Translate this page into:
Erythroderma secondary to lichen planus in a child
2 Department of Dermatology, Venereology and Leprology, Dr. Ram Manohar Lohia Hospital, Post Graduate Institute of Medical Education and Research, New Delhi, India
3 Department of Dermatology, Venereology and Leprology, Maulana Azad Medical College, Lok Nayak Hospital, New Delhi, India
Correspondence Address:
Surabhi Sinha
C - 403, Sabka Ghar, C.G.H.S., Plot No. 23, Sector 6, Dwarka, New Delhi - 110 075
India
| How to cite this article: Gupta C, Sinha S, Sahoo B, Garg VK. Erythroderma secondary to lichen planus in a child. Indian J Dermatol Venereol Leprol 2016;82:89-91 |
Sir,
A 12-year-old boy presented with generalized redness and scaling of the skin for 3 months and white patches on the tongue for 1 month. The eruption began as multiple, itchy, reddish, small papules over both legs which soon progressed to generalized involvement associated with fine scaling. There was no history of prior drug intake, fever, joint pains, photosensitivity, weight loss, anorexia or tuberculosis prior to the onset of the disease and the child was not atopic. Examination revealed generalized dusky blanchable erythema of the skin associated with grayish-white, fine semiadherent scales with some crusted erosions over the lower limbs [Figure - 1]a. Thickening of the palms and soles was present and nails were normal. The oral cavity showed white ill-defined plaques over the tongue and hard palate along with a few ulcers [Figure - 1]b. Laboratory investigation revealed a raised absolute eosinophil count. Fine needle aspiration cytology from an enlarged inguinal lymph node revealed reactive lymphadenitis and potassium hydroxide scraping from the mouth for oral candidiasis was positive. A wedge skin biopsy from the back revealed hyperkeratosis, parakeratosis, hypogranulosis and irregular acanthosis with moderate lymphoplasmacytic infiltrate in the superficial dermis [Figure - 1]c. Serial biopsies done during the erythrodermic phase showed similar changes. Based on the clinico-pathological features, a provisional diagnosis of erythroderma secondary to psoriasis vulgaris with oral candidiasis was made. The boy was treated with methotrexate 7.5 mg weekly for 8 weeks and oral fluconazole. The skin lesions improved significantly (Psoriasis Area and Severity Index score declined from 46.2 to 6.4) but the oral lesions did not improve despite repeated courses of fluconazole.
 |
| Figure 1: (a) Diffuse erythema associated with grayish-white semi-adherent scales with dark brown crusted erosions on lower limbs, (b) multiple discrete to coalescent erosions over tongue and hard palate surrounded by whitish plaques, (c) hyperkeratosis, parakeratosis, hypogranulosis and irregular acanthosis along with lymphoplasmacytic infi ltrate in upper dermis (H and E, ×100) |
Interestingly, as the child began to improve, a few violaceus flat-topped papules were noticed on the volar aspect of wrists [Figure - 2]a, followed by similar lesions over lower limbs and on lips [Figure - 2]b. By this time, a lacy pattern was also noticed over the buccal mucosa with a few erosions over the hard palate. Skin biopsy from a papule showed compact orthokeratosis, wedge-shaped hypergranulosis, irregular acanthosis, vacuolar degeneration of basal layer, colloid bodies in the basal layer and upper dermis and a band-like dermal lymphohistocytic infiltrate consistent with lichen planus [Figure - 2]c. Subsequently, the shaft of penis also developed violaceous papules [Figure - 2]d. Oral mucosal biopsy showed acute on chronic ulceration with granulation tissue and fibrosis underneath. Non-ulcerated areas showed focal saw-toothing and lympho-plasmacytic infiltrate. The diagnosis was then revised to erythroderma secondary to lichen planus. As oral lesions were not responding to methotrexate, he was administered oral prednisolone, 1 mg/kg and topical triamcinolone paste. Oral steroids were tapered gradually according to the clinical response and dapsone, 50 mg was added as maintenance therapy while topical steroid application was continued for oral lesions along with intermittent courses of fluconazole. The child improved markedly with resolution of skin lesions and oral complaints over the next 3 months.
