Translate this page into:
Evaluation of an ablative and non-ablative laser procedure in the treatment of striae distensae
2 Department of Pathology, Okmeydanı Training and Research Hospital, Istanbul, Turkey
Correspondence Address:
Sule Gungor
Dar�lacize Street, Okmeydan? Hospital, ?i?li- 34000, Istanbul
Turkey
| How to cite this article: Gungor S, Sayilgan T, Gokdemir G, Ozcan D. Evaluation of an ablative and non-ablative laser procedure in the treatment of striae distensae. Indian J Dermatol Venereol Leprol 2014;80:409-412 |
Abstract
Background: Striae distensae or stretch marks are atrophic linear dermal scars with epidermal atrophy. There are many therapeutic options for management, but no consistently effective modality is available yet. Objective: We compared the efficacy of 1064 nm long pulse (LP) Nd: YAG laser and 2940 nm variable square pulse (VSP) erbium: YAG laser in the treatment of striae distensae. Methods: Twenty female volunteers (Fitzpatrick skin types II-V) aged between 20 and 40 years with striae (3 patients with the rubra type and 17 with the alba type) were enrolled in the study. The duration of striae ranged from 4 months to 12 years. Lesions were located on the abdomen in all patients except one patient who had striae on the arms and two patients with striae in the lumbar region. Treatments were randomly allocated to both sides of the body in each patient, one side being treated with VSP erbium: YAG laser and the opposite side with LP Nd: YAG laser. All subjects were treated monthly for a total of three treatments. Two 3-mm punch biopsies were obtained from six subjects, both of the same striae, one before the first treatment and one 4 weeks after the last session. Results: Response was evaluated clinically by photographic comparison and was found to be poor in 17 subjects, both on the LP Nd: YAG laser treated side and VSP erbium YAG laser treated side. All these patients had mature lesions (striae distensae alba). Three subjects had a moderate response on both sides; these patients' striae were immature (striae distensae rubra). Histologically, elastic fibers were slightly increased in post-treatment samples compared with pretreatment skin biopsies. Conclusion: We observed no satisfactory clinical improvement in striae distensae alba lesions although histopathological changes were seen. We suggest that variable square pulse Er: YAG and long pulse Nd: YAG lasers are not useful in the treatment of striae distensae alba.INTRODUCTION
Striae distensae, also known as stretch marks, are atrophic linear dermal scars with epidermal atrophy which occur after excessive dermal stretching and/or under the influence of estrogens and corticosteroids. [1] Though striae do not present any significant medical issues, they are a cause of cosmetic concern. Many therapeutic modalities have been tried including topical tretinoin, microdermabrasion, radiofrequency, photothermolysis, intense pulsed light, ablative and non-ablative lasers and fractional lasers; but no consistently effective modality is available yet. [2] Lasers have recently been advertised as an effective treatment alternative but most studies report contradictory results. Treatment with the long-pulsed (LP) 1064 nm neodymium-doped yttrium aluminum garnet (Nd: YAG) laser is known to induce production of dermal collagen and it has been used successfully in the non-ablative treatment of wrinkles and atrophic scars. [3] The variable square pulse (VSP) 2940 nm erbium: yttrium aluminum garnet Er: YAG laser has also been used for both the ablative and non-ablative treatment of wrinkles, atrophic scars and striae. [4],[5] VSP Er: YAG laser has both ablative (short pulse) and non-ablative (smooth pulse) effects on the tissue. [6] Since striae have both a clinical and histological resemblance to atrophic scars, these two laser procedures could be effective for treating them as well. Therefore, the goal of this study was to compare the efficacy of the LP Nd: YAG laser and the VSP Er: YAG laser in the treatment of striae distensae.
METHODS
The study protocol was approved by the ethics committee and written informed consent to participate in the trial was obtained from each patient.
Exclusion criteria included a history of keloidal scarring or connective tissue disease, the use of vitamin A derivatives within 6 months prior to recruitment in the study, any previous treatment for striae distensae, pregnancy and the use of systemic drugs.
