Translate this page into:
Enthesopathy in patients with nail psoriasis – a cross-sectional evaluation of clinical, onychoscopic and ultrasonographic features
Corresponding author: Dr. Chander Grover, Professor, Department of Dermatology and STD, University College of Medical Sciences (UCMS) and Guru Teg Bahadur (GTB) Hospital, Delhi, India, chandergroverkubba76@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhoi AK, Grover C, Singal A, Tandon A. Enthesopathy in patients with nail psoriasis – a cross-sectional evaluation of clinical, onychoscopic and ultrasonographic features. Indian J Dermatol Venereol Leprol 2023;89:854-61.
Abstract
Background
Nail involvement in psoriasis is common and may be an indicator not only of disease severity, but also of the presence of psoriatic arthritis. However, the relationship of nail psoriasis with enthesitis remains under-explored.
Aims
This study was conducted to evaluate the clinical, onychoscopic (nail dermatoscopic) and ultrasonographic features in patients with nail psoriasis.
Materials and Methods
All nails of twenty adult patients with nail psoriasis were examined clinically and onychoscopically. Patients were evaluated for psoriatic arthritis (Classification Criteria for Psoriatic Arthritis), the severity of cutaneous disease (Psoriasis Area Severity Index) and nail disease (Nail Psoriasis Severity Index). Ultrasonography of the clinically involved digits was performed for evidence of distal interphalangeal joint enthesitis.
Results
Out of 20 patients, 18 patients had cutaneous psoriasis and 2 had isolated nail involvement. Among the 18 patients with skin psoriasis, 4 had associated psoriatic arthritis. The most commonly observed clinical and onychoscopic features were pitting (31.2% and 42.2%), onycholysis (36% and 36.5%) and subungual hyperkeratosis (30.2% and 30.5%), respectively. Ultrasonographic evidence of distal interphalangeal joint enthesitis was seen in 57% (175/307) of the digits with clinical nail involvement. Enthesitis was more common in patients with psoriatic arthritis (77% vs 50.6%). Nail thickening, crumbling and onychorrhexis (all features of nail matrix involvement) were significantly associated with enthesitis (P < 0.005).
Limitation
The major limitation was the small sample size and lack of controls. Only the clinically involved digits were evaluated for enthesitis.
Conclusion
Enthesitis was frequently detected on ultrasonography in patients with nail psoriasis, even in clinically asymptomatic individuals. Nail features of thickening, crumbling and onychorrhexis may predict underlying enthesitis and the potential development of arthritis. A comprehensive evaluation could help identify patients with psoriasis at risk for arthritis, helping improve long-term outcomes.
Keywords
Enthesitis
nail psoriasis
psoriatic arthritis
nail dermoscopy.
Plain Language Summary
Ultrasonographic evaluation of distal interphalangeal joint involvement in nail psoriasis
Nail psoriasis is more frequent as well as more severe in patients with psoriatic arthritis. Through this study we explore its association with distal interphalangeal joint (DIP) enthesitis. Ultrasonographic evidence of DIP joint enthesitis was found to be commonly present in 307 digits of 20 patients, manifesting nail psoriasis. This was present even when the patient did not have any clinical evidence of psoriatic arthritis. We also found that nails with thickening, crumbling, or onychorrhexis had evidence of enthesitis more commonly. This study highlights that nail psoriasis should be comprehensively evaluated and treatment options chosen with a long-term aim to prevent joint damage.
Introduction
Isolated nail involvement may be seen in 5–10% of patients with psoriasis and the incidence of nail involvement has been estimated to be up to 90% over a lifetime.1,2 Nail psoriasis significantly affects the quality of life3–5 and correlates with increased disease severity, longer duration and higher frequency of joint involvement.
Clinical features of nail psoriasis are variable, determined by the site of involvement within the nail unit. The nail bed rests directly on the periosteum of the distal phalanx and the nail matrix lies in proximity to the distal interphalangeal joint and the insertion of the digital extensor tendon. This explains the frequent association of nail psoriasis with distal interphalangeal joint arthritis and enthesitis.
