Translate this page into:
Electrochemotherapy for a locally advanced basal cell carcinoma on the forehead
2 Department of Experimental and Clinical Medicine, DISM, Institute of Dermatology, University of Udine, Italy
Correspondence Address:
Nicola di Meo
Department of Dermatology, Maggiore Hospital of Trieste, IV Floor Palazzina Infettivi, University of Trieste, Trieste, 34151
Italy
| How to cite this article: Gatti A, Stinco G, di Meo N, Noal C, Maione V, Trevisan G. Electrochemotherapy for a locally advanced basal cell carcinoma on the forehead. Indian J Dermatol Venereol Leprol 2014;80:378-380 |
Sir,
Electrochemotherapy (ECT) is an effective loco-regional therapy for solid skin cancers with a high overall objective response rate and good cosmetic results. It is used for the treatment of cutaneous and subcutaneous tumour nodules where standard treatments have failed or proved to be inappropriate. It is mainly indicated in melanoma, Kaposi sarcoma, and cutaneous or subcutaneous metastases. Recent studies have focused on its role in the treatment of cutaneous tumours, in particular basal cell carcinoma (BCC) and squamous cell carcinoma of the head and neck. [1],[2]
This therapeutic modality is based on the combination of electroporation and the administration of cytotoxic low permeability drugs. Electroporation uses pulsed, high-intensity electric fields to temporarily increase cell membrane permeability by creation of pores, thereby allowing non-permeable chemotherapeutic agents to enter the cells. These electric pulses also increase the cytotoxicity of the drugs. Bleomycin and cisplatin are the two commonly used drugs in this method. [3] The clinical procedures for a standardized, efficient and safe electric pulse and drug administration protocol for electrochemotherapy are provided by the results of a multicenter European Standard Operating Procedure of Electrochemotherapy (ESOPE). [4] We report our experience in a case of basal cell carcinoma.
A 54-year-old man presented with a pigmented and deep infiltrating plaque localized over the forehead. The lesion represented a relapsed basal cell carcinoma confirmed by histopathology [Figure - 1]a and b. He was operated with Moh′s surgical technique one year earlier, but the lesion relapsed at the same site [Figure - 2]a. We offered electrochemotherapy as a treatment option as he refused surgical intervention. A bolus of bleomycin and an electrical pulse generator was used under general anesthesia following the ESOPE guidelines. Bleomycin was administered intravenously in a dosage of 30000 IU followed by the application of electric pulses directly over the tumour. We used a linear field of 20 mm and the median time of treatment was 30 minutes. The procedure was well tolerated and led to a rapid clinical regression of the lesion. At one year of follow up, mild scarring with hyperpigmentation was seen over the treated site [Figure - 2]b. There was no evidence of relapse on histopathological and dermoscopic examination.
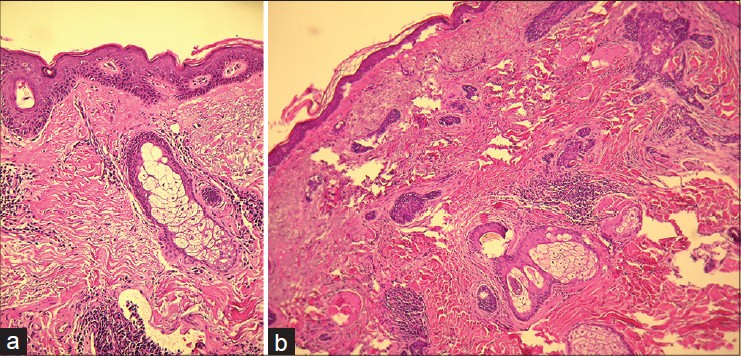 |
| Figure 1: (a) Basal cell carcinoma (H and E, ×40). (b) Infiltrative growth of basal cell carcinoma (H and E, ×40) |
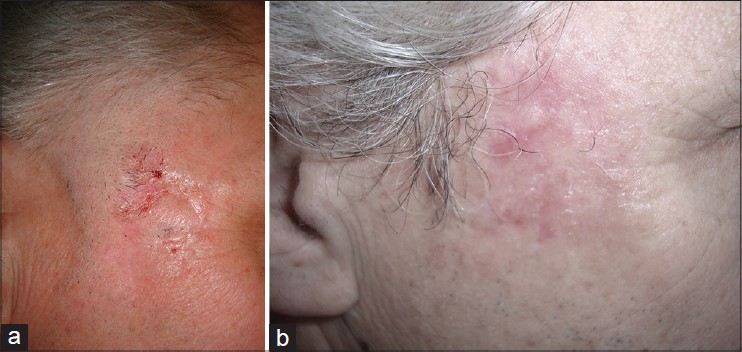 |
| Figure 2: (a) A deep, infiltrating plaque localized over the forehead. (b) Post-electrochemotherapy, at one year follow up, with mild scarring and hyperpigmentation |
