Translate this page into:
Evaluation of cervical and anal intraepithelial neoplasia in women attending a sexually transmitted infection clinic
2 Department of Obstetrics and Gynaecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, New Delhi, India
3 Department of Pathology, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, New Delhi, India
Correspondence Address:
Deepika Pandhi
Department of Dermatology and STD, University College of Medical Sciences and Guru Teg Bahadur Hospital, University of Delhi, New Delhi - 110 095
India
| How to cite this article: Bisherwal K, Pandhi D, Singal A, Guleria K, Mishra K. Evaluation of cervical and anal intraepithelial neoplasia in women attending a sexually transmitted infection clinic. Indian J Dermatol Venereol Leprol 2016;82:498-504 |
Abstract
Background: The incidence of anal and cervical cancers and their precursors have increased in the past decades. Women with HIV and sexually transmitted infections are at a higher risk. Cervical human papilloma virus infection may serve as a reservoir and source of anal infection or vice versa. A higher incidence of anal cytological abnormality has been observed in patients with abnormal cervical cytology. Objectives: This cross sectional study was designed to estimate the prevalence and associations of anal and cervical cytological abnormalities in a cohort of sexually active women using Papanicolaou smears. Methods: We conducted a single centre study of 35 consecutive HIV positive and 40 HIV negative women attending the sexually transmitted infection clinic. Cervical and anal specimens were obtained for cytology after a detailed history and examination. Chi square test and coefficient of correlation were used for comparison. Results: Cervical dysplasia was observed in 22.6% (17.3% low-grade squamous intraepithelial lesion and 5.3% high grade squamous intraepithelial lesion) and anal dysplasia in 8% study subjects (6.7% low-grade squamous intraepithelial lesion and 1.3% high grade squamous intraepithelial lesion); no association was observed with HIV infection. A higher number of patients with cervical dysplasia (29.4%) were found to have concomitant anal dysplasia (P = 0.002). History of anal intercourse was reported in all patients with anal dysplasia and was higher (P < 0.037) in patients with cervical dysplasia. Limitations: The limitations included a small sample size, lack of correlation with histological findings and bias due to STI clinic-based recruitment of the study population. Conclusion: Cytology may be used to screen for cervical and anal dysplasia in women irrespective of HIV status. Women with cervical dysplasia may be preferentially screened for anal dysplasia and vice versa. Anal intercourse may be a risk factor for anal and cervical dysplasia.Introduction
Globally, an estimated 33.4 million people are currently living with human immunodeficiency virus (HIV) infection, the proportion of women being slightly less than 52 percent. Although HIV prevalence in India is low, it is among the seven countries in Asia which account for more than 90% of people living with HIV infection, due to it being the second most populous country in the world.[1]
Cervical cancer and its precursors are the most important gynecological consequences of HIV infection. Among women with HIV infection in the United States of America, a relative risk of 5.4 for cervical cancer has been found as compared to the general population.[2] In India, cancer of the cervix constitutes about 15–51% of all cancers in women and rates of age-standardized incidence range from 17.2 to 55/100,000 women.[3]
Likewise, the incidence of anal cancer is on the rise in tandem with an increase in the prevalence of human papillomavirus (HPV)-related disease and HIV infection.[4] According to recent data from the United States and Europe, the incidence of anal cancer among HIV positive individuals ranges from 42 to 137 cases/100,000 person-years, a rate that is 30–100 times higher than that of the general population, women being more frequently affected than men.[4],[5] The incidence of anal cancer in India was 99,000 in 2002, 60% of cases occurring in women.[6] The incidence of both these cancers and their precursor lesions have increased in the past decades with the higher risk being attributed to various reasons such as HIV infection, low CD4 counts, multiple sex partners, history of cigarette smoking, anal intercourse and the presence of other sexually transmitted infections.[7],[8]
In women, anogenital HPV infection is likely to be multicentric with the cervix serving as a reservoir and source of anal infection, or vice versa.[9],[10] Since there is a possibility of HPV autoinoculation (e.g. transmission from the cervico-vaginal compartment to the anal mucosa) in women, anal intercourse has been postulated to be an important risk factor for the development of anal cancer.[11],[12],[13] However, anal intercourse as a risk factor for cervical cancer has not been evaluated. Further, there is a paucity of studies documenting both the incidence of cervical and anal dysplasia as well as their simultaneous correlation.[11],[14] In the few studies correlating anal and cervical dysplasia, a higher incidence of anal cytological abnormality has been observed in patients with abnormal cervical cytology.[15],[16],[17] We were unable to find any previous studies from Asia on the subject of anal dysplasia in women, concurrent cervical and anal dysplasia in women or a comparison of anal and cervical dysplasia in HIV-positive women. Cytology using conventional Papanicolaou smears is a useful screening method for detecting anal and cervical squamous intraepithelial lesions.[18] Therefore, this study was planned to screen women attending our sexually transmitted infection clinic for both cervical and anal dysplasia using cytology (Papanicolaou smear). This is important, particularly in resource-constrained countries such as India where there is limited availability of colposcopy and high-resolution anoscopy. Patients with dysplasia on cytological evaluation can preferentially be taken up for further evaluation, biopsy and management.