An early diagnosis of enthesitis and distal interphalangeal joint arthritis by radiological imaging (ultrasonography, magnetic resonance imaging) may permit choice of appropriate therapy, thus enabling optimal therapeutic outcomes, improving prognosis and preventing deformities. Ultrasonography is cheaper and more easily available than magnetic resonance imaging and is a sensitive, repeatable and real-time assessment.
The nature and characteristics of nail unit changes have not been comprehensively evaluated and data regarding the link between nail psoriasis and enthesitis of the corresponding digital extensor tendon is scant. To bridge this gap, we evaluated clinical and onychoscopic features of patients with nail psoriasis along with an ultrasonographic assessment of the DIP joints and entheses.
Materials and Methods
A convenience sample of 20 consecutive adult patients with nail psoriasis presenting to the Skin OPD of the Department of Dermatology and STD, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India, was recruited after approval by the Institutional Ethical Committee. The study protocol was explained and written informed consent obtained from each study participant.
A detailed history and complete mucocutaneous examination documenting the site(s) of cutaneous involvement and cutaneous disease severity (using the Psoriasis Area Severity Index) was performed. The nails of all fingers and toes were examined under good light, and the severity of nail involvement was recorded using the Nail Psoriasis Severity Index. Nail dermoscopy (onychoscopy) was performed with a USB dermatoscope (Dinolite edge Digital Microscope AM7515MZT, AnMo Electronics Corporation, Taipei, Taiwan) and the changes noted. A detailed musculoskeletal examination was conducted and the presence of psoriatic arthritis was documented using the Classification criteria for Psoriatic Arthritis (CASPAR).
Ultrasonographic assessment (Samsung RS80 EVO, Samsung Electronics Co. Ltd, Seoul, South Korea) of the distal interphalangeal joint and entheses was performed on all digits with clinically involved nails using a linear probe (frequency of 3–16 Hz). We used the OMERACT 7 (Outcome Measures in Rheumatoid Arthritis Clinical Trials) definitions for ultrasonographic pathology and a loss of normal fibrillary architecture of the digital extensor tendon, the presence of enthesophytes at the point of bony insertion or bony changes, including erosions, were documented as enthesitis.6
All data were recorded in MS Excel and statistical analysis was performed using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, N.Y., USA). Means and proportions were calculated. Appropriate statistical tests of significance including t-test (for means), Chi-square test and Fisher’s exact test (for proportions) were applied to evaluate statistical significance of differences between study groups.
Results
The ages of the study subjects ranged from 18–60 years (mean 38.1 ± 12.7 years). Men outnumbered women (1.85:1) and the duration of psoriasis ranged from 1 to 13 years (mean 5.9 ± 3.4 years) [Table 1]. Of the 20 patients with nail psoriasis, 4 had associated psoriatic arthritis, 2 patients had isolated nail involvement, while the rest had only cutaneous involvement. The Psoriasis Area Severity Index (PASI) of the 18 patients with cutaneous disease ranged from 1.6 to 50.8 (mean 12.2 ± 10.9).
