Translate this page into:
Erythema gyratum repens associated with cryptogenic organizing pneumonia
Correspondence Address:
Adam Reich
Department of Dermatology, Venereology and Allergology, Wroclaw Medical University, Chałubińskiego 1, 50 368 Wroclaw
Poland
| How to cite this article: Samotij D, Szczech J, Bencal-Kusinska M, Reich A. Erythema gyratum repens associated with cryptogenic organizing pneumonia. Indian J Dermatol Venereol Leprol 2016;82:212-213 |
Sir,
Erythema gyratum repens is a figurate erythema with a characteristic wood grain pattern and rapid peripheral spread. Here, we report a case of erythema gyratum repens occurring in a patient with cryptogenic organizing pneumonia.
A 54-year-old male was admitted due to peculiar figurate erythemas mainly located on the lower legs. The patient had an 18-month history of cryptogenic organizing pneumonia complicated by pulmonary hypertension. Cryptogenic organizing pneumonia was diagnosed based on chest X-ray, computed tomography (showing dispersed stromal fibrosis with bronchiectasis [Figure - 1] and mediastinal lymph node enlargement) and lung biopsy.
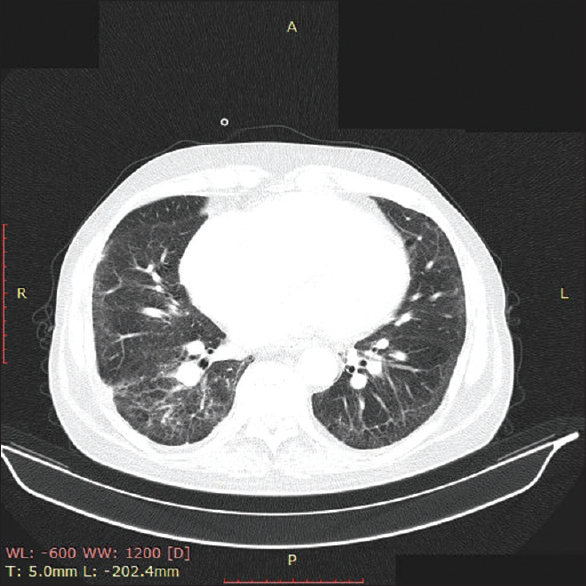 |
| Figure 1: Computed tomography of the chest showing dispersed stromal fibrosis of the lungs with bronchiectasis |
Seven months after onset of cryptogenic organizing pneumonia, the patient developed erythematous raised skin lesions initially misdiagnosed as urticarial wheals. He underwent treatment with antihistamines for 5 months without improvement. New skin lesions continued to develop on an intermittent basis, were painful and accompanied by fever, malaise and deterioration of respiratory function. The patient was admitted for investigations and management. At the time of admission, he had non-pruritic, pale red, slightly elevated, polycyclic and concentric mildly scaly plaques. The skin lesion resembled wood grains and showed rapid peripheral progression [Figure - 2]. Physical examination, abdominal and pelvic sonography and computed tomography, upper gastrointestinal endoscopy and colonoscopy revealed no abnormalities. On complete blood count, the patient had microcytic hypochromic iron deficiency anemia with hemoglobin of 9.9 g/dL, serum iron level 4.0 μmol/L; (normal range: 11.6-31.2 μmol/L). Bone marrow aspirate did not reveal any abnormalities. However, hypocomplementemia (low C3 and C4) and marked elevation of serum inflammatory biomarkers (C-reactive protein level: 150.4 mg/L, erythrocyte sedimentation rate: 54 mm/h, ferritin level: 920 μg/L, and alpha-1-acid glycoprotein: 2.99 mg/ml [normal range: 0.6-1.2]) was found. Liver function tests were within the normal limits except a moderately raised serum gamma glutamyl transpeptidase level of 131 U/L. Urine examination showed marked proteinuria (>0.5 g/dL) although no kidney biopsy was performed to evaluate the reason for proteinuria. Antinuclear antibodies and antineutrophil cytoplasmic antibodies were negative in the serum. Histological examination of a skin biopsy showed an atrophic epidermis with dermal perivascular mononuclear cell infiltration [Figure - 3]. The patient was continued on oral prednisone 20 mg/day for cryptogenic organizing pneumonia. As the patient′s clinical condition progressively deteriorated, he was re-investigated but no other underlying disease was found. The patient was then started on pulsed cyclophosphamide therapy (500 mg i.v. each month for 7 months) leading to marked improvement of respiratory function, proteinuria and a gradual improvement of skin changes which resolved within 6 months. The patient has been under observation for the last 3 years with no relapse or signs of any malignancy.