Methods
Study population
This cross-sectional study was performed at the sexually transmitted infection clinic of Guru Teg Bahadur Hospital, New Delhi, India. Forty consecutive HIV-positive and 35 high-risk HIV-negative sexually active women, aged between 18 and 45 years, attending the clinic between November 2011 and April 2013 and consenting to be a part of the study were included. Women at “high risk” were those reporting any of the following: reporting multiple sexual partners, sex with a person having multiple sexual partners, anal intercourse or any sexually transmitted infection. Patients who presented with ulcerations were sampled for cytology after treatment of the ulcers. The study was approved by the Institutional Research Ethics Committee.
Study design
After obtaining written informed consent, each subject was asked to provide a detailed history on their routine gynecological health and the risk factors associated with development of cytological abnormalities. This assessment, done by means of a predesigned questionnaire, included demographic details, medical history, sexual practices, addictions and HIV status (confirmed by documentary evidence). CD4 counts at the time of diagnosis of HIV infection were also noted. Following this, a detailed visual examination was performed. Laboratory investigations included hemogram, Venereal Disease Research Laboratory (VDRL) test and tests to confirm sexually transmitted infection such as Grams stained smear, tzanck smear, Treponema pallidum hemagglutination assay (TPHA), gonococcal culture and chlamydia antigen test. Corresponding cervical samples anal and anal cytology specimens were taken with a moistened cytobrush by a single clinician, fixed and stained according to the Papanicolaou protocol. The cytosmears were then reviewed independently by the pathologist who was blinded to the clinical details to avoid bias. The minimum criterion for adequate cellularity was taken as >1000 cells for anal smears and >7000 cells for cervical smears. The diagnosis for both anal and cervical smears was classified according to Bethesda classification 2001 as: negative for intraepithelial lesions; atypical squamous cells of undetermined significance; low-grade squamous intraepithelial lesion; atypical squamous cells of undetermined significance which cannot exclude high-grade squamous intraepithelial lesion; high-grade squamous intraepithelial lesion.[19] Additional features such as koilocytes, dysplastic cells, abnormal flora, parakeratotic cells, anucleated, binucleated and/or multinucleated squamous cells and glandular/transitional cells, wherever seen, were also recorded.
Statistical evaluation
All statistical analysis was performed using SPSS Statistics software version 17.0 (Chicago, IL, USA). The threshold of significance was set at P (two-tailed) < 0.05 (confidence interval ¼ 95%) and P < 0.01 (confidence interval ¼ 99%) was taken as highly significant. The study subjects were subdivided into three comparison groups: HIV-positive versus HIV-negative, patients with and without cervical dysplasia and patients with and without anal dysplasia on cytology. Unpaired t-test, Chi-square test and Fischer's exact test were used to compare the parameters in various groups. The correlation of cervical and anal dysplasia as well as the correlation of CD4 count at the time of recruitment to study and grade of dysplasia was done by calculating Pearson's Chi-square coefficient.
Results
Demographic data
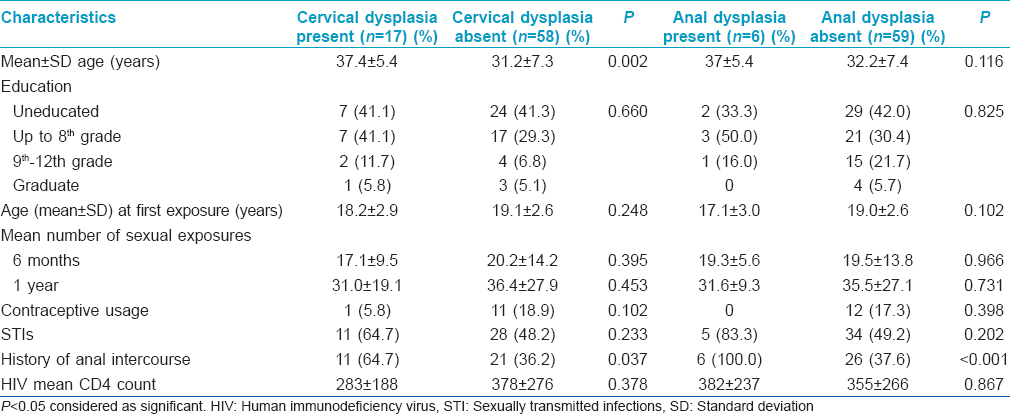
The baseline characteristics and sociodemographic information of the examined cohort (n = 75 women) are presented in [Table - 1] and [Table - 2]. Most of the patients (40%) belonged to the 30–39 years age group.