| Nail psoriasis (n = 20) | Nail psoriasis without psoriatic arthritis (n = 16) | Nail psoriasis with psoriatic arthritis (n = 4) | |
|---|---|---|---|
| Gender Male:Female | 1.85:1 | 1.6:1 | 3:1 |
| Age (years) Mean ± standard deviation | 38.1 ± 12.65 | 38.18 ± 13.67 | 37.75 ± 7.25 |
| Disease duration (years) Mean ± standard deviation | 5.85 ± 3.39 | 5.4 ± 3.39 | 7.5 ± 2.87 |
| PASI Score (Mean ± standard deviation) | 12.22 ± 10.9 | 13.4 0 ±11.67 | 7.5 ± 4.57 |
|
Nail psoriasis severity index score Mean ± standard deviation |
52.1 ± 33.42 | 42 ± 24.62 | 92.5 ± 33.47 |
| Number of nails involved per patient | 15.35 ± 4.0 | 14.56 ± 4.03 | 18.5 ± 1.65 |
| Ultrasonography evaluation of distal interphalangeal joint | |||
| Total number of clinically involved nails (examined by ultrasonography) | 307 | 233 | 74 |
| Presence of radiological evidence of distal interphalangeal enthesopathy | 175 (57%) | 118 (50.64%) | 57 (77.02%) |
| Ultrasonography features seen | |||
| Enthesophyte formation | 143 (46.57%) | 103 (44.2%) | 40 (70.17%) |
| Bony erosion | 10 (3.25%) | 3 (1.28%) | 7 (9.45%) |
| Loss of normal fibrillary architecture | 22 (7.16%) | 12 (5.15%) | 10 (13.5%) |
Clinical nail involvement
All 400 nails of the 20 patients were examined and 307 of these were affected clinically. The mean number of nails involved in each patient was 15 (SD ± 4; range 9–20) and the mean Nail Psoriasis Severity Index (NAPSI) was 52.1 (SD ± 33.4; range 15–120). The mean Nail Psoriasis Severity Index was higher in patients with psoriatic arthritis in comparison with those without (92.5 vs 42). A weak correlation between nail psoriasis severity index and psoriasis area severity index was noted (Pearson’s correlation coefficient (r) = 0.208) but this was not statistically significant (P = 0.376). A total of 74/80 nails (92.5%) were involved in the 4 patients with psoriatic arthritis, while 118/320 nails (36.9%) were involved in psoriasis patients without arthritis.
The features of nail psoriasis on clinical examination are shown in Figure 1. Pitting was the commonest nail matrix change [Figure 2a] followed by thickening and crumbling [Figure 3a]. The most frequent nail bed changes were onycholysis, subungual hyperkeratosis and splinter haemorrhages, in that order [Figure 4a]. Pitting was most frequent finding in fingernails and distal onycholysis with subungual hyperkeratosis was the commonest change in toenails. A statistically significant difference was notable between the finger and toenails with respect to the incidence of some features such as pitting, thickening and crumbling, onychorrhexis, onycholysis and subungual hyperkeratosis [Table 2].

- Frequency distribution of nail psoriasis features on clinical examination and onychoscopy

- Clinical evidence of pitting in nail psoriasis seen as multiple, irregularly arranged pits

- Nail dermoscopy (onychoscopy) showing psoriatic nail pitting with pits that are irregular in distribution, size, shape and depth (black arrows). Few have associated scaling (red arrow) (Dinolite AM7515MZT nonpolarised ×35)

- Clinical finding of extensive psoriasis with thickened and crumbling nails with yellowish discolouration

- Onychoscopic image of thickened and crumbling nail plate. Yellow discolouration and opaque nail plate with the nail bed not visible (Dinolite AM7515MZT nonpolarised ×35)

- Clinical evidence of nail bed psoriasis seen as distal onycholysis, salmon patch and splinter haemorrhages seen involving multiple nails

- Onychoscopic image showing distal disruption of onychodermal band (onycholysis) (black arrows) with proximal erythema (red stars) and multiple splinter haemorrhages (blue arrowheads) (Dinolite AM7515MZT polarised ×60)
| Clinical examination | Onychoscopic examination | |||||
|---|---|---|---|---|---|---|
