Translate this page into:
Erythema elevatum diutinum associated with severe ocular complications and lung tuberculosis
Corresponding author: Prof. Yan Yu, Department of Dermatology, The First Hospital of Jilin University, Changchun, Jilin 130021, P.R. China. yu_yan@jlu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Si H, Li S, Wen Q, Yu Y. Erythema elevatum diutinum associated with severe ocular complications and lung tuberculosis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1291_2023
Dear Editor,
Erythema elevatum diutinum (EED) is a rare and chronic form of cutaneous leukocytoclastic vasculitis that has been related to multiple underlying diseases such as HIV infection, IgA paraproteinaemia, rheumatoid arthritis, and tuberculosis.1,2 In addition to cutaneous manifestations, EED can also present with rare ocular findings with peripheral ulcerative keratitis (PUK) being the most common.1 We describe a rare case of EED associated with bilateral pseudopterygium and pulmonary tuberculosis, which has not been reported previously.
A 64-year-old Chinese man presented with a 20-year-history of reddish/purplish patches and nodules on his limbs and ears. The lesions worsened five years ago, accompanied by vision blurring, redness, itching and wetness in his right eye. Similar symptoms appeared in the left eye two years ago, along with worsening skin lesions and sporadic episodes of coughing, expectoration, haemoptysis, and low-grade fever. Dermatological examination revealed multiple, discrete, symmetrical, firm, erythematous and purplish nodules and plaques on the face, ears, and limbs. In addition, atrophic scars occurred on both the ears and hands. Some lesions showed superficial erosions and scaling [Figures 1a-b]. The violaceous patch on the forearm and wrist of the patient were considered to be caused by increased capillary fragility and subcutaneous bleeding after minor trauma. Such localized changes were found on both wrists and forearms of the patient [Figure 1c]. Ocular examination revealed bilateral evidence of white linear scarring, conjunctival congestion, neovascularisation, and symblepharon. The bulbar conjunctiva of both eyes exhibited proliferation and invasion into the corneal limbus, covering the area of the pupil (5–7 mm). This part of the cornea appeared greyish-white with full-thickness turbidity [Figures 1d, 1e].

- Atrophic scars and a few scattered scaly nodules on the ear.

- Erythematous scaly plaques on the elbow.

- A purplish scaly plaque on the dorsum of the hand and atrophic scars on the fingers.
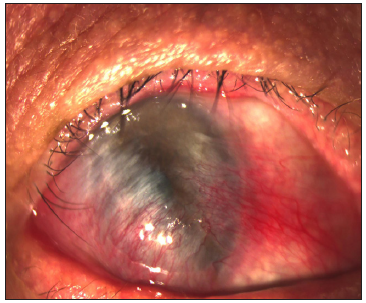
- Slit-lamp examination of the right eye.
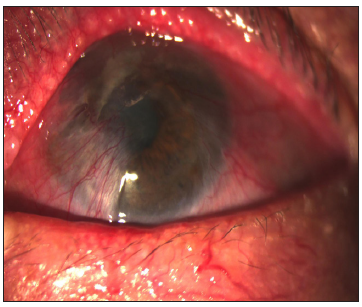
- Slit-lamp examination of the left eye.
Laboratory tests demonstrated an elevated serum IgA and serum lambda (LAM) light chain, and positive IgG antibodies against Mycobacterium tuberculosis; a computed tomography scan of the lungs revealed nodules in the posterior segment of the upper lobe tip and the dorsal segment of the lower lobe of both lungs, surrounded by the cord-like shadows and thick pleura, consistent with pulmonary tuberculosis [Figure 2]. For the pathological biopsies, we chose representative elbow lesions, and the pathological findings agreed with the EED modifications. Since we considered that all the plaques and nodules on the patient’s skin were caused by the same illnesses, a single tissue sample was used for the pathological biopsy [Figure 3].