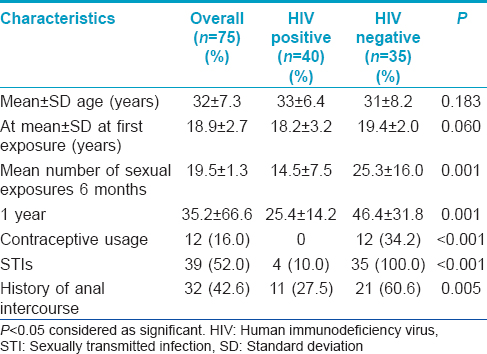
Sexual practices
All 75 patients were married. Only seven (9.3%) patients reported contact with more than one sexual partner, a history elicited more frequently in patients with cervical dysplasia (P = 0.002). History of anal intercourse was present in 32 (42.6%) of the subjects. It was reported by all patients with anal dysplasia and was also significantly associated with cervical dysplasia (P< 0.037).
Sexually transmitted infections
Vaginal discharge and genital itching were the most common complaints (34.6%), followed by abdominal pain (20.0%) and backache (17.3%). None of the patients reported anal complaints. Overall, 39 (52%) had associated sexually transmitted infections with vaginal discharge being the most common sexually transmitted infection. The presence of sexually transmitted infections was comparable in all study groups [Table - 1]. Six (10.2%) study subjects presented with genital warts while perianal warts were detected in only one seronegative patient. Paradoxically, 70% of patients without cervical dysplasia had genital warts as compared to 29% in patients with cervical dysplasia; the difference being statistically significant (P = 0.006). However, there was no statistical difference between patients with and without anal dysplasia (P = 0.094).
CD4 count in HIV-positive patients
Among the 40 HIV positive patients, 16 (40%) were on highly active antiretroviral therapy. There was no correlation of CD4 count at time of recruitment with degree of anal dysplasia (R = −0.003, P = 0.986) and cervical dysplasia (R = –0.227, P = 0.177) [Table - 2].
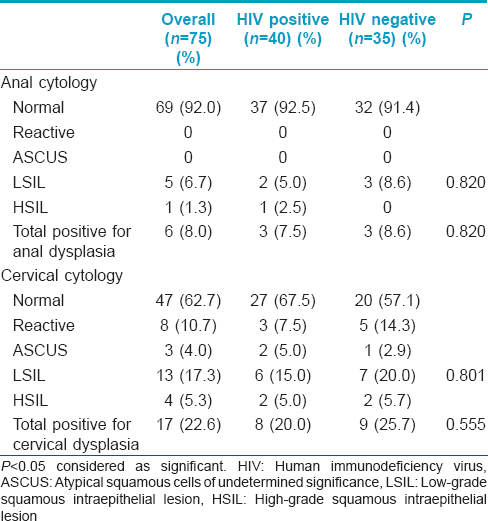
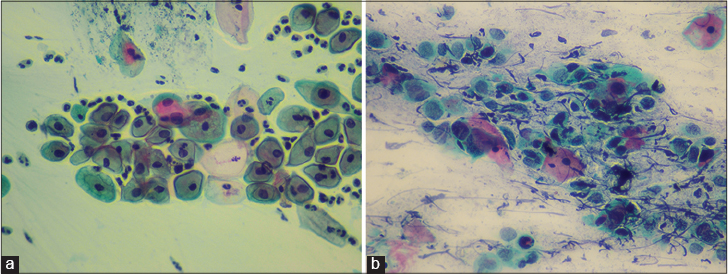
Anal cytology
The findings of anal cytological evaluation with Papanicolaou smear are depicted in [Table - 3]. Overall, 6 (8%) had abnormal anal cytology; the incidence of a low-grade squamous intraepithelial lesion was comparable in HIV-positive (7.5%) and HIV-negative (8.6%; P = 0.820) patients. High-grade dysplasia was recorded only in one HIV-positive patient [Figure - 1]a and [Figure - 1]b. Abnormal flora was evident in 49.3%, columnar cells in 78.6% and inflammatory cells in 29.3% of anal cytology smears.