A total of 20 female volunteers (Fitzpatrick skin types II-V) between the ages of 20 to 40 years with striae distensae (three patients with the rubra type and the others with alba type) were enrolled in the study. The duration of striae ranged from 4 months to 12 years. All patients had lesions on the abdomen except one who had lesions on the arm and two who had involvement of the lumbar region.
Prior to the laser procedure, eutectic mixture of local anaesthetics (EMLA® ) topical anesthetic cream was applied under an occlusive dressing for 45 minutes and subsequently cleaned with distilled water.
The subjects were then treated on a randomly selected side with the VSP 2940 nm Er: YAG laser. The procedure was performed with one pass in the smooth mode (250 ms) at 3.2 joules with a 7 mm spot size and a 50% overlap, following two passes in the short pulse mode (0.3 ms) at 1 joule with a 7 mm spot size and a 50% overlap. The 1064 nm LP Nd: YAG laser procedure was performed on the opposite side using two passes with 50ms pulse duration at 50J/cm² with a 6 mm spot size and a 50% overlap. To minimize treatment discomfort, a cold air cooling device was used to cool the skin during laser irradiation. After the conclusion of the procedure, a fragrance-free moisturizing cream was applied three times a day for 1 week.
All subjects received a total of three treatments administered at monthly intervals and the side effects were recorded at each treatment session. Photographic documentation was obtained baseline and 4 weeks after the last session using the same camera (Canon EOS 500D). Two blinded dermatologists then made clinical assessments by evaluating the photographs according to evaluation scores. More than 66% visual improvement was rated as a good response, 33-66% visual improvement was rated a moderate response, less than 33% visual improvement was rated a poor response.
Two 3-mm punch biopsies from the same striae (one before the first treatment and the other 4 weeks after the last session) were obtained from six subjects. Five biopsies were performed on the erbium laser-treated side while one biopsy was performed on the Nd: YAG laser-treated side. All the sections were stained with hematoxylin and eosin (H and E), elastica von Gieson (EVG), orcein, and Masson′s trichrome (MT) stain in order to study the overall skin structure and in particular the elastin and collagen fibers. The thickness of the epidermis and dermis was then recorded using ocular micrometers.
RESULTS
Seventeen subjects with mature striae distensae (alba type) had a poor response to both the laser types [Figure - 1] while the remaining 3 patients who had immature striae distensae (rubra type) were evaluated as having a moderate response to both laser procedures [Figure - 2].
 |
| Figure 1: Poor response to both laser types in mature striae |
 |
| Figure 2: Moderate response to both laser types in immature striae |
Mild long-acting erythema and post-inflammatory hyperpigmentation was noted in six of the patients on the VSP Er: YAG side [Figure - 3]. No complications were noted on the LP Nd: YAG laser-treated side. No other side effects, such as scarring or wound infection, were observed with either laser treatment.
No consistent difference in epidermal thickness was observed on histopathology before and after treatment. An examination of the EVG and orcein-stained slides revealed that the number of elastin fibers was slightly increased in the post-treatment samples compared with the pre-treatment skin biopsies [Figure - 4]. The newly formed fibers were usually thin and arranged in reticular, branching patterns that were located perpendicular to the epidermis. In one of the cases, the fibers were also slightly thickened. The Massons trichrome-stained sections showed that the collagen fibers were aligned almost parallel to the epidermis in four of the cases (all treated with VSP Er: YAG laser) in the post-laser biopsies, but for another participant (treated with Nd: YAG laser treated SD sample), these fibers were not as parallel.
