Translate this page into:
Erythrodermic pityriasis rubra pilaris: Dramatic response to infliximab therapy
2 Department of Pathology, Istanbul Medeniyet University, Goztepe Research and Training Hospital, Istanbul, Turkey
Correspondence Address:
Ayse Serap Karadag
Istanbul Medeniyet University, Goztepe Research and Training Hospital, Dermatology Istanbul
Turkey
| How to cite this article: Karadag AS, Kavala M, Ozlu E, Ozkanlı S, Zindancı &, Turkoglu Z. Erythrodermic pityriasis rubra pilaris: Dramatic response to infliximab therapy. Indian J Dermatol Venereol Leprol 2016;82:112 |
Sir,
Pityriasis rubra pilaris is a chronic papulo-squamous skin disorder characterized by skin and nail involvement.[1] The exact etiology is unknown. Vitamin A deficiency, infections, trauma and impaired immune responses are among the suggested causes.[2] A variety of topical and systemic treatment options are available.[3] This case is reported due to a dramatic response obtained with infliximab therapy, when various other systemic medications failed to produce a therapeutic response.
A 31-year-old woman presented to our clinic with a 4-year history of erythematous plaques over the upper half of her body which was spreading to the extremities. Dermatological examination revealed pink to red follicular papules which coalesced to form plaques. These were located over the face, neck, trunk, upper and lower extremities with patches of normal skin in between [Figure - 1]. There was no history of similar complaints in her family. Laboratory tests including complete hemogram, urinalysis, liver and kidney function tests, C-reactive protein, anti-HCV, anti-HIV, anti-HBsAg, and Mantoux test were within normal limits. Histopathological examination of the skin biopsy revealed hyperkeratosis, irregular acanthosis, broad rete ridges and thick suprapapillary plates. There was a superficial perivascular lymphocytic infiltrate in the dermis [Figure - 2].
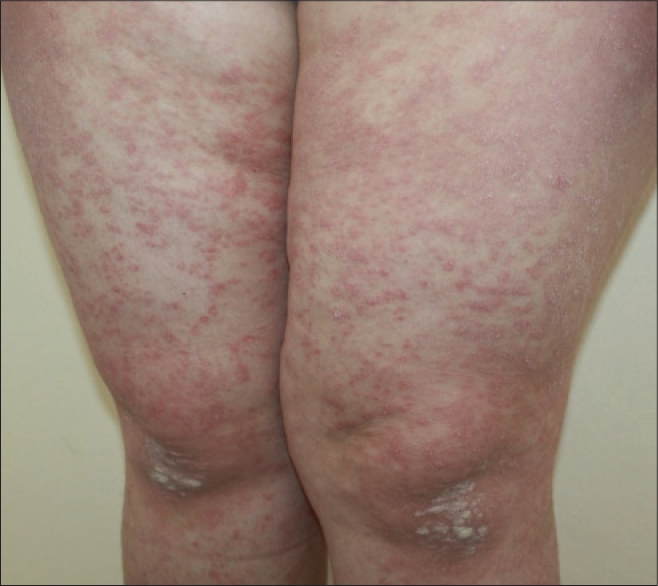 |
| Figure 1: Erythematous follicular papules and plaques over the lower limb, with islands of normal skin |
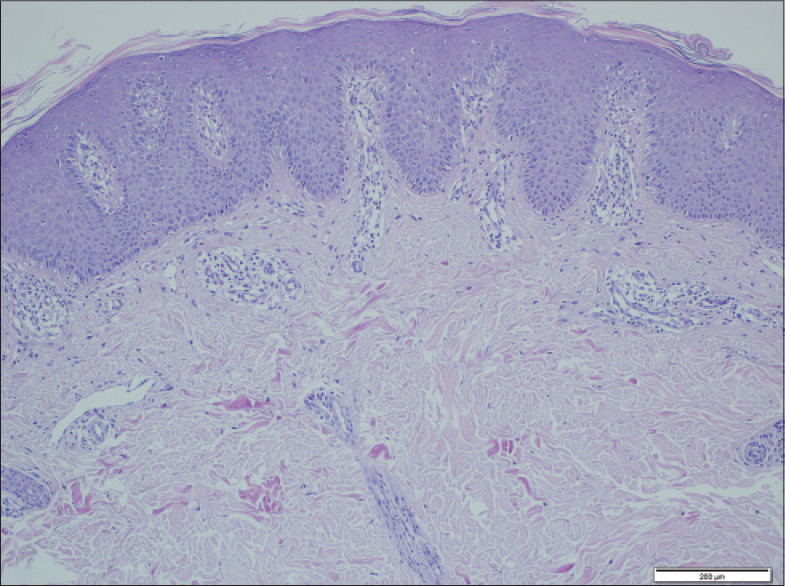 |
| Figure 2: Hyperkeratosis, irregular acanthosis, and thick suprapapillary plates (H and E, x100) |
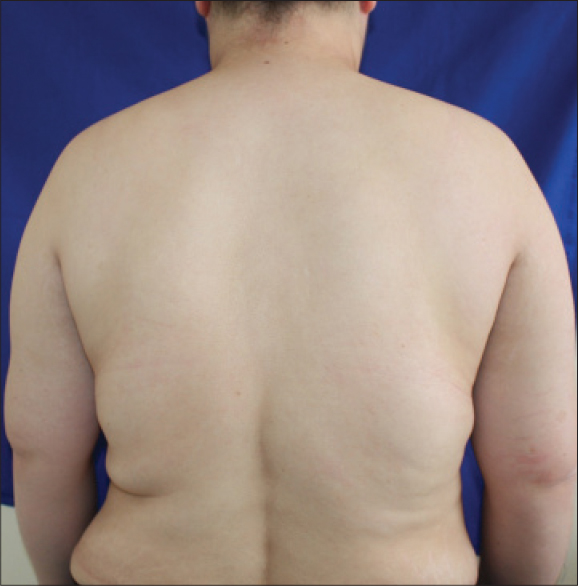
Based on the clinical and histopathological findings, the patient was diagnosed with pityriasis rubra pilaris. The patient had previously received systemic retinoids, phototherapy (nbUVB, PUVA), retinoic acid and nbUVB (re-nbUVB) combination, with no improvement. She developed erythroderma since the last 4 months [Figure - 3]. We treated her with methotrexate 15 mg/week for 3 months but the patient's lesions did not improve. Infliximab therapy was planned after ruling out contraindications. Two doses of 5 mg/kg of intravenous infliximab was administered at a two week interval, which resulted in a near total disease regression [Figure - 4]. The patient continued to receive this therapy similar to our psoriasis protocol (week 0, 2, 6, and then once in 2 months for a total duration of 1 year). She did not have any relapse after stopping medications during her two years of follow up.
 |
| Figure 3: Erythroderma |
 |
| Figure 4: Total resolution after treatment |
