Translate this page into:
Erythroderma: a study of incidence and aetiopathogenesis
Correspondence Address:
Ajay Chaudhary
5/A Sham Dham, Sion, Bombay-400022
India
| How to cite this article: Chaudhary A, Gupte PD. Erythroderma: a study of incidence and aetiopathogenesis. Indian J Dermatol Venereol Leprol 1997;63:38-39 |
Abstract
Thirty cases of exfoliative dermatitis (22 male and 8 female) were selected at random for study. In addition to routine history and clinical examination, investigations like histopathology of skin and lymph nodes, peripheral blood smear for abnormal cells and bone marrow examinations were done. Aetiologically, the cases could be classified into 4 categories namely exfoliation in per existing dermatoses, drug-induced exfoliation, idiopathic exfoliation and exfoliation secondary to internal malignancy. Two cases showed abnormal monocytoid cells (sezary cells) in peripheral blood smear.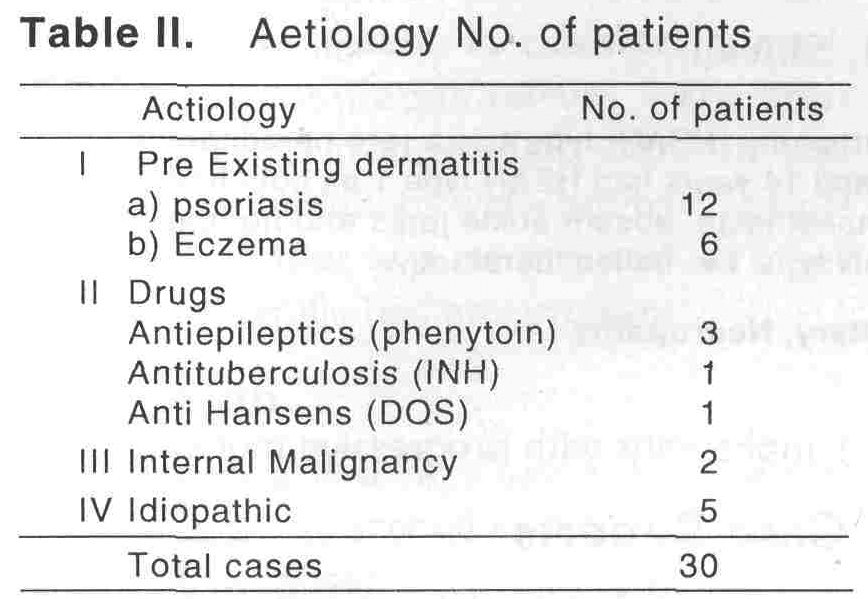
Introduction
Exfoliative dermatitis is a symptom complex characterized by generalised or universal exfoliation of the skin in response to various factors, internal or external, known or unknown. It either represents reflection on the skin of severe systemic disease or extension of pre existing cutaneous disease. The term erythroderma is applied when erythema is a conspicuous clinical feature, but distinction from exfoliative dermatitis is arbitary and these two terms are regarded as synonyms. Some of the recognized aetiological factors are exacerbation of an existing dermatoses, drugs and reticulosis. Incidence of exfoliative dermatitis in this country appears to be on the increase, but very little work has been done particularly with regard to aetiology of the disease. Hence, most of the cases of exfoliative dermatitis which are labeled as idiopathic, may at a later stage manifest certain reticulosis. The present study was undertaken to find out the causes which lead to this disorder.
Material and Methods
Thirty patients (22 male and 8 female) with erythroderma were taken up for the study. All the patinets were hospitalized. A detailed history was taken and following investigations were performed Complete haemogram, serum proteins, total and differential, liver and renal function tests, routine and microscopic urine tests, peripheral blood smear for abnormal cells, X-ray chest, skin and lymph node biopsies. Bonemarrow examination by sternal puncture was done in 2 cases.
Results
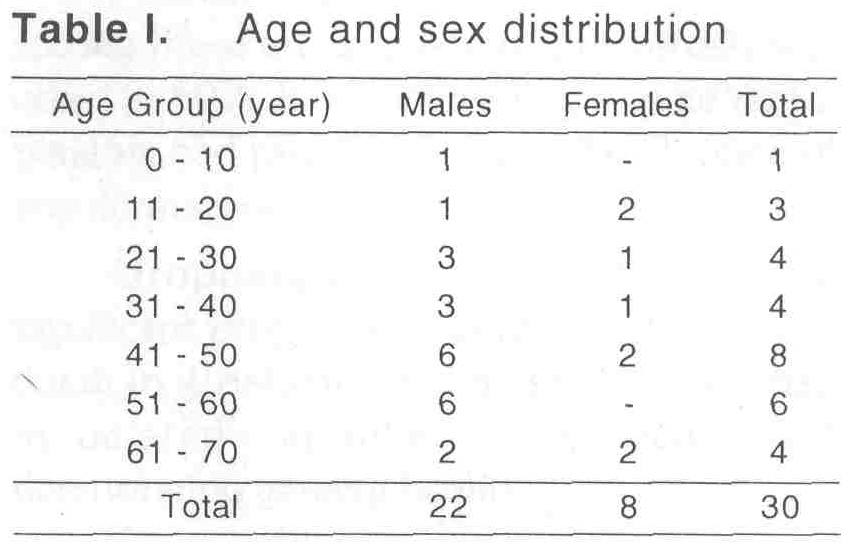
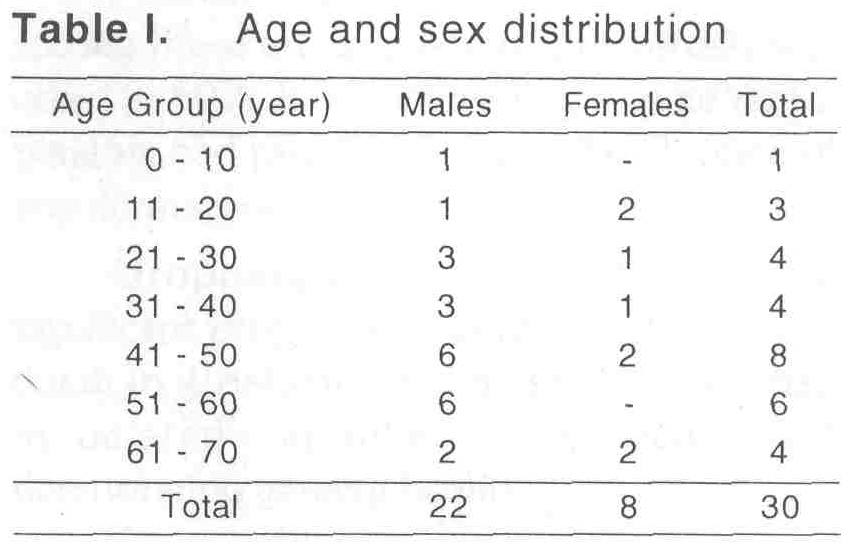
The disease was observed maximally in the 5th decade followed by 6th decade of life. Mean age of incidence is 51.5 years. [Table - 1] Incidence of exfoliative dermatitis was more in males than females.
