Translate this page into:
Erythema-ab-igne: Dermatoscopic evaluation of six cases
Corresponding author: Dr. Keshavamurthy Vinay, Department of Dermatology, Venereology and Leprology, Post Graduate Institute of Medical Education and Research, Chandigarh, India. vinay.keshavmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta H, Gupta S, Vinay K. Erythema-ab-igne: Dermatoscopic evaluation of six cases. Indian J Dermatol Venereol Leprol. 2024;90:654-6. doi: 10.25259/IJDVL_68_2023
Dear Editor,
Erythema-ab-igne (EAI), or toasted skin syndrome, is a dermatosis resulting from low-level exposure to infrared heat. It presents as reticulated erythema and hyperpigmentation corresponding to dermal venous plexus. This results in a clinical picture characterized initially by transient macular erythema that easily blanches, progressing to fixed dusky hyperpigmentation. Dermatoscopic features of EAI need to be better characterized; knowledge of these features may aid in the differentiation of EAI from other reticulate dermatoses. We aim to provide new insights into the dermatoscopic features of EAI.
Six patients clinically diagnosed with EAI were included in the study. All patients were females with an average age of 36 years (range: 18–40 years) and had a history of using heating devices. Shins were involved in all six patients; two had lesions extending to the thighs and lower abdomen [Figure 1]. Dermatoscopic images were obtained using a DermLite DL4 dermatoscope attached to the camera of iPhone 12. Dermatoscopic features observed included accentuated pigment network (100%), epidermal scaling (83.3%), dilated eccrine openings (83.3%), polymorphous vessels (83.3%), red globules (33.3%), telangiectasias (33.3%) and white structureless areas (16.7%), over a background of erythema (100%) and homogenous brown pigmentation (100%) [Figures 2a–2d].

- Dusky hyperpigmentation over the back of the thighs in a net-like pattern
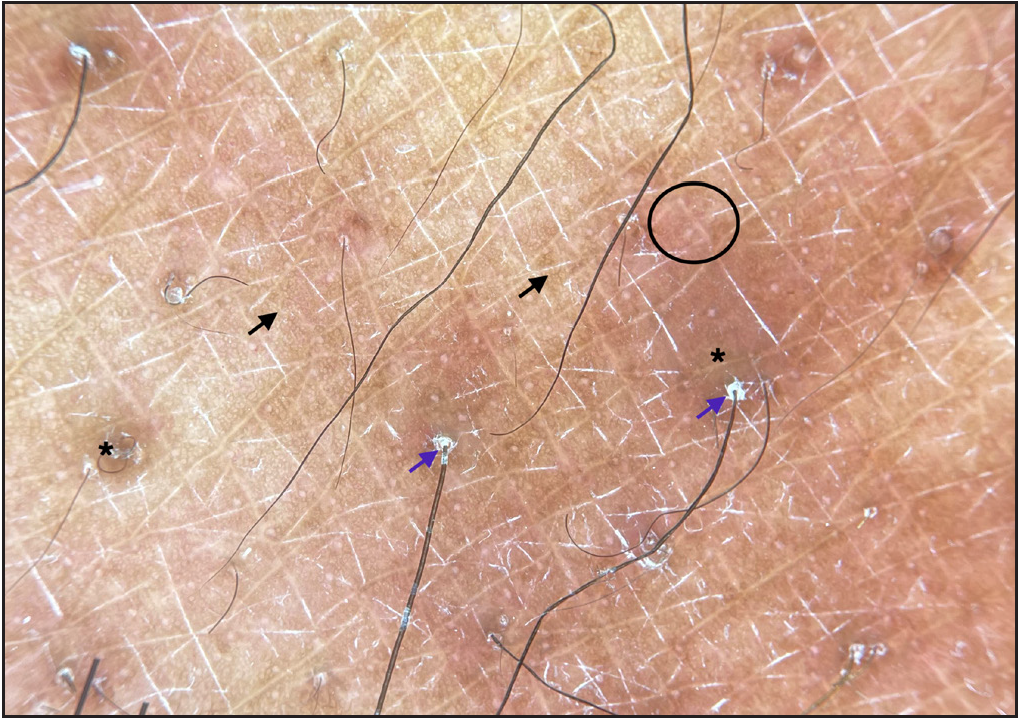
- Dermatoscopic evaluation of erythema-ab-igne: Accentuated pigment network (black arrows), follicular hyperkeratosis (blue arrows), polymorphous vessels (black circle) over a diffuse brown background (black asterisk) (DermLite DL4, 10x polarised).