 |
| Figure 2: (a) Multiple discrete fl at topped violaceous papules over volar aspect of both wrists, (b) similar lesions over both lower limbs, (c) compact orthokeratosis, wedge-shaped hypergranulosis, irregular acanthosis, vacuolar degeneration of basal layer, colloid bodies in basal layer and upper dermis and band-like dermal lymphohistocytic infi ltrate (H and E, ×100), (d) violaceous papules over genitalia |
Erythroderma is a reaction pattern characterized by generalized erythema with desquamation affecting more than 90% of the body surface. It is relatively uncommon in children compared to adults. Common causes of erythroderma in childhood are drug reactions (29%), genodermatoses, psoriasis and staphylococcal scalded skin syndrome (18% each), atopic dermatitis (12%) and seborrheic dermatitis (5%).[1]
Lichen planus is rare in childhood with less than 2–3% of all cases being seen in patients under 20 years of age.[2],[3] As in adults, both genders are equally affected. Mucosal lichen planus in children is uncommon being reported in 13.8-30% of childhood lichen planus.[4],[5],[6]
The clinical features of erythroderma are often non-specific and the approach to patients depends on a careful history. The diagnosis is more difficult in a patient without a prior history of dermatologic diseases who denies having recently taken any medication, as in our case. In such cases, it is important to perform a skin biopsy. Clinicopathological correlation in erythroderma is usually poor because often the specific cutaneous changes of a dermatosis or a drug reaction are obscured by the non-specific changes induced by erythroderma. Frequently, the histological features are those of chronic dermatitis or psoriasiform dermatitis.
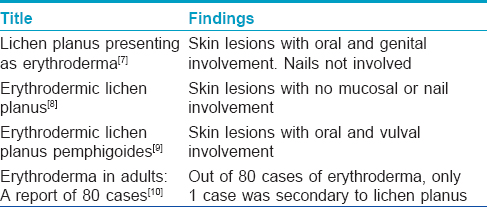
We could find only 4 prior case reports of erythroderma secondary to lichen planus and all were in adult patients [Table - 1].
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sehgal VN, Srivastava G. Erythroderma/generalized exfoliative dermatitis in pediatric practice: An overview. Int J Dermatol 2006;45:831-9.
[Google Scholar]
|
| 2. |
Boyd AS, Neldner KH. Lichen planus. J Am Acad Dermatol 1991;25:593-619.
[Google Scholar]
|
| 3. |
Hurwitz S, editor. Papulosquamous and related disorders in clinical paediatric dermatology. In: A Textbook of Skin Disorders of Childhood and Adolescence. 2nd ed. Philadelphia: WB Saunders; 1981. p. 83-105.
[Google Scholar]
|
| 4. |
Kanwar AJ, Handa S, Ghosh S, Kaur S. Lichen planus in childhood: A report of 17 patients. Pediatr Dermatol 1991;8:288-91.
[Google Scholar]
|
| 5. |
Sharma R, Maheshwari V. Childhood lichen planus: A report of fifty cases. Pediatr Dermatol 1999;16:345-8.
[Google Scholar]
|
| 6. |
Handa S, Sahoo B. Childhood lichen planus: A study of 87 cases. Int J Dermatol 2002;41:423-7.
[Google Scholar]
|
| 7. |
Gupta LK, Garg A, Khare AK, Mittal A. Lichen planus presenting as erythroderma. Indian J Dermatol Venereol Leprol 2012;78:409.
[Google Scholar]
|
| 8. |
Rose AE, Patel U, Chu J, Patel R, Meehan S, Latkowski JA. Erythrodermic lichen planus. Dermatol Online J 2011;17:26.
[Google Scholar]
|
| 9. |
Campos-Domínguez M, Silvente C, de la Cueva P, González-Carrascosa M, Lecona M, Suárez R, et al. Erythrodermic lichen planus pemphigoides. Actas Dermosifiliogr 2006;97:583-6.
[Google Scholar]
|
| 10. |
Rym BM, Mourad M, Bechir Z, Dalenda E, Faika C, Iadh AM, et al. Erythroderma in adults: A report of 80 cases. Int J Dermatol 2005;44:731-5.
[Google Scholar]
|
Fulltext Views
3,624
PDF downloads
2,964