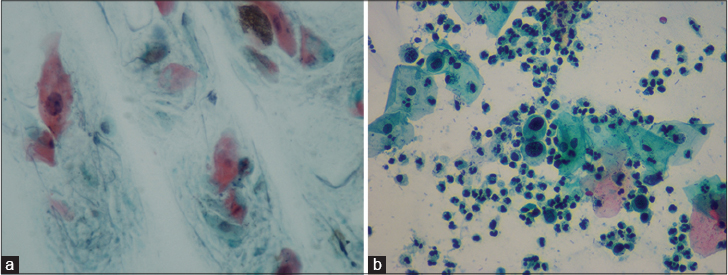 |
| Figure 1: (a) Anal smears showing normal cells and low-grade squamous intraepithelial lesion (Pap, ×400). (b) Anal Papanicolaou smear showing high-grade squamous intraepithelial lesion (Pap, ×400) |
Cervical cytology
[Table - 3] depicts the findings of cervical cytological evaluation with Papanicolaou smear. Overall, 28 (37.3%) subjects had abnormal cervical cytology including reactive, atypical squamous cells of undetermined significance, low-grade squamous intraepithelial lesion and high-grade squamous intraepithelial lesions, which were more frequent in the HIV-negative group (15 subjects [42.9%]) as compared to the HIV-positive group (13 subjects [32.5%]) [Figure - 2]a and [Figure - 2]b. However, dysplastic changes (low-grade squamous intraepithelial lesion and high-grade squamous intraepithelial lesion) were comparable in the HIV positive (eight subjects [25.7%]) and HIV negative groups (nine subjects [20%]) (P = 0.555). A reactive nuclear enlargement was observed in 8 (10.7%) smears, low-grade squamous intraepithelial lesion in 13 (17.3%) smears and a high-grade squamous intraepithelial lesion in 4 (5.3%) smears. Six (15%) subjects in the HIV-positive and 7 (20%) subjects in the HIV-negative group showed a positive cytology for low-grade squamous intraepithelial lesion with the difference not being statistically significant (P = 0.801). Similarly, high-grade dysplasia was also comparable in both HIV-positive and HIV-negative groups (5.0% vs. 5.7%). Abnormal flora was seen in 50.6%, columnar cells in 73.3% and inflammatory cells in 32.0% of cervical cytology smears.
 |
| Figure 2: (a) Cervical smear showing koilocytes and low-grade squamous intraepithelial lesion (Pap, ×400). (b) Cervical smear showing high-grade squamous intraepithelial lesion and inflammatory cells (Pap, ×400) |
Cervical and anal cytology
A significantly higher number of patients, 17 (29.4%) with cervical dysplasia were found to have anal dysplasia on anal cytological smears as compared to patients without cervical dysplasia (P = 0.002). The correlation of grade of cervical dysplasia with degree of anal dysplasia using Pearson's coefficient of correlation showed a statistically significant (R = −0.381, P = 0.001) negative correlation. Therefore, patients with a higher grade of cervical dysplasia were more likely to have concomitant anal dysplasia.
Discussion
Cervical and anal squamous lesions are a common finding, especially in HIV-infected patients and the incidence of both these cancers and their precursor lesions have increased in the past decades.[2] Although anal squamous cell carcinoma is rare in the general population, it is the fourth most commonly reported malignancy in HIV-positive individuals.[20]
Cytology has been proposed as a potential cost-effective and simple screening tool in the evaluation of anorectal and cervical specimens because of the morphologic similarities of anal and cervical cancer and intraepithelial neoplasia.[18] Previous studies on anal dysplasia have mostly targeted HIV-positive women and have reported anal dysplasia ranging from 10% to 33%.[14], 16, [21],[22],[23],[24],[25] The results of our study with 8% of our study subjects having anal dysplasia are marginally lower than the range reported so far in the literature, which has mostly originated from Europe and the American continent. The comparable rates of dysplasia obtained in this study need validation in larger multicentric studies as no previous attempts have been made to compare the risk of anal dysplasia between HIV-positive and HIV-negative groups in Asian women.