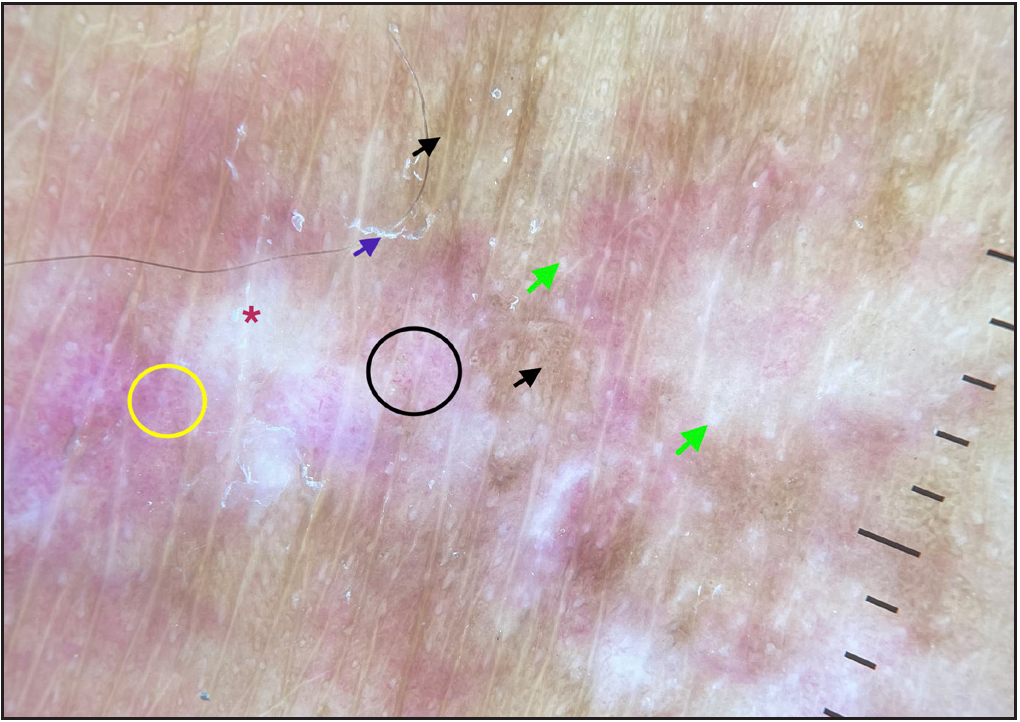
- Dermatoscopic evaluation of erythema-ab-igne: Accentuated pigment network (black arrows), epidermal scaling (blue arrows), tortuous vessels (black circle), dotted vessels (yellow circle), white structureless areas (red asterisk) and green arrows (dilated eccrine openings) (DermLite DL4, 10x polarised).
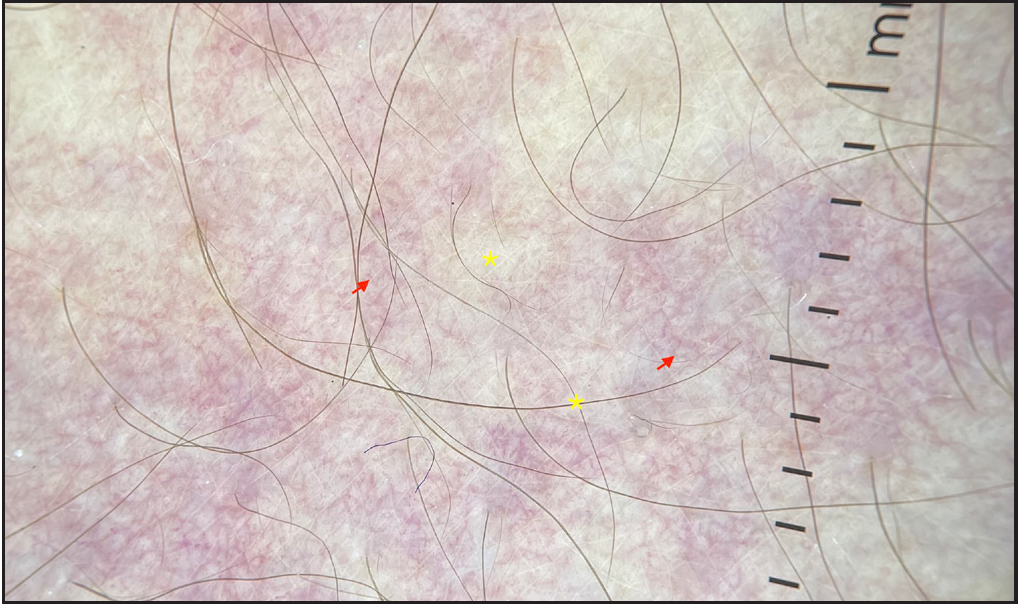
- Dermatoscopic evaluation of erythema-ab-igne: Telangiectasias (red arrows) over a white background (yellow asterisk) in a patient with extensive erythema ab igne (DermLite DL4, 10x polarised)
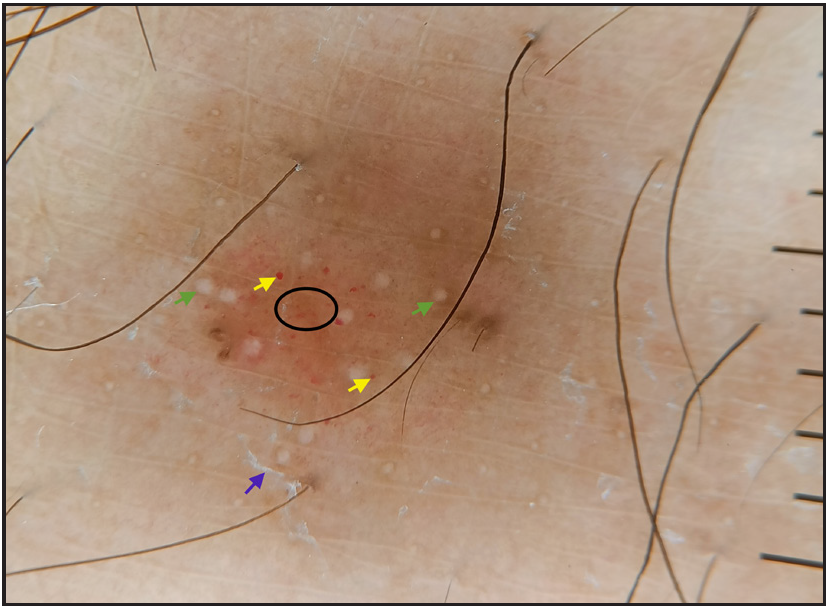
- Dermatoscopic evaluation of erythema-ab-igne: Epidermal scaling (blue arrows), green arrows (dilated eccrine openings), red globules (yellow arrows), dotted vessels (black circle) (DermLite DL4, 10 ×, polarised)
In line with the existing literature, most of our patients were females, and the lower limbs were the most common site of involvement. 1 EAI may result from exposure to heat sources such as electric stoves, laptops, and hot water bottles. All our patients reported EAI after exposure to room heaters, likely due to the lack of central heating in most Indian households.
The pathogenesis of EAI is not completely elucidated, and recurrent heat exposure has been postulated to damage blood vessels in the papillary dermis with consequent hemosiderin accumulation and hyperpigmentation.
1
Diagnosis is generally clinical, although histopathology may be required to rule out other differentials in rare cases. Previous case reports have described erythema, telangiectasias, polymorphous vessels, and diffuse brown hyperpigmentation as dermatoscopic features of EAI.
2–4
Apart from these previously reported findings, we observed accentuation of pigment network, dilated eccrine openings, and epidermal scaling in nearly all our patients. The main differentials of EAI include livedo reticularis, cutis marmorata, poikilodermatous mycosis fungoides, and adverse cutaneous drug reactions to amantadine. Dermatoscopy of poikilodermatous mycosis fungoides has been described as fine scales with linear branching vessels on a pink to the brown background.
5
