appear as a secondary rifampicin-resistant case. Secondary resistance to rifampicin in multibacillary relapse cases has been reported across the globe.29,30 The main aim of fixed duration multidrug therapy is to cure leprosy patients and to interrupt the transmission of leprosy to the community. Therefore, it is desirable to treat/follow up on such cases until no viable bacilli remain in the patient.
Our study showed positivity of viable bacilli in many patients after the completion of 12 months of multidrug therapy. Thus, it strongly suggests that the treatment regimen has to be redesigned for highly bacillated cases. Therefore, the present regimen of multidrug therapy which advocates a fixed duration of treatment of 12 months for all multibacillary cases, irrespective of bacterial index, needs to be thoroughly debated and reconsidered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Indian Council of Medical Research (Grant No. 5/8/3(1)2013-ECD-I) and England and Wales Foundation (205T03).
References
- Infection with mycobacterium lepromatosis. Am J Trop Med Hyg. 2016;95:500-1.
- [CrossRef] [PubMed] [Google Scholar]
- WHO Weekly epidemiological record, No. 35. . 2018;93:445-456. (http://www.who.int/wer accessed on 28th March 2019)
- [Google Scholar]
- Central Leprosy Division, Directorate General of Health Services, Ministry of Health and Family Welfare Government of India, Nirman Bhavan, New Delhi.
- [Google Scholar]
- The bactericidal effect of rifampicin on M. leprae in man: A) single doses of 600 900 and 1200 mg; and b) daily doses of 300 mg. Int J Lepr Other Mycobact Dis. 1976;44:183-7.
- [Google Scholar]
- Reciprocity between regulatory t cells and th17 cells: Relevance to polarized immunity in leprosy. PLoS Negl Trop Dis. 2016;10:e0004338.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular detection of multidrug-resistant mycobacterium leprae from Indian leprosy patients. J Glob Antimicrob Resist. 2018;12:214-9.
- [CrossRef] [PubMed] [Google Scholar]
- Transmission of drug-resistant leprosy in guinea-conakry detected using molecular epidemiological approaches. Clin Infect Dis. 2016;63:1482-4.
- [CrossRef] [PubMed] [Google Scholar]
- Multidrug resistance to dapsone, rifampicin, and ofloxacin in Mycobacterium leprae. Lancet. 1997;349:103-4.
- [CrossRef] [PubMed] [Google Scholar]
- Multidrug resistant Mycobacterium leprae from patients with leprosy. Antimicrob Agents Chemother. 2001;45:3635-9.
- [CrossRef] [PubMed] [Google Scholar]
- A Mycobacterium leprae isolate resistant to dapsone, rifampin, ofloxacin and sparfloxacin. Int J Lepr Other Mycobact Dis. 2000;68:452-5.
- [Google Scholar]
- A second case of multidrug-resistant mycobacterium leprae isolated from a Japanese patient with relapsed lepromatous leprosy. Int J Lepr Other Mycobact Dis. 2003;71:240-3.
- [CrossRef] [PubMed] [Google Scholar]
- Twelve months fixed duration WHO multidrug therapy for multibacillary leprosy: Incidence of relapses in Agra field-based cohort study. Indian J Med Res. 2013;138:536-40.
- [Google Scholar]
- Identification of differentially expressed mRNA in prokaryotic organisms by customized amplification libraries (DECAL): The effect of isoniazid on gene expression in mycobacterium tuberculosis. Proc Natl Acad Sci U S A. 1998;95:13227-32.
- [CrossRef] [PubMed] [Google Scholar]
- Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3:1101-8.
- [CrossRef] [PubMed] [Google Scholar]
- Viability and drug susceptibility testing of M. leprae using mouse footpad in 37 relapse cases of leprosy. Int J Lepr Other Mycobact Dis. 2003;71:210-7.
- [CrossRef] [PubMed] [Google Scholar]
- Are viable mycobacterium leprae present in lepromatous patients after completion of 12 months' and 24 months' multi-drug therapy. Indian J Lepr. 2004;76:199-206.
- [Google Scholar]
- Persister studies in leprosy patients after multi-drug treatment. Int J Lepr Other Mycobact Dis. 2005;73:100-4.
- [Google Scholar]
- Relapse after long-term follow up of multibacillary patients treated by WHO multidrug regimen. Marchoux chemotherapy study group. Int J Lepr Other Mycobact Dis. 1995;63:195-201.
- [Google Scholar]
- Study of 35 cases of hansen's disease, which required treatment beyond fixed duration-multi drug therapy. Indian J Lepr. 2015;87:79-83.
- [Google Scholar]
- Fixed-duration therapy in leprosy: Limitations and opportunities. Indian J Dermatol. 2013;58:93-100.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features and diagnosis of relapses in leprosy. Indian J Lepr. 1995;67:45-59.
- [Google Scholar]
- Molecular assays for determining mycobacterium leprae viability in tissues of experimentally infected mice. PLoS Negl Trop Dis. 2013;7:e2404.
- [CrossRef] [PubMed] [Google Scholar]
- Quantitative real-time PCR analysis of Mycobacterium leprae DNA and mRNA in human biopsy material from leprosy and reactional cases. J Med Microbiol. 2009;58:753-9.
- [CrossRef] [PubMed] [Google Scholar]
- Isolation of Mycobacterium leprae from untreated borderline tuberculoid, mid-borderline and indeterminate cases using the mouse foot pad technique-a study of 209 cases. Lepr Rev. 2006;77:366-70.
- [CrossRef] [Google Scholar]
- Detection of mRNA transcripts and active transcription in persistent mycobacterium tuberculosis induced by exposure to rifampin or pyrazinamide. J Bacteriol. 2000;182:6358-65.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of reactive nitrogen intermediates on gene expression in Mycobacterium tuberculosis. Cell Microbiol. 2003;5:637-48.
- [CrossRef] [PubMed] [Google Scholar]
- Drug resistance patterns in mycobacterium leprae isolates from relapsed leprosy patients attending the leprosy mission (TLM) hospitals in India. Lepr Rev. 2014;85:177-85.
- [CrossRef] [PubMed] [Google Scholar]
- Emergence and transmission of drug-/multidrug-resistant mycobacterium leprae in a former leprosy colony in the Brazilian Amazon. Clin Infect Dis. 2020;70:2054-61.
- [CrossRef] [PubMed] [Google Scholar]