 |
| Figure 3: Long-acting erythema observed on the side of erbium:YAG laser application, but no side effect observed on the side of Nd:YAG laser application |
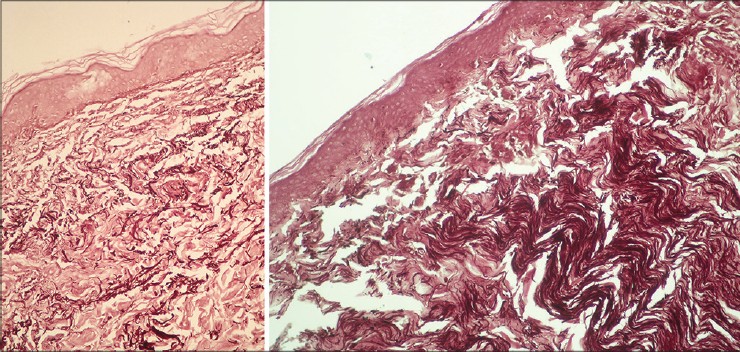 |
| Figure 4: The number of elastin fibers was slightly increased in the post-treatment samples compared with the pre-treatment skin biopsies (Orcein, ×400) |
DISCUSSION
Despite various therapeutic modalities being available, the treatment of sriae distensae remains a challenge. Various laser systems are currently being promoted for their treatment. [2],[7],[8] The non-ablative long pulse Nd: YAG laser and ablative Er: YAG laser have been suggested as effective methods of treatment for striae distensae in previous studies. When we compared the efficacy of these two methods, patients with the mature, alba type of striae distensae had poor clinical improvement with both laser types. However, both laser treatments were moderately successful with immature striae distensae of the rubra type.
Variable Square Pulse (VSP) technology Er: YAG lasers have variable pulse widths and pulse sequences allowing the practitioner to select the effect of the laser from "cold" ablation peeling to deeper thermal coagulation. At high fluences and low pulse durations, the speed of ablation is faster than the diffusion of heat into the tissue so that all of the laser energy is used up for ′cold ablation′. With decreasing fluences and/or longer pulse widths, the thermally affected tissue layer at the end of the pulse becomes thicker, thermal effects become more pronounced and ablation efficiency is considerably reduced, termed as ′warm ablation′ and at even lower energies as ′hot ablation′. At fluences below the ablation threshold there is no ablation and this is known as ′smooth mode′. In this mode, laser energy is transmitted as heat into the skin surface without any resulting ablation and is then dissipated into the deeper tissue layers. The effect of smooth mode is mainly thermal modification of the skin without any significant ablation of the epidermis. Histological investigations show that smooth mode treatments result in collagen thermal effects that extend deeper than 100 μm below the epidermal-dermal junction. Clinically, this collagen thermal effect results in visible and long-lasting reduction of wrinkles and scars. [6]
Histopathologically, striae distensae show loss of the supporting material i.e. the collagen and the elastin fibers compared to normal skin, which reduces the thickness and stability of the dermis. There is also flattening of the rete ridges resulting in thinning of the epidermis. In our study, after therapy, though the epidermal and dermal thickness did not change, the amount of both elastin and collagen fibers increased in dermis but it seems this increase was not enough to be clinically apparent. The collagen fibers on the side treated with the long pulse Nd: YAG laser showed decreased parallelism whereas the same fibers on the side treated with the variable square pulse Er: YAG laser became more parallel. This can be interpreted to indicate that the effects of the VSP Er: YAG laser on collagen fibres are similar to those seen in wound healing and scar formation. On the other hand, following treatment with long pulse Nd: YAG laser, the pattern of fibers is closer to normal skin.
There are inconsistent results described in the literature regarding the management of the striae distensae by different laser systems. Yang et al. [9] showed the effectiveness of the CO 2 laser, and Suh et al. [10] demonstrated the efficacy of the pulsed dye laser. However, Nehal et al. [11] showed no clinical or histological improvement of alba type of striae distensae when pulsed dye laser was used. Furthermore, Jimenez et al. [12] showed that the pulsed dye laser was effective for rubra lesions but not alba lesions. In another study conducted with a diode laser on 11 patients with striae distensae, Tay et al. [13] reported no clinical improvement on photographic evaluation. Finally, Goldman et al. [14] used the 1064 nm LP Nd: YAG laser on 20 patients who had immature striae and observed clinical improvement. In recent years, fractional lasers have become more popular in the treatment of strial distensal due to fewer side effects and a better response. [7]
CONCLUSION
We observed no satisfactory clinical improvement with regard to strial distensal alba lesions, although histopathological changes did take place. We recommend that the VSP Er: YAG and long pulse Nd: YAG lasers not be used for the treatment of striae distensae of the alba type. They may be moderately helpful in treating striae distensae of the rubra type. Randomized controlled studies are needed to evaluate the efficacy of lasers for the treatment of striae distensae.
| 1. |
Alster TS, Handrick C. Laser treatment of hypertrophic scars, keloids and striae. Semin Cutan Med Surg 2000;19:287-92.
