Translate this page into:
Elastosis linearis rubra nasi: A new clinical entity in the spectrum of localized nodular elastosis
2 Department of Dermatology P.D. Hinduja Hospital, Mahim, Mumbai, Maharashtra, India
Correspondence Address:
Shyam Bhanu Verma
18 Amee Society, Diwalipura, Vadodara -390 015, Gujarat
India
| How to cite this article: Verma SB, Joshi RS. Elastosis linearis rubra nasi: A new clinical entity in the spectrum of localized nodular elastosis. Indian J Dermatol Venereol Leprol 2015;81:62-64 |
Sir,
Sun damaged skin (actinic or solar elastosis) presents clinically with dry skin showing diffuse thickening and beading of skin, yellow-sallow color, loss of elasticity leading to prominent wrinkling and accentuation of normal skin markings. In severe cases, telangiectasia and pigmentary changes (poikiloderma) may occur. These changes are usually diffuse and affect almost all areas chronically exposed to the sun. Histopathological correlates are a thin and flattened epidermis with a thin papillary dermis which appears as a Grenz zone between the epidermis and the upper reticular dermis. The upper reticular dermis has thickened, curled and serpiginous, tangled basophilic fibers. At times, masses of elastotic material with loss of outlines of individual fibers are seen without any significant inflammatory infiltrates. [1]
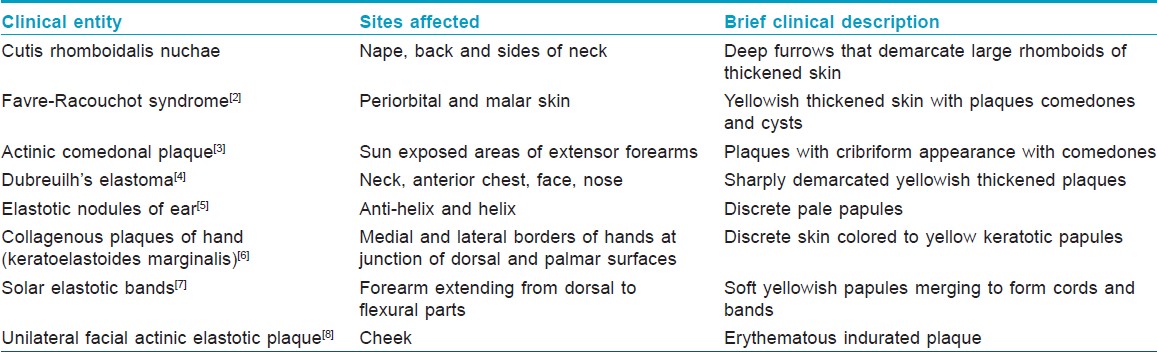
While these changes are seen in all skin chronically exposed to the sun, several case reports have appeared in the literature wherein localized nodular collections of elastotic material in the upper and or mid-reticular dermis have been described as the main histopathological finding, without any other associated skin disease. Such cases have had varied clinical presentations affecting different body sites such as localized papules, plaques, bands, etc., with or without comedones. These ′′nodular elastotic conditions′′ have been described under various names [Table - 1]. [2],[3],[4],[5],[6],[7],[8]
We describe a case of nodular solar elastosis with a clinical presentation that does not appear to have been described previously. We suggest the term elastosis linearis rubra nasi to describe it.
A 50-year-old Indian woman with Fitzpatrick phototype V, presented with an asymptomatic, gradually growing, linear, red plaque on her nose for the past 6 months [Figure - 1]. It started from the root of the nose (nasion) about 4 mm from the midline and extended all the way down about 4 mm parallel to the tip of the nose. It was firm to feel, slightly indurated and blanched on pressure. There was no scaling, crusting, oozing or ulceration at any point. She did not have significant wrinkling or sallowness and her skin did not appear to be abnormal or overtly sundamaged. There were no comedones, papules or plaques on the face. The patient said that the lesion became a little more prominent and red whenever there was prolonged sun exposure. She also claimed that it increased when she spent long hours in the kitchen in front of the stove where she cooked over a gas flame. She was in good health and was not taking photosensitizing drugs for any medical problems. There was no history of trauma and no indicators in her history to suggest it to be a factitial process. Her hematologic and biochemical parameters were within normal limits. A clinical differential diagnosis of morphea was considered and a 3 mm punch biopsy was performed.
