Translate this page into:
Efficacy of topical 5% fluorouracil needling in vitiligo
Correspondence Address:
Sneha Gandhi
Room No. 9, Skin OPD, Bapuji Hospital, MCC B Block, Davangere, Karnataka
India
| How to cite this article: Shashikiran A R, Gandhi S, Murugesh S B, Kusagur M, Sugareddy. Efficacy of topical 5% fluorouracil needling in vitiligo. Indian J Dermatol Venereol Leprol 2018;84:203-205 |
Sir,
Although vitiligo is a disease known since ancient times, the search for an optimal treatment still continues. Despite the availability of numerous medical and surgical treatment options, a single universally reliable therapeutic modality is yet to emerge due to variability of response rate in different patients.[1]
Topical 5% fluorouracil is one of the less popular weapons in the armamentarium for the treatment of vitiligo. It has been tried earlier in combination with dermabrasion and lasers. These procedures, however, often require a special setup with a deep learning curve, and the cost tends to deprive the patients from lower socioeconomic strata, of these modalities. Our aim is to provide a safe, effective, and easily reproducible modality for the treatment of vitiligo using topical 5% fluorouracil.
We conducted an open, non randomized, single-arm study to observe the safety and efficacy of needling following topical 5% fluorouracil application on patches of stable vitiligo. Thirty-nine patients with a total of 100 patches were included in this prospective clinical study conducted from July 2014 to December 2015 after obtaining approval from the ethical committee at the department of dermatology, JJM Medical College, Davanagere.
Patients with disease stability of at least one year duration, who consented to be a part of the study, were included whereas patients with active Koebner's phenomenon, age less than 10 years, and patches on the face, genitalia, and intertriginous areas were excluded from the study. Each patch was initially outlined on a transparent over head projector (OHP) sheet and photographed. The duration of each patch, presence of other prognostic factors including leukotrichia, site, and the treatment taken previously were recorded.
Under aseptic precautions, a thick paste of 5% fluorouracil cream is applied on the patch followed by needling with a 26-G needle. The needling points are placed as close as possible to each other. A lag period of few seconds between the time of needling and appearance of pin point bleed indicates that the needle has reached the dermo-epidermal junction. Following this, the area is cleaned with betadine and equal quantities of 5% fluorouracil and a topical antibiotic cream applied on the treated area and dressed.
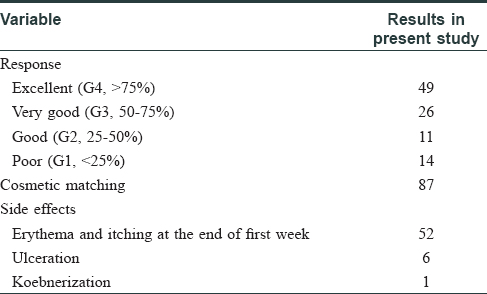
The patients are then advised to apply a mixture of 5% fluorouracil and antibiotic cream twice daily for 15 days. 5% fluorouracil needling was done once a month for 3 consecutive months; serial photographs were taken; and the patients were followed up for 6 months. Repigmentation was categorized as <25% (poor-G1), 25–50% (good-G2), 50–75% (very good-G3), and >75% (excellent-G4). G3 and G4 grades were considered as the desirable outcomes.
The patients' age in our study ranged from 13 years to 44 years. The female-to-male ratio was 1.7:1, and the duration of vitiligo ranged from 1.2 years to 11.5 years with a mean duration of 4.9 years. The different morphological types of vitiligo were vitiligo vulgaris in 23 (58%) patients, acrofacial in 13 (34%) patients, and focal vitiligo in 3 (8%) patients. Out of the 100 patches, 49 were on the limbs, 36 on the trunk/abdomen, and 15 patches were distributed acrally.
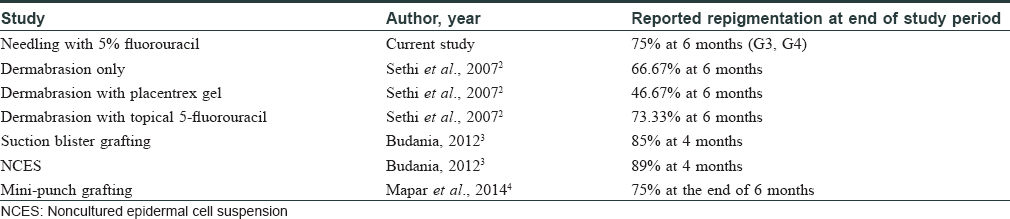
More than 75% repigmentation (excellent response) [Figure - 1] was noted in 49% of the patches. Very good response with 50–75% repigmentation [Figure - 2] was seen in 26% of the patches 25–50% repigmentation in 11% of the patches, whereas 14% of the patches responded poorly with less than 25% repigmentation [Table - 1]. This efficacy was found to be comparable to other surgical modalities [Table - 2]. The rate of pigmentation was rapid in approximately 8% of the patches, which developed 100% repigmentation within the first month. Among the responders, the cosmetic matching of the repigmentation area was excellent (87%). Approximately 8% of the patients initially developed hyperpigmentation, which returned to normal skin color during the follow-up period. The repigmentation was stable throughout the follow-up period of 6 months except in one patient who had recurrence of depigmentation and development of new lesions.
