Translate this page into:
Erythematous edematous plaques in a 47-year-old woman with postmastectomy lymphedema
Corresponding author: Dr. Javier Sánchez Bernal, Department of Dermatology, Hospital San Jorge, Av. Martínez de Velasco, 36, 22004 Huesca, Spain. javisanchez_5@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sánchez-Bernal J, Álvarez-Salafranca M, Ramírez-Lluch M, Aldea-Manrique B. Erythematous edematous plaques in a 47-year-old woman with postmastectomy lymphedema. Indian J Dermatol Venereol Leprol 2023;89:141-3.
A 47-year-old woman presented with fever (38.6º C) and general discomfort for the past 48 h. She also noticed an eruption of painful cutaneous lesions in her right breast and arm at the same time.
This patient has a history of infiltrating ductal carcinoma of the right breast that had been surgically removed by radical mastectomy and right lymphadenectomy 21 months ago. As a surgical sequela, she developed right arm lymphedema. Afterward, she underwent chemotherapy and radiotherapy; with this combined treatment, she achieved a complete remission. Both therapies had ended 13 months ago. During all this time, there had not been any changes in her condition and she remained asymptomatic without any sign of progression.
Physical examination showed cutaneous lesions placed in her right half of the upper body (arm, shoulder and pectoral region). These were erythematous-edematous warm plaques associated with mild tenderness [Figure 1a]. Some skin areas were spared and there were some papules in her right forearm, similar to those lesions previously described but in a smaller size [Figure 1b].

- Erythematous indurated plaques with patched involvement of right pectoral, shoulder and upper arm affected by postmastectomy lymphedema

- Erythematous indurated plaque on the forearm
Laboratory tests revealed an increased c-reactive protein (15’74 mg/dL) and elevated white blood count of 13.300 per mm3 with an 80% of neutrophils. A cutaneous biopsy was performed, showing a neutrophilic dermal infiltrate with a mixed perivascular and interstitial distribution alongside papillary dermal edema without overt vasculitis in the dermis and subcutis [Figure 2]. The biopsy culture was negative.
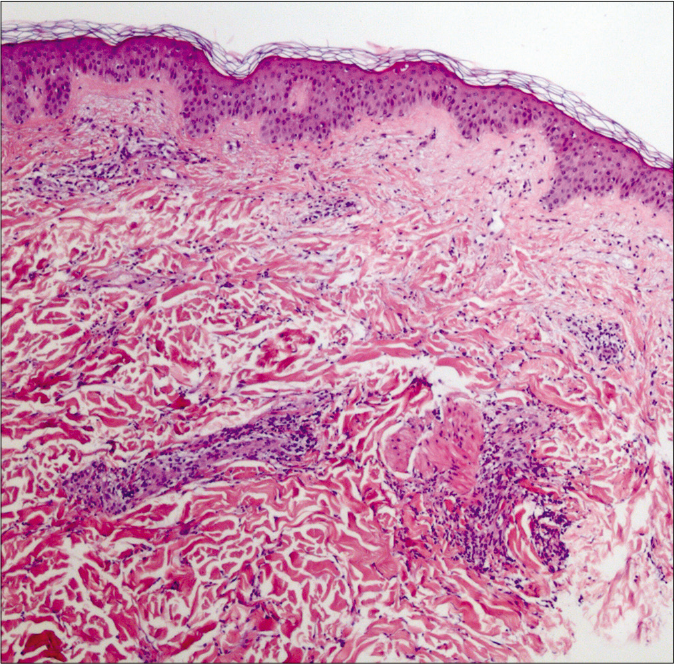
- Preserved epidermis with perivascular and interstitial neutrophilic infiltrate, accompanied by edema of the papillary dermis without vasculitis (H and E, ×400)
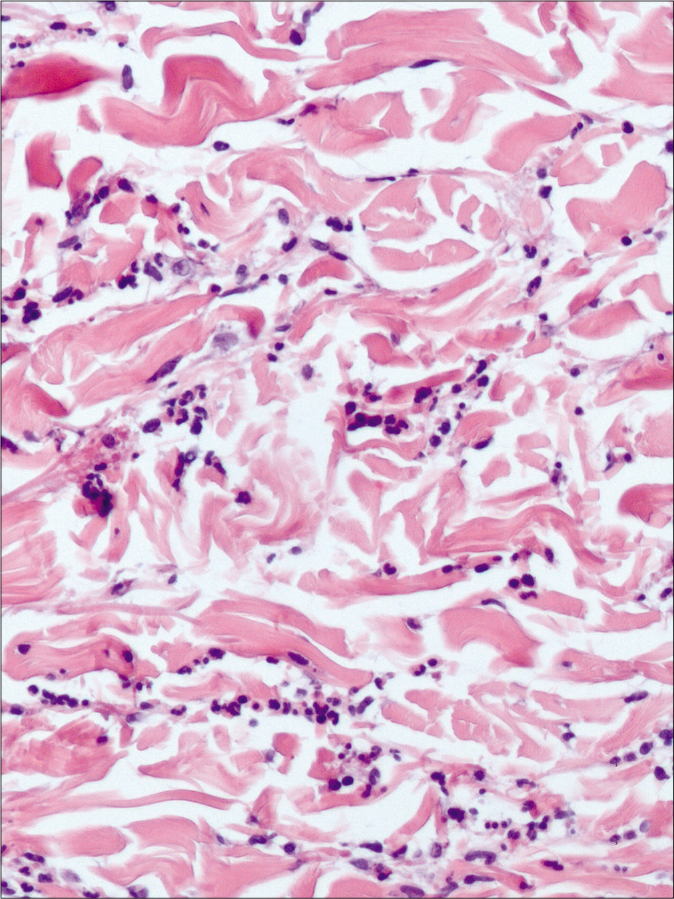
- Neutrophilic dermal infiltrate (H and E, ×200)
Question
What is your diagnosis?
Answer
Neutrophilic dermatosis on postmastectomy lymphedema
Discussion
Suspecting neutrophilic dermatosis, prednisone treatment with a dosage of 30 mg per day was initiated which achieved complete clearance of cutaneous lesions and resolution of systemic symptoms after 48 h [Figure 3]. After the patient was discharged, she continued to take oral prednisone in tapering doses for six days, starting with 30 mg daily with a reduction of 10 mg each 48 h. During the two-year follow-up, we have not recorded recurrent episodes.

