Translate this page into:
Enalapril induced normocomplementemic urticarial vasculitis
Correspondence Address:
Savita Koregol
Mahesh Nilaya, Near Muchakhandi Cross, Belgaum Road, Bagalkot - 587 101, Karnataka
India
| How to cite this article: Koregol S, Naidu V, Rao S, Ankad B S. Enalapril induced normocomplementemic urticarial vasculitis. Indian J Dermatol Venereol Leprol 2015;81:73-74 |
Sir,
Urticarial vasculitis usually occurs without a detectable cause or due to underlying connective tissue disorders; drug-induced disease is rare. Cutaneous changes occur frequently in adverse drug reactions, and account for 1-3% of drug reactions in hospitalized patients. Drugs have often been implicated in the etiology of vasculitis and are reported to cause approximately 10% of the cases of vasculitis. [1] We report a case of enalapril-induced normocomplementemic urticarial vasculitis. We were unable to find any previous reports of this association.
A 71-year-old obese male presented with complaints of painful and itchy skin lesions over the trunk for 4 days. On examination, wheals with underlying erythema were present over the abdomen [Figure - 1]. One week prior to the onset of these lesions, he was diagnosed to have hypertension and started on enalapril 5 mg once daily every morning. He started to develop skin lesions after taking the drug for 8 days. He had no history of similar complaints in the past, swelling of lips or difficulty in breathing. There was no history of joint pain, oral ulcers, photosensitivity, dryness of mouth and eyes, loss of weight or appetite, or any other family history of similar complaints. He was a diabetic taking oral hypoglycemic agents for 3 years and aspirin for ischemic heart disease for 2 years.
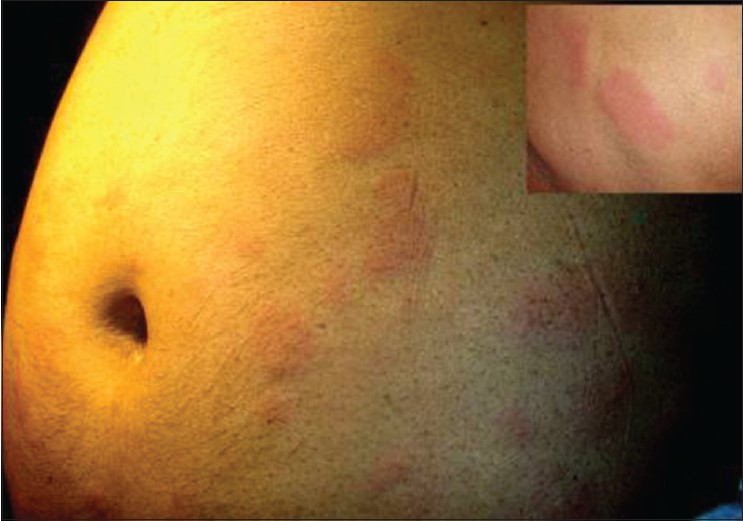 |
| Figure 1: Annular wheals over the abdomen; inset shows a magnified view of the individual lesion |
We advised the patient to return after 72 hours to check for clearance or persistence of the wheals while the patient was still on enalapril. On repeat examination after 72 hours, the wheals still persisted over the abdomen and a few new lesions appeared over the thighs. We arrived at a provisional diagnosis of drug induced urticarial vasculitis based on the history and clinical examination. Histopathological examination revealed a normal epidermis and dermis with perivascular infiltration by neutrophils, lymphocytes, and a few eosinophils. Prominent edema of dermis was noted. The vessel walls showed minimal fibrin deposits, leukocytoclasis, and erythrocyte extravasation, which was suggestive of urticarial vasculitis. The routine laboratory investigations, which included hemogram, liver and renal function tests were within normal limits. Other causes of vasculitis were ruled out with negative results for antinuclear antibodies, antineutrophil cytoplasmic antibodies, cryoglobulins, hepatitis B and C, and rheumatoid factor serology. The serum protein electrophoresis and serum concentrations of C3 and C4 were normal. We advised the patient to stop enalapril and administered systemic corticosteroids. After a week, lesions started to subside leaving behind residual purpura.
Side effects of enalapril include angioedema, brassy cough, insomnia and dry mouth. Urticarial vasculitis presents as urticarial lesions most often over the trunk or proximal limbs, frequently with associated angioedema. Unlike simple urticarial these lesions persist for more than 24 hours, demonstrate purpura and postinflammatory pigmentation, and cause symptoms of burning and pain. [2] Urticarial vasculitis is commonly associated with connective tissue diseases with a prevalence of 32% in Sjogren′s syndrome and 20% in systemic lupus erythematosus. It is also associated with physical urticaria, hepatits B or C infection, IgM or IgA gammopathies, serum sickness, colonic cancer, and drug ingestion. [2]
Drug induced urticarial vasculitis has been previously reported secondary to glatiramer acetate in a 48-year-old female undergoing treatment for multiple sclerosis. [3] A 72-year-old woman treated for diabetes with glimepride developed leukocytoclastic vasculitis as reported by Salem et al. [4] The diagnosis of drug-induced vasculitis is based on exclusion of known causes of vasculitis, histopathological correlation, the patient′s drug exposure, and improvement of the symptoms when the suspected drug is withdrawn. [5]
This case was labelled as normocomplementemic urticarial vasculitis secondary to enalapril. The positive indicators were an underlying history of enalapril intake for hypertension, wheals that resolved after a period of more than 72 hours, normal complement levels of C3 and C4 and histopathological findings in favour of vasculitis.
| 1. |
Demoly P, Viola M, Gomes ER, Romano A. Epidemiology and causes of drug hypersensitivity. In: Pichler WJ, editors. Drug hypersensitivity. 1 st ed. New York: Karger publisher; 2007. p. 168-89.
[Google Scholar]
|
| 2. |
Breathnach SM. Vasculitis, Neutrophilic dermatoses and related disorders. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 8 th ed. Oxford, UK: Blackwell; 2010. p. 50.21-3.
th ed. Oxford, UK: Blackwell; 2010. p. 50.21-3.'>[Google Scholar]
|
| 3. |
Kandi B, Oguz S, Cobanoglu B, Bulut S, Saral Y. An urticarial vasculitis case induced by glatiramer acetate. J Dermatolog Treat 2008;19:305-7.
[Google Scholar]
|
| 4. |
Ben Salem C, Hmouda H, Bouraoui K. Glimepiride-induced vasculitis: A case report. Br J Clin Pharmacol 2007;64:113-4.
[Google Scholar]
|
| 5. |
Elkyan O, Yaron M, Caspi D. Minocycline-induced autoimmune syndromes: An overview. Semin Arthritis Rheum 1999;28:392-7.
[Google Scholar]
|
Fulltext Views
3,515
PDF downloads
2,709