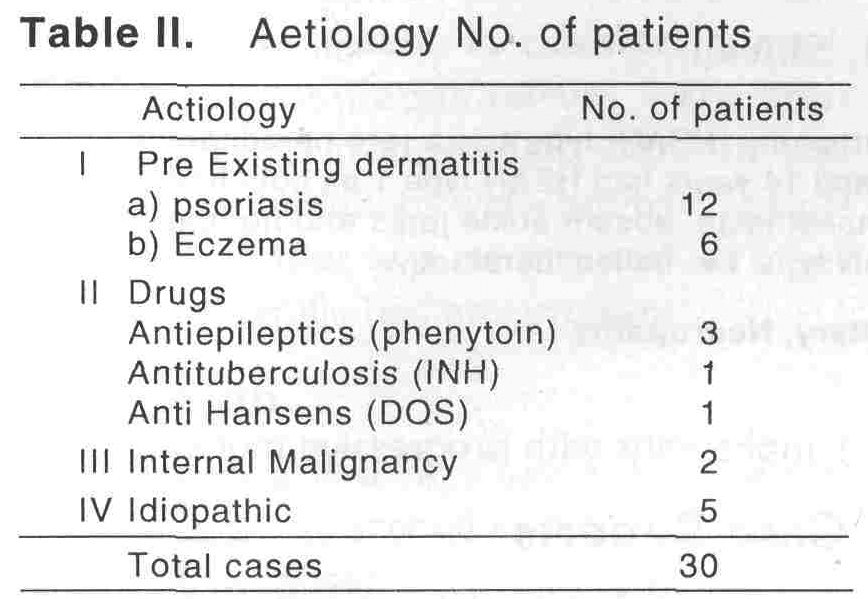
In the present series, the cases could be classified according to the causative factors as shown in [Table - 2].
Nail changes like pitting, subungual hyperkeratosis were noted in most of the cases of Psoriatic Erythroderma. Psoriatic Erythroderma (40%) accounted for the bulk of exfoliative dermatitis. None of the 12 cases of psoriatic erythroderma had a known precipitating factor. The exfoliative dermatitis secondary to eczema was seen in 6 cases (20%). Ingestion of drugs was responsible for exfoliative dermatitis in 5 patients (16.6%). Malignancy (mycosis fungoides) as a cause of exfoliative dermatitis was found in 2 (6.6%) of our patients.
Oedema of varying severity was seen in 25 cases (83.3%). Hypoalbuminemai, anaemia and inflammation of the skin accounted for oedema. Enlargement of superficial lymph nodes was observed in 19 cases. The involvement was maximum in the inguinal group of glands. Laboratory investigations revealed no significant abnormality excepting in 2 cases in which the peripheral blood revealed presence of a typical lymphocytes (Sezary cells). Histopathology of the skin was helpful in the diagnosis of 25 patients. In 12 patients with psoriatic erythroderma, histopathology was consisten with psoriasis. Six patients of erythroderma showed features consistnet with that of an eczema, while drug-induced erythroderma showed psoriasiform presentation. Presence of Pautrier′s microabscesses in 2 cases implied that the occurrence of exfoliative dermatitis was secondary to mycosis fungoides. Lymph node biopsy in 10 cases was consistent with a diagnosis of dermatopathic lymphadenitis.
Discussion
In detemining the aetiology of the present series of cases of exfoliative dermatitis, history and the physical examination were of great help. Histopathology of skin was of maximum benefit in cases suspected to be related to pre existing dermatosis and internal malignancy. In our series, Commonest cause of exfoliative dermatitis was psoriasis, while internal malignancy constituted the least common cause Similar findings have been reported in other studies[4].
| 1. |
Abraham I, McGarthy IT, Saunders IL. One hundred and one cases of exfoliative dermatitis. Arch Dermatol 1963.87:96-101.
[Google Scholar]
|
| 2. |
Wilson HTH. Exfoliative dermatitis:its etiology and prognosis. Arch Dermatol. Syphilol. 1954,69:577-588.
[Google Scholar]
|
| 3. |
Sehgal VN, Rege VL. A retrospective study of exfoliative dermatitis. Ind J Dermatol Venerol 1974,40:36.
[Google Scholar]
|
| 4. |
Singh R, Garg BR. A clinical study of exfoliative dermatitis. Ind J Dermatol 1970,16:11
[Google Scholar]
|