The treatment of pityriasis rubra pilaris is based upon anecdotal reports due to its rarity, lack of controlled studies and idiopathic nature of the disorder. Many therapies have been used to treat this condition and include high-dose vitamin A, systemic retinoids, methotrexate, azathioprine, cyclosporine, stanozolol, phototherapy and extracorporeal phototherapy. Systemic retinoids and methotrexate are most commonly used. Considering the overlapping characteristics of pityriasis rubra pilaris and psoriasis in terms of clinical appearance and response to therapy, previous studies have reported that biologicals with proven efficacy in psoriasis can also be used for the treatment of pityriasis rubra pilaris.[3]
TNF-alpha is a pro-inflammatory cytokine that acts as an immunomodulator in various systemic and dermatological disorders. Infliximab is a chimeric monoclonal antibody that binds to TNF-alpha. The drug was initially developed for the treatment of Crohn's disease. Subsequent reports indicated efficacy in the treatment of inflammatory dermatoses including psoriasis, hidradenitis suppurativa and pyoderma gangrenosum.[4] In 2013, a systematic review on the use of TNF-alpha antagonists in patients with type 1 pityriasis rubra pilaris was published.[5] A total of 15 patients received therapy with TNF-alpha antagonists, and there was complete response in 12 (80%) patients, partial response in two, and no response in one patient. TNF-alpha antagonists such as infliximab, etanercept or adalimumab were used in the treatment of patients as monotherapy, or in combination with other drugs such as methotrexate and acitretin. Infliximab was the most commonly used TNF-alpha antagonist. A dose of 5 mg/kg was administered at weeks 0, 2, 6, and then every 8 weeks in accordance with the treatment protocol for psoriasis. None of the patients developed any side effects. Considering the rapid and excellent response to infliximab, the researchers suggested that TNF-alpha plays a very important role in the pathophysiology of pityriasis rubra pilaris.[5]
Infliximab can be used as an alternative in the treatment of patients with adult onset treatment resistant pityriasis rubra pilaris. However, larger studies are necessary to establish the efficacy of the drug.
| 1. |
Misery I, Faure M, Claidy A. Pityriasis rubra pilaris and human immunodeficiency virus infection – type 6 pityriasis rubra pilaris?. Br J Dermatol 1996;135:1008-9.
[Google Scholar]
|
| 2. |
Behr FD, Bangert JL, Hansen RC. Atypical pityriasis rubra pilaris associated with arthropathy and osteoporosis: A case report with 15-year follow-up. Pediatr Dermatol 2002;19:46-51.
[Google Scholar]
|
| 3. |
Liao WC, Mutasim DF. Infliximab for the treatment of adult-onset pityriasis rubra pilaris. Arch Dermatol 2005;141:423-5.
[Google Scholar]
|
| 4. |
Ruiz-Genao DP, Lopez-Estebaranz JL, Naz-Villalba E, Gamo-Villegas R, Calzado-Villarreal L, Pinedo-Moraleda F. Pityriasis rubra pilaris successfully treated with infliximab. Acta Derm Venereol 2007;87:552-3.
[Google Scholar]
|
| 5. |
Petrof G, Almaani N, Archer CB, Griffiths WA, Smith CH. A systematic review of the literature on the treatment of pityriasis rubra pilaris type 1 with TNF-antagonists. J Eur Acad Dermatol Venereol 2013;27:131-5.
[Google Scholar]
|
Fulltext Views
3,774
PDF downloads
2,331