 |
| Figure 2: Concentric, polycyclic plaques of erythema gyratum repens |
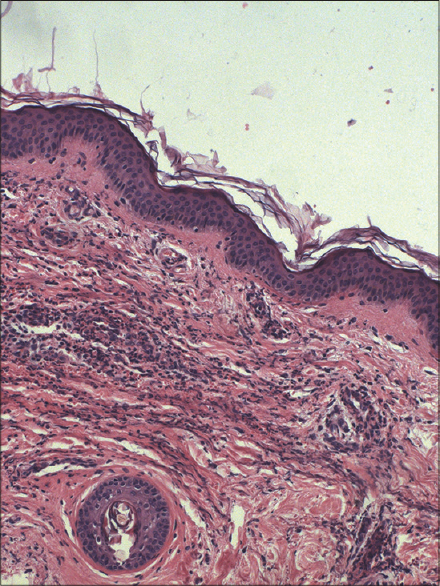 |
| Figure 3: Mild hyperkeratosis and mixed perivascular inflammatory infiltrate in the upper dermis (H and E original magnification, ×100) |
Since its first description erythema gyratum repens has been considered to be a paraneoplastic dermatosis. [1] However, in about 10-15% of patients it may accompany other diseases such as connective tissue diseases, infections and other conditions. Almost one-third of all non-paraneoplastic erythema gyratum repens cases have been considered idiopathic. [1],[2],[3]
Erythema gyratum repens is considered as an immunologically driven skin disease, however, its etiology still remains poorly understood. Currently, there are three suggested hypotheses regarding its pathogenesis: (1) cross-reacting tumor antigens which causes an inflammatory skin disorder, (2) transformation of normal skin proteins by tumor thus making them antigenic, (3) deposition of immune complexes with tumor antigens at the basement membrane zone and induction of inflammation. [4],[5] Despite a distinctive clinical morphology, skin lesions of erythema gyratum repens have non-specific histologic findings with acanthosis, mild hyperkeratosis, focal parakeratosis and epidermal spongiosis with superficial mononuclear, lymphohistiocytic perivascular inflammatory infiltrate in the dermis. [4],[5] Direct immunofluorescence of lesional skin may show IgG and C3 deposits along the basement membrane zone.
In our patient, we were unable to identify any of the conditions previously described to coexist with erythema gyratum repens. The exacerbation of skin lesions temporally correlated with periods of high activity of the lung disease. Based on this observation, we concluded that erythema gyratum repens in our patient was related to underlying cryptogenic organizing pneumonia; we were unable to find previous reports of this association.
Interestingly, the skin lesions in our patient were quite painful, a feature that is not usually reported in erythema gyratum repens.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rongioletti F, Fausti V, Parodi A. Erythema gyratum repens is not an obligate paraneoplastic disease: A systematic review of the literature and personal experience. J Eur Acad Dermatol Venereol 2014;28:112-5.
[Google Scholar]
|
| 2. |
Barber PV, Doyle L, Vickers DM, Hubbard H. Erythema gyratum repens with pulmonary tuberculosis. Br J Dermatol 1978;98:465-8.
[Google Scholar]
|
| 3. |
Endo Y, Fujisawa A, Tanioka M, Miyachi Y. Erythema gyratum repens preceding the onset of rheumatoid arthritis. Eur J Dermatol 2013;23:399-400.
[Google Scholar]
|
| 4. |
Eubanks LE, McBurney E, Reed R. Erythema gyratum repens. Am J Med Sci 2001;321:302-5.
[Google Scholar]
|
| 5. |
Stone SP, Buescher LS. Life-threatening paraneoplastic cutaneous syndromes. Clin Dermatol 2005;23:301-6.
[Google Scholar]
|
Fulltext Views
3,759
PDF downloads
1,918