| Fingernails n (%) | Toenails n (%) | P value | Fingernails n (%) | Toenails n (%) | P-value | |
| Total nails examined | 200 | 200 | 200 | 200 | ||
| Nail matrix features | ||||||
| Pitting | 105 (53%) | 20 (10%) | 0.0001* | 127 (64%) | 42 (21%) | 0.00001* |
| Thickening and Crumbling | 40 (20%) | 65 (33%) | 0.004* | 40 (20%) | 64 (32%) | 0.465 |
| Leukonychia | 4 (2%) | 1 (0.5%) | 0.371 | 9 (5%) | 1 (0.5%) | 0.02* |
| Red spot in lunula | 0 | 0 | 0 | 0 | ||
| Longitudinal ridging | 8 (4%) | 2 (1%) | 0.105 | 18 (9%) | 6 (3%) | 0.011* |
| Beau’s line | 20 (10%) | 21 (11%) | 0.869 | 23 (12%) | 21 (11%) | 0.749 |
| Onychoschizia | 1 (0.5%) | 4 (2%) | 0.371 | 1 (0.5%) | 4 (2%) | 0.371 |
| Onychorrhexis | 2 (2%) | 14 (7%) | 0.003* | 3 (1.5%) | 20 (10%) | 0.0003* |
| Longitudinal Melanonychia | 3 (1.5%) | 2 (1%) | 1 | 3 (1.5%) | 2 (1%) | 1 |
| Nail bed features | ||||||
| Onycholysis | 54 (27%) | 90 (45%) | 0.001* | 53 (27%) | 93 (47%) | 0.288 |
| Oil spot | 7 (4%) | 0 | 0.014* | 6 (3%) | 0 | 0.03 |
| Subungual hyperkeratosis | 43 (22%) | 78 (39%) | 0.0001* | 43 (22%) | 79 (40%) | 0.00009* |
| Splinter haemorrhages | 8 (4%) | 1 (0.5%) | 0.037* | 27 (14%) | 5 (3%) | 0.0001 |
Onychoscopy (Nail Dermatoscopy)
Onychoscopic involvement alone (without clinical changes) was noted in 8 nails (i.e. a total of 315 nails were involved on onychoscopy) [Table 2; Figure 1]. Pitting, thickening and crumbling were the most common nail matrix features noted on onychoscopy [Figures 2b and 3b]. The most frequent nail bed changes were onycholysis, subungual hyperkeratosis and splinter haemorrhages, in that order [Figure 4b].
The difference in incidence of pitting, leukonychia, longitudinal ridging, onychorrhexis and subungual hyperkeratosis between finger and toenails was statistically significant (P < 0.05) [Table 2]. Pitting, longitudinal ridging and splinter haemorrhages were significantly more frequently seen on onychoscopy as compared with the clinical examination [Table 3].
| Clinical examination n = 200 (%) | Onychoscopic examination n = 200 (%) | P-value | |
|---|---|---|---|
| Total nails involved | 307 (76%) | 315 (78%) | 0.496 |
| Nail matrix features | |||
| Pitting | 125 (31%) | 169 (42%) | 0.001* |
| Thickening and crumbling | 105 (26%) | 104 (26%) | 0.9 |
| Leukonychia | 5 (1%) | 10 (3%) | 0.192 |
| Red spot in the lunula | 0 | 0 | |
| Longitudinal ridging | 10 (3%) | 24 (6%) | 0.014* |
| Beau’s line | 41 (10%) | 44 (11%) | 0.712 |
| Onychoschizia | 5 (1%) | 5 (1%) | 1 |
| Onychorrhexis | 16 (4%) | 23 (6%) | 0.25 |
| Longitudinal Melanonychia | 5 (1%) | 5 (1%) | 1 |
| Nail bed features | |||
| Onycholysis | 144 (36%) | 146 (37%) | 0.883 |
| Oil spot | 7 (2%) | 6 (2%) | 0.779 |
| Subungual HK | 121 (30%) | 122 (31%) | 0.938 |
| Splinter haemorrhage | 9 (2%) | 32 (8%) | 0.0002* |
| Variables | Nail features | Enthesitis | P-value | ||
|---|---|---|---|---|---|
| Present | Absent | Present | Absent | ||
| Pitting | n = 125 | n = 182 | n = 75 | n = 50 | 0.772 |
| Thickening and crumbling | n = 105 | n = 202 | n = 68 | n = 37 | 0.04* |
| Beau’s line | n = 41 | n = 266 | n =19 | n = 22 | 0.138 |
| Onychorrhexis | n = 16 | n = 291 | n = 3 | n = 13 | 0.002* |
| Onycholysis | n = 144 | n = 163 | n = 82 | n = 62 | 0.984 |
| Oil spot | n = 7 | n = 300 | n = 3 | n = 4 | 0.468 |
| Subungual Hyperkeratosis | n = 121 | n = 186 | n = 76 | n = 45 | 0.097 |
| Splinter haemorrhages | n = 9 | n = 298 | n = 6 | n = 3 | 0.736 |
Ultrasonography
All 20 patients had enthesitis on ultrasonography and 57% of the clinically affected digits (175/307) demonstrated changes [Figures 5 and 6 and Table 1]. Enthesitis was documented in 77% (57 of 74) of the clinically affected nails of the 4 patients with psoriatic arthritis, but in only 51% (118/233) in those without arthritis.