Basal cell carcinoma is the most common cutaneous malignant neoplasm, accounting for up to 80% of non melanoma skin cancers and has an estimated annual incidence of 0.1 to 0.5% in the United States. Surgery is the standard treatment but in some cases there could be a progression or relapse of the disease. Treatment must be individualized according to the patient and depends upon the location, size, tumour sub-type, patient preferences and on the cost effectiveness of therapy. Due to the location, there was a risk of facial nerve damage during surgery. Biological therapies such as epidermal growth factor receptor or Hedgehog inhibitor are costly [5] . Electrochemotherapy is a low risk therapeutic option with good clinical and aesthetic results. Its use in locally advanced basal cell carcinoma has not been standardized yet. It has been reported that electrochemotherapy with bleomycin sulphate gave the best response rates in basal cell carcinoma among a variety of primary and secondary skin tumours with a complete response in up to 94.4% of cases after one treatment session. [5]
Potential contraindications to this technique include poor renal function, arrhythmia, pacemaker use and pulmonary fibrosis. A number of studies have shown that electrochemotherapy is associated with a good overall response rate. Gargiulo et al., [2] reported no recurrences during a mean follow-up of 20 months in a non-randomised study of 34 patients including 20 patients with BCC, and improved local tumour control with repeated electrochemotherapy. The only side effects reported are mild and transient erythema and oedema which resolve within 24 hours. In peculiar locations such as the orbit or eye muscles, electrochemotherapy does not cause significant dysfunctional outcome. A septal cartilage perforation was reported in 1 patient receiving treatment in the right nasal vestibule. [2]
Therapeutic response occurs without any increased morbidity for the patient with tissue-sparing and low risk due to the minimal dose of chemotherapy, local anaesthesia, absence of surgical wounds, good aesthetic results, brief hospitalization and high compliance of the patient. Furthermore, the absence of systemic side effects and low immunosuppression even with repeated doses make this a suitable technique for elderly patients with poor general condition or co-morbidities. In conclusion, this technique appears to be well tolerated, safe and repeatable. In our case, this approach gave very satisfying results with no recurrence and a good aesthetic outcome at follow up one year later. Our experience, along with that of others, demonstrates that electrochemotherapy with intravenous or intra-tumour bleomycin is an effective treatment option for patients with advanced basal cell carcinoma.
| 1. |
Mevio N, Bertino G, Occhini A, Scelsi D, Tagliabue M, Mura F, et al. Electrochemotherapy for the treatment of recurrent head and neck cancers: Preliminary results. Tumori 2012;98:308-13.
[Google Scholar]
|
| 2. |
Gargiulo M, Papa A, Capasso P, Moio M, Cubicciotti E, Parascandolo S. Electrochemotherapy for non-melanoma head and neck cancers: Clinical outcomes in 25 patients. Ann Surg 2012;255:1158-64.
[Google Scholar]
|
| 3. |
Reinhold U. Electrochemotherapy for primary skin cancer and skin metastasis related to other malignancies. Anticancer Drugs 2011;22:711-8.
[Google Scholar]
|
| 4. |
Testori A, Tosti G, Martinoli C, Spadola G, Cataldo F, Verrecchia F, et al. Electrochemotherapy for cutaneous and subcutaneous tumor lesions: A novel therapeutic approach. Dermatol Ther 2010;23:651-61.
[Google Scholar]
|
| 5. |
Ali FR, Lear JT. Systemic treatments for basal cell carcinoma (BCC): The advent of dermato-oncology in BCC. Br J Dermatol 2013;169:53-7.
[Google Scholar]
|
Fulltext Views
2,559
PDF downloads
1,862