- A computed tomography scan of the lungs revealing pulmonary tuberculosis (red arrow).
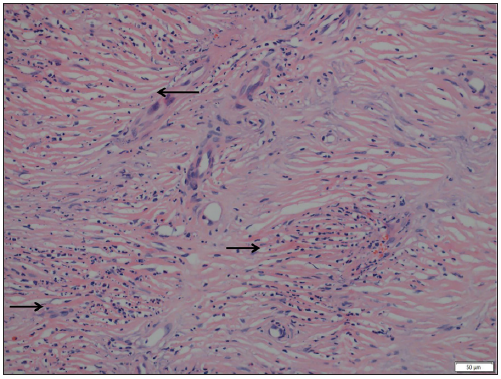
- Perivascular neutrophilic infiltration with karyorrhexis and concentric perivascular fibrosis (black arrows) (Haematoxylin and Eosin, 200x).
The patient was diagnosed with EED associated with bilateral pseudopterygium, corneal leukoma, and symblepharon, as well as pulmonary tuberculosis. Dapsone 100 mg daily, eye drops, and anti-tuberculosis medication were administrated, resulting in good improvement in 2 months. However, the patient subsequently failed to follow up and, tragically, passed away 1 year later due to multiple organ failure.
EED, a rare kind of chronic leukocytoclastic vasculitis, primarily affects individuals between the ages of 40 and 60 years with a similar incidence among men and women.1 A typical EED rash usually manifests as reddish/purplish, brown or yellow papules, nodules, and plaques that are symmetrically distributed on the extensor surface of the distal portion of the extremities and occasionally on the face, trunk, genitals, and buttocks.2 Histopathological changes of EED depend on the stage of the lesions; early lesions are characterised by neutrophilic infiltrate with eosinophils in the upper dermis to the mid-dermis and older lesions demonstrate dermal concentric perivascular fibrosis with mixed inflammation and lipid deposition.1,2
Although the exact pathogenesis of EED remains uncertain, it is thought to be correlated with the continuous deposition of the circulating immune complex in small vessels which results in complement fixation and subsequent inflammation. EED is related to a variety of systemic diseases, including certain infectious diseases.1,2,3 The association between EED and tuberculosis has been described in only a few cases in the English literature.3 The mechanism of EED associated with tuberculosis is hypothesised to involve the deposition of immune complexes, potentially formed by antibodies against M. tuberculosis proteins, in dermal vessel walls. This process may lead to leukocytoclastic vasculitis, contributing to the development of EED in these cases. In our patient, the onset of symptoms of tuberculosis coincided with the exacerbation of EED. This observation led us to speculate that tuberculosis might have been a contributing factor to the worsening of EED in this particular case.
We could find only 10 reported cases of EED with ocular involvement. The most common finding was PUK which was reported in nine cases. Other findings included Terrien marginal degeneration, scleritis, and inflammatory sclerokeratitis without thinning; only one patient was diagnosed with pseudopterygium, unlike our patient, who only had the left eye affected.1-6 Ocular inflammation occurred concurrently with the cutaneous lesions in all cases and the majority of the ocular and skin lesions improved simultaneously after treatment, indicating a potential association between the two. In our case, the initial failure to recognise the relationship between ocular abnormalities and EED led to a prolonged disease course. This highlights the critical importance of early and accurate diagnosis of eye involvement in patients with EED, as it is essential for providing the correct treatment and improving prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Progressive keratolysis with pseudopterygium associated with erythema elevatum diutinum. Ophthalmology. 2011;118:927-33.
- [CrossRef] [PubMed] [Google Scholar]
- A case of erythema elevatum diutinum associated with peripheral ulcerative keratitis. Indian J Dermatol Venereol Leprol. 2023;19:1-3.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum: A case report and review of literature. Int J Dermatol. 2019;58:408-15.
- [CrossRef] [PubMed] [Google Scholar]
- A case of erythema elevatum diutinum associated with peripheral ulcerative keratitis. Australas. J. Dermatol. 2012;53:78-80.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum associated with peripheral ulcerative keratitis. J Eur Acad Dermatol Venereol. 2011;25:741-2.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum associated with scleritis. Indian Dermatol Online J. 2011;2:28-30.
- [CrossRef] [PubMed] [Google Scholar]