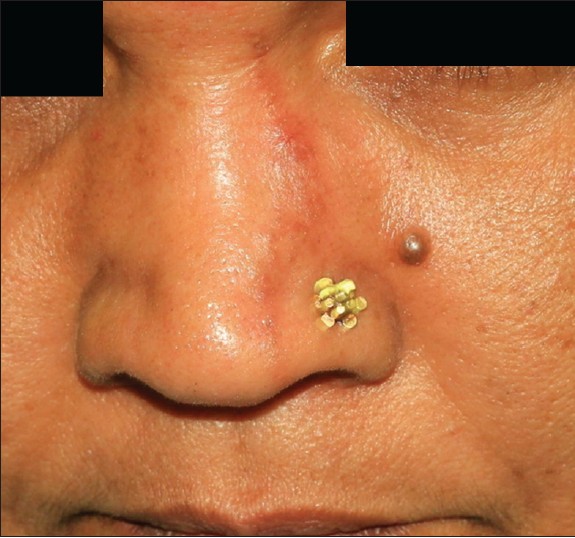 |
| Figure 1: Linear erythematous plaque on left side of nose |
Histopathology showed a flattened epidermis with several large melanocytes at the dermo-epidermal junction. The upper reticular dermis had, in several foci, nodular collections of deeply basophilic elastotic material and homogenized connective tissue separated from the flattened epidermis by a narrow clear Grenz zone [Figure - 2]. This altered basophilic material on staining with Van Geison stain showed fragmented tortuous elastic fibers [Figure - 3]. The rest of the dermis showed mild alteration of elastic fibers and normal appendages. There was no mucin, amyloid or colloid material. The upper dermis had a few thin walled telangiectatic vessels and a moderately dense perifollicular lymphocytic infiltrate. The upper dermis appeared to be slightly fibrotic with scattered fibrocytes, but no sclerotic collagen was seen.
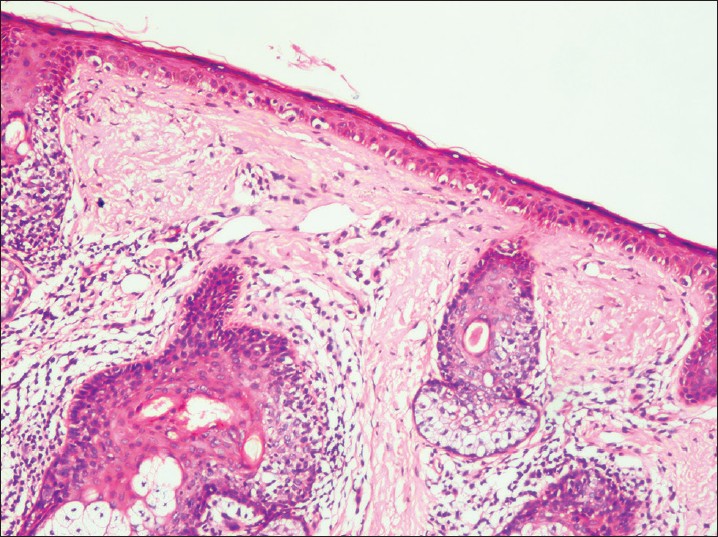 |
| Figure 2: Flat epidermis with increased numbers of melanocytes, telangiectatic vessels in the upper dermis with a moderately dense perifollicular lymphocytic infiltrate and two foci with nodular elastosis in the upper reticular dermis. (H and E, ×100) |
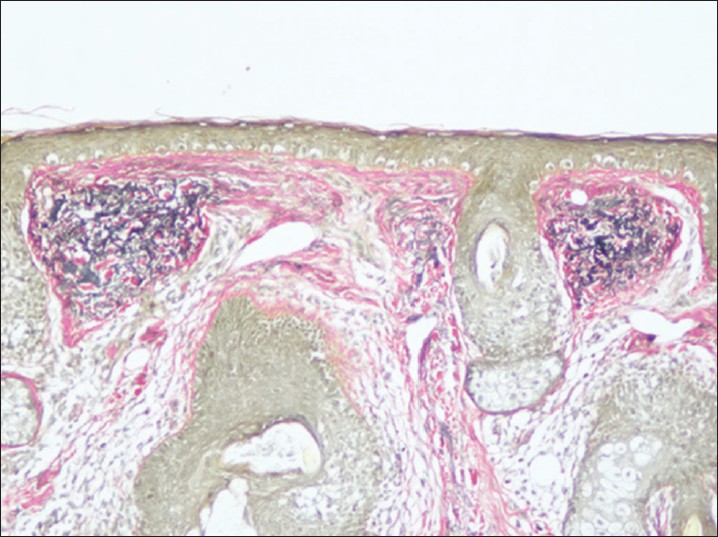 |
| Figure 3: Elastic stain showing two nodules of black elastotic material in the upper reticular dermis. (Van Gieson, ×100) |
Our case has nodular solar elastosis with some features similar to a single case report of ′′unilateral facial actinic elastotic plaque′′ [8] that has been described in a 82-year-old Caucasian woman in Australia who presented with an ill defined tumor-like indurated plaque on the left cheek with prominent erythema which worsened on palpation of the lesion and which showed nodular elastotic material in the dermis without any deposition of amyloid or colloid material. While there was significant solar damage to the entire face evidenced by marked wrinkling, pigmentary changes and a sallow appearance, the plaque showed elastotic damage which exceeded that seen in the surrounding skin.