- Longitudinal scan of distal interphalangeal joint showing enthesophyte (yellow arrow)

- Longitudinal scan of distal interphalangeal joint showing bony erosion (white star)
Enthesophyte formation (143 digits, 46.6%] was the commonest ultrasonography feature seen, while loss of normal fibrillary architecture (22 digits, 7.2%) and bony erosions (10 digits, 3.3%) were less commonly observed. Thickening and crumbling of the nail plate and onychorrhexis were frequently associated with enthesitis (P value of <0.05) [Table 4].
Discussion
Nail involvement in psoriasis is a common and important indicator of psoriatic arthritis and enthesitis. Ideally, nail psoriasis should influence long-term treatment choices, but in clinical practice it is often overlooked during diagnosis and management.
The mean number of nails involved per patient (18.5 vs 14.6) and the mean nail psoriasis severity index (92.5 vs 42) was higher in patients with psoriatic arthritis in our study, similar to previous reports. 5,7,8 This positive correlation of the frequency and severity of nail disease with psoriatic arthritis emphasizes the importance of a comprehensive nail evaluation.
The commonest clinical nail feature was onycholysis, followed by pitting and subungual hyperkeratosis [Table 3]. These have been variably reported to be onycholysis and splinter haemorrhages,9 or pitting and onycholysis.10 The most common onychoscopic feature was pitting, followed by onycholysis and subungual hyperkeratosis. The difference in frequency distribution between fingernails and toenails was statistically significant for some nail features [Table 2]. In contrast, Chauhan et al. reported significant differences for all nail features except Beau’s line and onychomadesis.11 We found a statistically significant difference in the frequency of detection for pitting, splinter haemorrhages and longitudinal ridging on onychoscopic examination as compared to clinical examination [Table 3]. Thus, onychoscopy is a useful adjunct in the evaluation of nail changes that may not otherwise visible.
Ultrasonography facilitates real-time evaluation of every component of the nail unit as well as the distal interphalangeal joint [Figure 7]. Ultrasonography nail plate changes have been classified by Wortsman et al.12 into types I–IV, with type IV being the most severe [Figure 8]. These correlate well with psoriatic arthritis.13 Though we could not do a comprehensive analysis of the nail plate structure in our patients, we did evaluate the entheseal structure in detail.

- Longitudinal scan of normal distal interphalangeal joint showing digital extensor tendon attachment (white star)
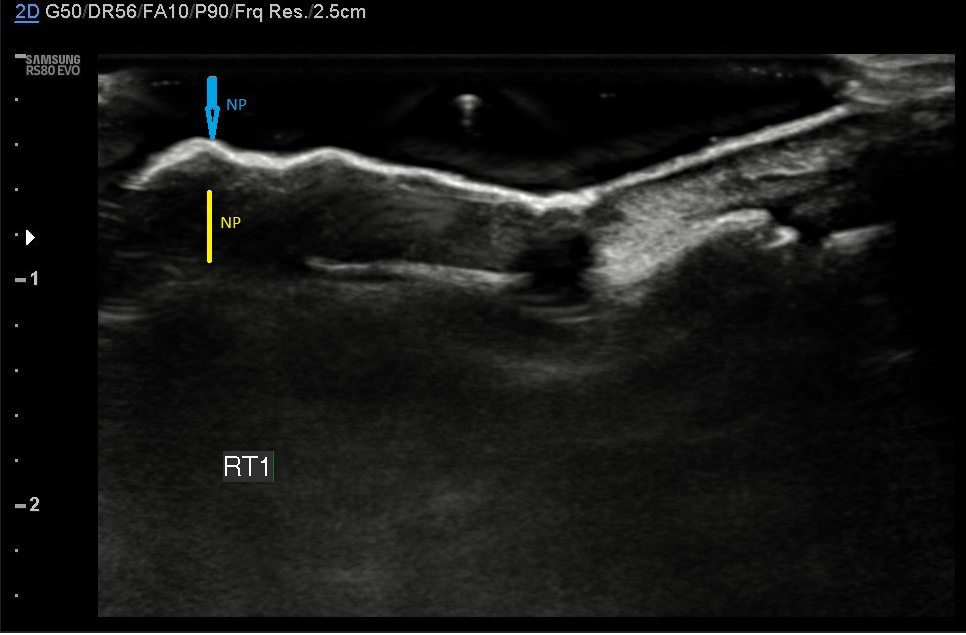
- Longitudinal scan of psoriatic nail showing thickened, irregular and wavy nail plate (NP, blue arrow) with loss of interplate hypoechoic zone and thickening of the nail bed (NB, Yellow arrow)
All our patients with nail psoriasis had evidence of enthesitis though most were asymptomatic. Ultrasonographic evidence of enthesitis was observed in 57% of involved digits. The higher frequency of distal interphalangeal joint enthesitis in patients with psoriatic arthritis was in concordance with previous data by Krajewska-Włodarczyk et al.14–16 [Table 5].
