Translate this page into:
Eruptive blue nevi
2 Pars Clinic, Rasht, Iran
Correspondence Address:
Omid Zargari
MD Pars Clinic, Somaye Blvd, Golsar, Rasht 41657
Iran
| How to cite this article: Kesty K, Zargari O. Eruptive blue nevi. Indian J Dermatol Venereol Leprol 2015;81:198-201 |
Sir,
A 56-year-old male was referred to our clinic for skin tag removal. During examination, multiple (more than 20) dark blue macules were noted on his balding scalp [Figure - 1] and [Figure - 2]. He denied any itching, ulceration, or other symptoms related to these macules. He had noticed the spots on his scalp, approximately 10 years prior to this visit. Notably, a few months before the patient noticed the blue macules, he was involved in a motor vehicle accident in which his head impacted the roof. There were no penetrating injuries or lacerations, however, at the time of the accident. In addition, the patient denied any history consistent with accidental tattooing of his scalp. The clinical features and histopathologic exam of a skin biopsy from the scalp were consistent with eruptive blue nevi [Figure - 3].
 |
| Figure 1: Multiple blue-gray macules on the scalp |
 |
| Figure 2: Close-up image of eruptive blue nevi |
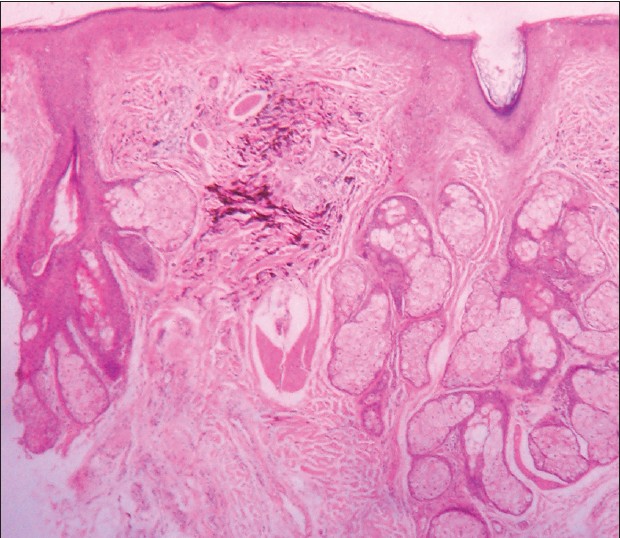 |
| Figure 3: Dermal collection of elongated melanocytes with abundant melanin pigment and intervening collagen bundles (hematoxylin and eosin, ×100) |
Blue nevi are melanocytic neoplasias of pigmented spindle and/or epithelioid melanocytes in the mid-dermis. [1] They appear as blue, blue-gray, or blue-black and are present in 0.5-4.0% of healthy white adults. [1] Most blue nevi are acquired; however, approximately 1 in 3000 newborns are born with congenital blue nevi. [1] The blue-gray color is due to the optical effect, named the Tyndall effect, of backscatter of blue light from the skin over dermal melanin. [1] Multiple blue nevi can present as part of the Carney complex/LAMB (lentigines, atrial myxomas, blue nevi) syndrome, along with lentigines, atrial myxomas, and mucocutaneous mastocytosis. [2] Evaluation for the above condition in patients with blue nevi is therefore warranted. However, our patient had no clinical features apart from blue nevi; therefore, further work-up was not done.
The differential diagnosis of blue nevi includes pigmented spindle cell nevus, traumatic tattoo, primary or metastatic melanoma, pyogenic granuloma, glomus tumor, sclerosing hemangioma, dermatofibroma, and ochronosis. [1] The differential diagnosis for other blue lesions includes Spitz nevi, seborrheic keratosis, hemangioma, Kaposi sarcoma, and dermatofibroma.