[Google Scholar]
|
| 2. |
Elsaie ML, Baumann LS, Elsaaiee LT. Striae distensae (stretch marks) and different modalities of therapy: An update. Dermatol Surg 2009;35:563-73.
[Google Scholar]
|
| 3. |
Min SU, Choi YS, Lee DH, Yoon MY, Suh DH. Comparison of a long-pulse Nd: YAG laser and a combined 585/1,064-nm laser for the treatment of acne scars: A randomized split-face clinical study. Dermatol Surg 2009;35:1720-7.
[Google Scholar]
|
| 4. |
Wanitphakdeedecha R, Manuskiatti W, Siriphukpong S, Chen TM. Treatment of punched-out atrophic and rolling acne scars in skin phototypes III, IV, and V with variable square pulse erbium: Yttrium-aluminum-garnet laser resurfacing. Dermatol Surg 2009;35:1376-83.
[Google Scholar]
|
| 5. |
Wanitphakdeedecha R. Treatment of striae distensae with variable square pulse Erbium: YAG laser resurfacing. J Laser Health Acad 2012;1:S15.
[Google Scholar]
|
| 6. |
Lukac M, Perhavec T, Nemes K, Ahcan U. Ablation and thermal depths in VSP Er: YAG laser skin resurfacing. J Laser Health Acad 2010;1:56-71.
[Google Scholar]
|
| 7. |
De Angelis F, Kolesnikova L, Renato F, Liguori G. Fractional nonablative 1540-nm laser treatment of striae distensae in Fitzpatrick skin types II to IV: Clinical and histological results. Aesthet Surg J 2011;31:411-9.
[Google Scholar]
|
| 8. |
Al-Dhalimi MA, Abo Nasyria AA.A comparative study of the effectiveness of intense pulsed light wavelengths (650 nm vs 590 nm) in the treatment of striae distensae. J Cosmet Laser Ther 2013;15:120-5.
[Google Scholar]
|
| 9. |
Yang YJ, Lee GY. Treatment of striae distensae with nonablative fractional laser versus Ablative CO (2) fractional laser: A randomized controlled trial. Ann Dermatol 2011;23:481-9.
[Google Scholar]
|
| 10. |
Suh DH, Chang KY, Son HC, Ryu JH, Lee SJ, Song KY. Radiofrequency and 585-nm pulsed dye laser treatment of striae distensae: A report of 37 Asian patients. Dermatol Surg 2007;33:29-34.
[Google Scholar]
|
| 11. |
Nehal KS, Lichtenstein DA, Kamino H, Levine VJ, Ashinoff R. Treatment of mature striae with the pulsed dye laser. J Cutan Laser Ther 1999;1:41-4.
[Google Scholar]
|
| 12. |
Jiménez GP, Flores F, Berman B, Gunja-Smith Z. Treatment of striae rubra and striae alba with the 585-nm pulsed-dye laser. Dermatol Surg 2003;29:362-5.
[Google Scholar]
|
| 13. |
Tay YK, Kwok C, Tan E. Non-ablative 1,450-nm diode laser treatment of striae distensae. Lasers Surg Med 2006;38:196-9.
[Google Scholar]
|
| 14. |
Goldman A, Rossato F, Prati C. Stretch marks: Treatment using the 1,064-nm Nd: YAG laser. Dermatol Surg 2008;34:686-92.
[Google Scholar]
|
Fulltext Views
5,321
PDF downloads
2,550