Major limitation of our study was the lack of histopathological confirmation. We minimized this limitation by only including cases with unequivocal clinical diagnosis of EAI. Likely histopathological correlates of observed dermatoscopic findings are presented in Table 1.
Dermatoscopic feature
No. of patients (n = 6)
Histopathologic correlate
Lesional erythema
6 (100%)
Vasodilation
Accentuated pigment network
6 (100%)
Increased basal layer pigmentation
Homogenous brown pigmentation
6 (100%)
Dermal hemosiderin and melanin
Epidermal scaling and follicular hyperkeratosis
5 (83.3%)
Diffuse or focal hyperkeratosis
Dilated eccrine openings
5 (83.3%)
Dilatation of eccrine glands on heat exposure
Polymorphous vessels (linear vessels, dotted vessels, glomeruloid vessels, comma-shaped vessels)
5 (83.3%)
Dilation of postcapillary venules
Red globules
2 (33.3%)
Red blood cell extravasation
Telangiectasias
2 (33.3%)
Telangiectasias
White structureless areas
1 (16.7%)
Epidermal hyperkeratosis and dyskeratosis
Our study is an important case series describing the dermatoscopic features of EAI. EAI’s dermatoscopic hallmarks include homogeneous brown pigmentation, lesional erythema, and pigment network accentuation. We describe several new features, such as epidermal scaling, dilated eccrine openings, polymorphous vessels, and red globules. Knowledge regarding these parameters would aid the clinician in establishing the diagnosis of EAI and differentiating it from other disorders with similar clinical presentations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Clinical features and etiology of patients with erythema ab igne: A retrospective multicenter study. J Cosmet Dermatol. 2020;19:1774-9.
- [CrossRef] [PubMed] [Google Scholar]
- The use of dermatoscopy in the diagnosis of erythema ab igne. J Cosmet Dermatol. 2020;19:3444-5.
- [Google Scholar]
- A historical misleading case of erythema ab igne in a young Woman. Our Dermatology Online. 2019;9:454-5.
- [Google Scholar]
- Erythema Ab Igne induced by a laptop computer in an adolescent. An Bras Dermatol. 2011;86:128-30.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of poikilodermatous mycosis fungoides: A case escaping diagnosis for three decades. Photodermatol Photoimmunol Photomed. 2021;37:250-2.
- [CrossRef] [PubMed] [Google Scholar]