| Acosta-Felquer et al. 2017 | Krajewska-Włodarczyk et al. 2018 | Krajewska-Włodarczyk et al. 2019 | Present study | |||||
|---|---|---|---|---|---|---|---|---|
| Number of nails assessed | % of enthesitis on ultrasonography | Number of nails assessed | % of enthesitis on ultrasonography | Number of nails assessed | % of enthesitis on ultrasonography | Number of nails assessed | % of enthesitis on ultrasonography | |
| Number of nails with psoriasis | 236 | 60.6% | 416 | 46.3% | 440 | 49.5% | 307 | 57% |
| Number of nails with psoriasis without arthritis | 93 | 61.2% | 248 | 31% | 272 | 38% | 233 | 50.6% |
| Number of nails with psoriasis with psoriatic arthritis | 143 | 60.1% | 168 | 68% | 168 | 68% | 74 | 77% |
Thickening, crumbling and onychorrhexis of the nail were significantly associated with distal interphalangeal joint enthesitis. These three features are reflective of nail matrix disease and should alert the clinician towards the presence of enthesitis. However, other workers have noted that onycholysis to be frequently associated with enthesitis.17–19 Aydin et al.17 and Lai19 also noted pitting and crumbling, respectively in association with enthesitis.
Enthesitis is likely an early sign of arthritis and its persistence often precedes joint damage. Its frequency positively correlates with higher disease activity and poor quality of life.20 The association between nail psoriasis and adjacent enthesitis has been demonstrated by previous magnetic resonance imaging and ultrasonography studies.17,21 Entheseal inflammation is closely correlated with the inflammatory involvement of the nail matrix.22,23 This fact was reinforced in our study, with a high frequency of enthesitis in digits with involved nails, even in the absence of joint symptoms or signs.
Our findings outline a need for improving the sensitivity of diagnostic criteria for psoriatic arthritis. Patients with nail psoriasis do not have just distal interphalangeal joint enthesitis but also enthesitis involving other joints which may be in the form of higher than normal enthesitis scores for these distant joints. This suggests that enthesitis may be a systemic rather than a solely local entheseal response.24 An early diagnosis and treatment of enthesitis is critically important for ensuring a favourable outcome,25 and ultrasonography can thus serve as a non-invasive, relatively cheap and rapid technique for the assessment of entheseal changes.
Limitations
The major limitation of our study was the small sample size. No controls could be evaluated. Due to the small number of patients with concomitant psoriatic arthritis, we could not analyse conclusive differences. As we evaluated only the clinically involved digits, we cannot rule out the presence of subclinical enthesitis in uninvolved digits.
Conclusion
The frequency of enthesitis is very high in patients with nail psoriasis, even though clinical evidence may be lacking. The presence of nail changes like thickened and crumbling nails should alert dermatologists to plan treatment accordingly. A comprehensive clinical and onychoscopic evaluation can be a sensitive indicator in psoriasis patients at risk of psoriatic arthritis, even when the sensitivity of clinical criteria is low. Further studies with larger sample sizes involving different patient subsets can help comprehensively evaluate and validate these findings to help detect patients at risk early.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
NSI Thesis Research Grant 2019 (Grant no. 01/2019) provided as a partial research grant by the Nail Society of India.