- The skin lesions resolved completely after the treatment of systemic corticosteroids for 2 days
Lymphedema-associated neutrophilic dermatosis is considered as an atypical or localized presentation, different from the classical sweet syndrome.1,2 Compared with the classic sweet syndrome, this atypical variant differs from a milder clinical course, less systemic involvement and fewer recurrences.1
It is often found in women with a history of breast cancer that underwent lymphadenectomy.1,3 Nevertheless, there have been reported recently two clinical cases of patients with lower limb lymphedema.2 The time elapsed since surgery until the appearance of skin lesions is highly variable, from a few months to 14 years.1 There is no reported evidence of recurrent local relapse or distant metastasis from breast cancer after the resolution of the skin lesions.1,3,4
Clinically, it consists of multiple painful erythematous papules or plaques which may coalesce which predominantly develops on the lymphedematous area and can spread to the ipsilateral trunk.1,3,4 Systemic symptoms are usually mild or they even may be absent. Both extracutaneous manifestations and laboratory findings are often less remarkable comparing to the classical sweet syndrome.2,3
Histopathological findings are similar to those of classical sweet syndrome; an infiltrate primarily composed of neutrophils and localized mainly in the dermis. In some cases, the inflammatory infiltrate includes lymphocytes, histiocytes and eosinophils and there is marked edema in the papillary dermis.1,3
Regarding treatment, some publications are showing a good response to oral antibiotics and potassium iodide. However, systemic steroids remain as the first-line treatment for this entity, as well as in the classical sweet syndrome with the improvement of the symptoms and resolution of the cutaneous lesions shortly after initiation of therapy.1,2
Differential diagnosis is broad and it includes many different entities such as cellulitis, recall phenomenon, inflammatory breast carcinoma and herpes zoster.1,2,4 The patchy distribution of skin lesions, their extension beyond the irradiated area, the acute onset, as well as the absence of clustered vesicles, respectively, can aid in this differential diagnosis. Furthermore, a substantial improvement after systemic steroid therapy is a useful clue. Complementary tests such as Tzanck smear and laboratory and histopathological findings may also help along with the clinical presentation. The history of lymphedema should raise suspicion of this entity.
We consider that lymphedema-associated neutrophilic dermatosis is a poor-known complication and, therefore, it is most probably underdiagnosed, since this condition may mimic other infectious or inflammatory entities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Sweet’s syndrome on the area of postmastectomy lymphoedema. J Eur Acad Dermatol Venereol. 2006;20:401-5.
- [Google Scholar]
- Lymphedema-associated neutrophilic dermatosis: Two cases of localized Sweet syndrome on the lymphedematous lower limbs. J Dermatol. 2016;43:1062-6.
- [Google Scholar]
- Neutrophilic dermatosis on postmastectomy lymphedema. Actas Dermosifiliogr. 2012;103:649-51.
- [Google Scholar]
- Erythematous papules on the arm of a mastectomized patient. Actas Dermosifiliogr. 2009;100:231-2.
- [Google Scholar]