There are multiple types of blue nevi, including common blue nevus, cellular blue nevus, malignant blue nevus, large patch/plaque lesions, combined blue nevus, and atypical nevus. [2] Common blue nevi, as found in our patient, usually consist of a single lesion, less than 10 mm in diameter. The common blue nevi can appear anywhere, but approximately half of the reported cases are on the dorsa of the hands and feet. [1] Common blue nevi are also reported to occur in oral mucosa, uterine cervix, vagina, spermatic cord, prostate, and lymph nodes. [1],[3] The cellular blue nevus usually presents as nodules or plaques 1-3 + cm in diameter. They can have a smooth or irregular surface, and 50% of cases are found on the sacrum or buttocks [Table - 1]. [1] Malignant blue nevi are associated with cellular blue nevi, nevi of Ota, congenital blue nevi, or may arise without any underlying pathology. It has been suggested that malignant blue nevi are not a unique entity because they may be melanomas arising from a blue nevus. [1] Large patch/plaque blue nevi may be found in patients with a history of lentigo simplex. [1]
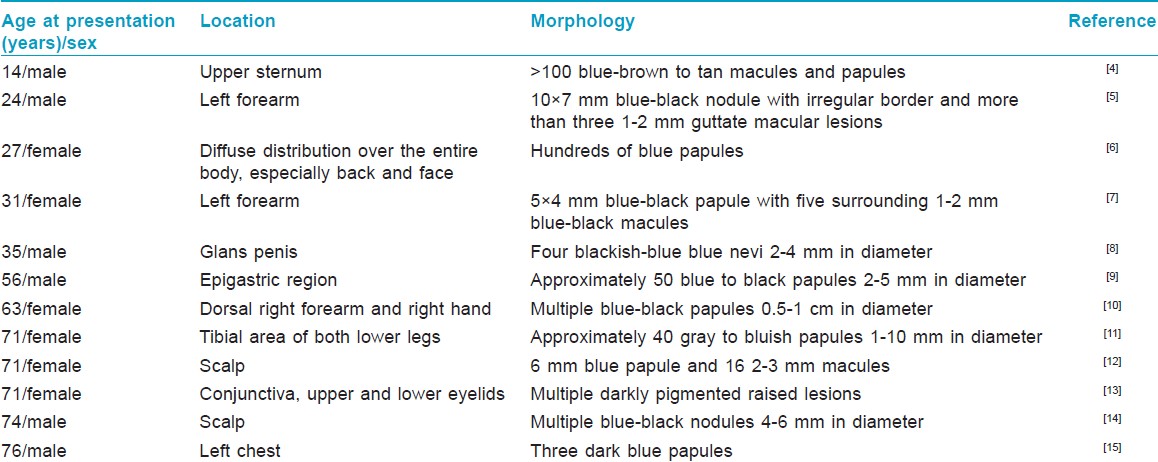
Once blue nevi appear, they typically remain stable and do not grow or change. Multiple cutaneous eruptive blue nevi are rare, with only 12 reports in the literature [Table - 1]. There is no report of any associated abnormality (except for an association with Carney complex) or increased risk of malignancy with eruptive blue nevi. [1],[16],[17]
The etiology of common blue nevi is unknown. [1] Interestingly, a specific somatic mutation in the heterotrimeric G protein alpha-subunit, GNAQ, has been reported to occur in blue nevi that turns GNAQ into a dominant oncogene resulting in melanocytic neoplasia. [2]
Most blue nevi are stable for many years and require no therapy. Change is worrisome for melanoma development and warrants biopsy and further workup. [17] Histopathologic examination of a blue nevus is warranted in the following instances: sudden appearance of a blue nodule, expansion of a previously stable blue nodule, and a nodule or plaque greater than 10 mm in diameter. [17] Excision of blue nevi should include subcutaneous fat to ensure removal of deep dermal melanocytes. [1]
Diagnosis of blue nevi can be made by clinical presentation, but histopathologic examination may be needed for confirmation in some cases. The dermatopathologic findings of common blue nevi include the following: dermal melanocytes appearing as melanin-containing fibroblast-like cells grouped in irregular bundles admixed with melanin-containing macrophages; groups of melanocytes with excess fibrous tissue in middle or upper reticular dermis, occasionally extending down to subcutaneous fat and up to papillary dermis; elongated melanin-producing dermal melanocytes lying with their long axis parallel to the epidermis; and normal appearing epidermis. [1]
We present this case of eruptive blue nevi on the scalp to highlight the rare location and the uncommonly high number of eruptive blue nevi in our patient.