Conflict of interest
There are no conflicts of interest.
References
- Nail psoriasis: The journey so far. Indian J Dermatol. 2014;59:319-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Psoriasis of the nail: Anatomy, pathology, clinical presentation, and a review of the literature on therapy. J Am Acad Dermatol. 2007;57:1-27.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis of the nails associated with disability in a large number of patients: results of a recent interview with 1,728 patients. Dermatol. 1996;193:300-3.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of nail psoriasis and treatment on quality of life: A systematic review. Skin Appendage Disord. 2021;7:83-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Nail psoriasis and quality-of-life measurement in clinical trials: Call for the use of nail-specific instruments. Am J Clin Dermatol. 2021;22:747-55.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Musculoskeletal ultrasound including definitions for ultrasonographic pathology. J Rheumatol. 2005;32:2485-7.
- [PubMed] [Google Scholar]
- Prevalence and clinical patterns of psoriatic arthritis in Indian patients with psoriasis. Indian J Dermatol Venereol Leprol. 2014;80:15-23.
- [CrossRef] [PubMed] [Google Scholar]
- Nail psoriasis, the unknown burden of disease. J Eur Acad Dermatol Venereol. 2014;28:1690-5.
- [CrossRef] [PubMed] [Google Scholar]
- Fingernail psoriasis reconsidered: A case-control study. J Am Acad Dermatol. 2013;69:245-52.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and serological characteristics of nail psoriasis in Indian patients: A cross-sectional study. Indian J Dermatol Venereol Leprol. 2017;83:650-5.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of nail psoriasis: An observational, analytical study. Skin Appendage Disord. 2020;6:207-15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of ultrasound in rheumatic skin and nail lesions: A multi-specialist approach. Clin Rheumatol. 2011;30:739-78.
- [CrossRef] [PubMed] [Google Scholar]
- Enthesitis: a hallmark of psoriatic arthritis. Semin Arthritis Rheum. 2018;48:35-43.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound assessment of changes in nails in psoriasis and psoriatic arthritis. Biomed Res Int. 2018;2018:8251097.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Distal interphalangeal joint extensor tendon enthesopathy in patients with nail psoriasis. Sci Rep. 2019;9:3628.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- High prevalence of ultrasonographic synovitis and enthesopathy in patients with psoriasis without psoriatic arthritis: A prospective case-control study. Rheumatology (Oxford). 2011;50:1838-48.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonographic assessment of nail in psoriatic disease shows a link between onychopathy and distal interphalangeal joint extensor tendon enthesopathy. Dermatol. 2012;225:231-5.
- [CrossRef] [PubMed] [Google Scholar]
- Nail involvement can predict enthesopathy in patients with psoriasis. J Dtsch Dermatol Ges. 2016;14:1102-7.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriatic nail involvement and its relationship with distal interphalangeal joint disease. Clin Rheumatol. 2016;35:2031-7.
- [CrossRef] [PubMed] [Google Scholar]
- Subclinical entheseal involvement in patients with psoriasis: an ultrasound study. Semin Arthritis Rheum. 2011;40:407-12.
- [CrossRef] [PubMed] [Google Scholar]
- A high-resolution magnetic resonance imaging study of distal interphalangeal joint arthropathy in psoriatic arthritis and osteoarthritis: are they the same? Arthritis Rheum. 2006;54:1328-33.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between the extensor tendon enthesis and the nail in distal interphalangeal joint disease in psoriatic arthritis—a high-resolution MRI and histological study. Rheumatology (Oxford). 2007;46:253-2.
- [CrossRef] [PubMed] [Google Scholar]
- Classification criteria for psoriatic arthritis: Development of new criteria from a large international study. Arthritis Rheum. 2006;54:2665-73.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis patients with nail disease have a greater magnitude of underlying systemic subclinical enthesopathy than those with normal nails. Ann Rheum Dis. 2012;71:553-56.
- [CrossRef] [PubMed] [Google Scholar]
- Improvements in diagnostic tools for early detection of psoriatic arthritis. Expert Rev Clin Immunol. 2016;12:1209-15.
- [CrossRef] [PubMed] [Google Scholar]