Most of the nodular actinic elastotic entities have been described in elderly persons who also had clinical features of actinic damage over the rest of the face and exposed areas. Our patient, in contrast, was younger in age and clinically did not show any appreciable actinic damage to the skin of the face, a phenomenon we find difficult to explain. However, she did have a long standing history of sun exposure while working on her farm as well as exposure to heat and infrared radiation while working in the kitchen.
Elastotic degeneration of the dermis has been suggested to occur due to actinic stimulation of fibroblasts and appears to result from transcriptional activation of the elastin gene. [1] DNA photo damage and UV damage induced reactive oxygen species are the initial molecular events that lead to the clinical and histological findings in chronic photodamage of the skin. [1]
Finlayson et al. have described a form of elastosis secondary to heat/infrared radiation in patients with erythema ab igne. [9] They found elastosis in the dermis of three patients with erythema ab igne which was similar to that seen in actinically damaged skin and suggested that both actinic elastosis seen in sun damaged skin and secondary elastosis seen in erythema ab igne might have a similar pathophysiology. The events leading to elastosis are likely to be caused by lysosomal labilizers like ultraviolet and infrared radiation with release of lysosomal enzymes that damage collagen of the dermis leading to accumulation of altered elastotic tissue. [3]
| 1. |
Solar (Actinic) elastosis. In: Weedon D, editor. Weedon's Skin Pathology. 3 rd ed. Philadelphia: Churchill Livingstone; 2010.p. 341-2.
rd ed. Philadelphia: Churchill Livingstone; 2010.p. 341-2.'>[Google Scholar]
|
| 2. |
Helm F. Nodular cutaneous elastosis with cysts and comedones. (Favre-Racouchot syndrome). Report of a case.Arch Dermatol 1961; 84:666-8.
[Google Scholar]
|
| 3. |
Eastern JS, Martin S. Actinic comedonal plaque. J Am Acad Dermatol 1980; 3:633-6.
[Google Scholar]
|
| 4. |
Degos R, Touraine R, Civatte J, Belaich S. Elastome en nappe du nez. Bull Soc Fr Dermatol Syphiligr 1966;73:123-4.
[Google Scholar]
|
| 5. |
Carter VH, Constantine VS, Poole WL. Elastotic nodules of the antihelix. Arch Dermatol 1969; 100:282-5.
[Google Scholar]
|
| 6. |
Kocsard E. Keratoelastoidosis marginalis of the hands. Dermatologica 1965:131:169-75.
[Google Scholar]
|
| 7. |
Raimer SS, Sanchez RL, Hubler WRJr, Dodson RF. Solar elastotic bands of the forearm: An unusual clinical presentation of actinic elastosis. J Am AcadDermatol 1986; 15:650-6.
[Google Scholar]
|
| 8. |
Wittal RA, Georgouras KE, Baird PJ, Cleary EG, Henderson M. Unilateral facial actinic elastotic plaque - A new clinical variant of actinic elastosis. Australas J Dermatol 1989;30:15-22.
[Google Scholar]
|
| 9. |
Finlayson GR, Sams WMJr, Smith JG Jr. Erythema abigne: A histopathological study. J Invest Dermatol 1966; 46:104-8.
[Google Scholar]
|
Fulltext Views
3,823
PDF downloads
3,094