ACKNOWLEDGEMENTS
We are grateful to Arash Taheri, MD, for his review of the manuscript and his insightful suggestions. We are also grateful to Dr. Mohamad Ashtiani for interpretation of the dermatopathology slides.
| 1. |
Grichnik JM, Rhodes AR, Sober AJ. Chapter 122. Benign Neoplasias and Hyperplasias of Melanocytes. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K. editors. Fitzpatrick's Dermatology in General Medicine. 8 th ed. New York: McGraw-Hill; 2012.
th ed. New York: McGraw-Hill; 2012.'>[Google Scholar]
|
| 2. |
Van Raamsdonk CD, Bezrookove V, Green G, Bauer J, Gaugler L, O'Brien JM, et al. Frequent somatic mutations of GNAQ in uveal melanoma and blue naevi. Nature 2009;457:599-602.
et al. Frequent somatic mutations of GNAQ in uveal melanoma and blue naevi. Nature 2009;457:599-602.'>[Google Scholar]
|
| 3. |
Patterson JW. Nevus cell aggregates in lymph nodes. Am J Clin Pathol 2004;121:13-5.
[Google Scholar]
|
| 4. |
Hendricks WM. Eruptive blue nevi. J Am Acad Dermatol 1981;4:50-3.
[Google Scholar]
|
| 5. |
Yonei N, Kimura A, Furukawa F. Common blue nevus with satellite lesions needs a differential diagnosis from malignant melanoma. Case Rep Dermatol 2013;5:244-7.
[Google Scholar]
|
| 6. |
Diehl JW, Berk DR, Ney A, Bayliss SJ. Diffuse dermal melanoytosis: Follow-up 30 years later with novel findings of eruptive blue nevi. Arch Dermatol 2011;147:1339-40.
[Google Scholar]
|
| 7. |
Chen T, Kurwa HA, Trotter MJ, Haber RM. Agminated blue nevi in a patient with dermatomyositis. J Am Acad Dermatol 2013;68:e52-3.
[Google Scholar]
|
| 8. |
deGiorgi V, Massi D, Brunasso G, Salvini C, Mastrolorenzo A, Zuccati G, et al. Eruptive multiple blue nevi of the penis: A clinical dermoscopic pathologic case study. J Cutan Pathol 2004;31:185-8.
[Google Scholar]
|
| 9. |
Shenfield HT, Maize JC. Multiple and agminated blue nevi. J Dermatol Surg Oncol 1980;6:725-8.
[Google Scholar]
|
| 10. |
Suchniak JM, Griego RD, Rudolph AH, Waidhofer W. Acquired multiple blue nevi on extremity. J Am Acad Dermatol 1995;33:1051-2.
[Google Scholar]
|
| 11. |
Krause MH, Bonnekoh B, Weisshaar E, Gollnick H. Coincidence of multiple, disseminated, tardive-eruptive blue nevi with cutis marmorata teleangiectatica congenital. Dermatology 2000;200:134-8.
[Google Scholar]
|
| 12. |
Knopp E, Diette K, Ko C, Lazova R. Multiple blue macules and papules on the scalp. Arch Dermatol 2009;145:1183-8.
[Google Scholar]
|
| 13. |
Blicker JA, Rootman J, White VA. Cellular blue nevus of the conjunctiva. Ophthalmology 1992;99:1714-7.
[Google Scholar]
|
| 14. |
Nardini P, De Giorgi V, Massi D, Carli P. Eruptive disseminated blue naevi of the scalp. Br J Dermatol 1999;140:178-80.
[Google Scholar]
|
| 15. |
Madan V, Gangodpadhyay M, Dawn G. A collection of blue papules. Clin Exp Derm 2009;34:121-2.
[Google Scholar]
|
| 16. |
Carney JA, Ferreiro JA. The epithelioid blue nevus: a multicentric familial tumor with important associations, including cardiac myxoma and psammomatous melanotic schwannoma. Am J Surg Pathol 1996;20:259-72.
[Google Scholar]
|
| 17. |
Granter SR, McKee PH, Calonje E, Mihm MC Jr. Busam K. Melanoma associated with blue nevus and melanoma mimicking cellular blue nevus: A clinicopathologic study of 10 cases on the spectrum of so-called 'malignant blue nevus'. Am J Surg Pathol 2001;25:316-23.
[Google Scholar]
|
Fulltext Views
8,649
PDF downloads
2,085