 |
| Figure 1a: Two depigmented patches of vitiligo before treatment |
 |
| Figure 1b: Two depigmented patches of vitiligo 1 month after first sitting showing both marginal and perifollicular repigmentation |
 |
| Figure 1c: Two depigmented patches of vitiligo after three sittings |
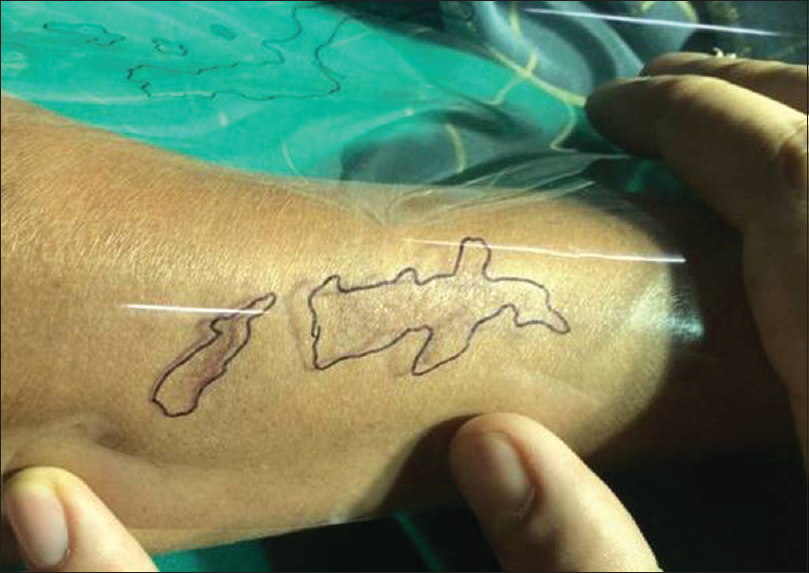 |
| Figure 1d: Complete pigmentation of the patches with cosmetic matching at the end of six months |
 |
| Figure 2: Patches showing >50% repigmentation (G3 and G4) at the end of 6 months |
Truncal lesions had the best response while the least responsive ones were located acrally. The factors associated with poor outcome in our study were leucotrichia, bony prominence, and acral location. These findings are in concordance with the literature.[2]
Topical application of 5% fluorouracil either alone or in combination with dermabrasion has been reported in the literature. Though the exact mechanism is not known, several possible theories are proposed to explain the repigmentation. – One such theory is that 5%- fluorouracil causes overstimulation of the melanocytes of the follicles, which migrate during epithelization to the surface, thereby inducing pigmentation.[2],[5]
The adverse effects recorded in our study include pain during the procedure (100%), erythema and itching in the first week post procedure (52%), ulceration (6%), and koebnerization (1%) [Table - 2]. These adverse effects are much milder compared to those observed on combining dermabrasion with topical 5-fluorouracil. Sethi et al. reported erythema and serous discharge in all patients, formation of pseudomembrane, and hypertrophic scarring in a study which combined dermabrasion with topical 5-flurouracil.[2]
The results from this study indicate that topical 5% fluorouracil needling is an efficacious, safe, easy, and reproducible method of repigmentation in vitiligo not responding to the medical line of therapy. The limitation of our study is that no control group was included.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Schallreuter KU, Bahadoran P, Picardo M, Slominski A, Elassiuty YE, Kemp EH, et al. Vitiligo pathogenesis: autoimmune disease, genetic defect, excessive reactive oxygen species, calcium imbalance, or what else? Exp Dermatol 2008;17:139-40.
[Google Scholar]
|
| 2. |
Sethi S, Mahajan BB, Gupta RR, Ohri A. Comparative evaluation of the therapeutic efficacy of dermabrasion, dermabrasion combined with topical 5% 5-fluorouracil cream, and dermabrasion combined with topical placentrex gel in localized stable vitiligo. Int J Dermatol 2007;46:875-9.
[Google Scholar]
|
| 3. |
Budania A, Parsad D, Kanwar AJ, Dogra S. Comparison between autologous noncultured epidermal cell suspension and suction blister epidermal grafting in stable vitiligo: a randomized study. Br J Dermatol 2012;167:1295-301.
[Google Scholar]
|
| 4. |
Mapar MA, Safarpour M, Mapar M, Haghighizadeh MH. A comparative study of the mini-punch grafting and hair follicle transplantation in the treatment of refractory and stable vitiligo. J Am Acad Dermatol 2014;70:743-7.
[Google Scholar]
|
| 5. |
Ortonne JP, MacDonald DM, Micoud A, Thivolet J. PUVA-induced repigmentation of vitiligo: a histochemical (split-DOPA) and ultrastructural study. Br J Dermatol 1979;101:1-12.
[Google Scholar]
|
Fulltext Views
9,120
PDF downloads
2,257