Abnormal cervical cytology was observed in 28 (37.3%) and cervical dysplasia in 17 (22.6%) of the study subjects. Various studies have reported that the prevalence of dysplastic changes range between 5% and 34% among HIV-positive women and 9–43.5% in HIV-negative women.[26],[27],[28],[29] The data from our study lies in between these ranges. However, a much higher prevalence of cervical dysplasia in HIV-positive as compared to HIV-negative women has been reported in studies which have recruited HIV-positive women from antiretroviral therapy clinics and HIV-negative women from gynecology outpatient departments.[11],[28] Our study failed to reproduce these results, which could be attributed to the presence of sexually transmitted infections in all the HIV-negative patients, due to their direct recruitment from the sexually transmitted infection clinic, whereas only 10% of the HIV-positive patients had these. This emphasizes the need for screening of dysplasia in sexually transmitted infection patients, irrespective of HIV status.
Anogenital HPV infection in women is likely to be multicentric and cervical HPV infection may serve as a reservoir and source of anal infection or vice versa. In a recent study analyzing the relationship between anal and cervical HPV infection in women, it was seen that the cervical, anal and concurrent cervical and anal area involvement was seen in 82.6%, 48.3% and 42.4% of women in the study group as against 28.0%, 26.0% and 8.0% of women in the control group, respectively.[29] Concurrent infections of the cervix and anus occurred 5.3 times more often in their study group than in the control group. This multicentric HPV infection might be a plausible explanation for the concurrent occurrence of non-cervical malignancies induced by HPV, including that of the anal canal. This is further supported by a recent database study wherein incidence of anogenital and head and neck malignancies in women with a previous diagnosis of cervical intraepithelial neoplasia was analyzed.[30] It was found that the crude incidence rate for anal cancers was 3.7/100,000 person-years and the standardized incidence ratio was 1.8 (95% confidence interval: 0.4–4.7). Similarly, in a recent study including 196 women with HPV-positive related cervical abnormalities, Lammé et al. reported the prevalence of abnormal anal cytology to be 17.6% and prevalence of anal HPV to be 32.5%.[17]
In our study, 17 (29.4%) patients with cervical dysplasia were found to have concomitant anal dysplasia on cytology. Calore et al., in their cohort of 49 women reported a much higher incidence of anal cytological abnormality (59.2%) in patients with abnormal cervical cytology.[15] Gingelmaier et al. also reported that 9 (69.2%) of their 13 patients with anal dysplasia had cervical dysplasia (69.2%).[16] The SUN study on 167 HIV-infected women also found that the presence of abnormal cervical cytology was associated with the presence of abnormal anal cytology (relative risk: 1.7, P = 0.024).[13]
In addition, in women, HPV autoinoculation (e.g. transmission from the cervico-vaginal compartment to the anal mucosa) is certainly possible.[11] Anal intercourse has, therefore, been postulated to be an important risk factor. Anal intercourse as a risk factor for cervical cancer has not been evaluated in the literature. Moreover, there are only a few studies evaluating its role in anal cancer. A recent study has shown that any frequency and any type of contact (penetrative or non-penetrative) with the anus is an important risk factor for concurrent HPV infection.[12] Hessol et al. also reported anal intercourse to be a risk factor for low-grade squamous intraepithelial lesions in women (odds ratio 3.2, 95% confidence interval 1.5–6.8) in their study.[11] However, the SUN study found no association of history of anal sex with anal HPV infection or abnormal anal cytology.[13] A history of anal intercourse was elicited in 32 (42.6%) of our study subjects; interestingly, history of anal intercourse was reported in all patients with anal dysplasia and in significantly higher (P< 0.037) numbers of patients with cervical dysplasia. Thus, history of anal intercourse emerged as a major risk factor for both anal and cervical dysplasia.
This pilot study from the Indian subcontinent describes the demographic data and potential risk factors for the occurrence of intraepithelial lesions among HIV-positive and high-risk HIV-negative women who were attending sexually transmitted infection clinics. Besides history of anal intercourse as discussed above, other factors such as mean age of first sexual exposure, mean number of sexual exposures in the last one year, number of sexual partners, contraceptive usage, history of anogenital warts and sexually transmitted infections were not found to be associated with a higher prevalence of cervical and anal dysplasia. The contribution of these risk factors toward the development of anal dysplasia needs further evaluation in a larger cohort.
Our study suffered from some limitations such as a small sample size, lack of correlation with histological findings and recruitment of the study population from a sexually transmitted infection clinic, thereby creating a bias.
Conclusion
Our pilot study highlights the importance of anal Papanicolaou smear cytology, risk of concurrent anal and cervical dysplasia and anal intercourse as a risk factor in Indian women. Large population-based multicentric studies spanning the whole subcontinent are recommended for further corroboration.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Grulich AE. HIV, immune deficiency and malignancy. J Int AIDS Soc 2008; 11:324-35.
[Google Scholar]
|
| 2. |
Frisch M, Biggar RJ, Goedert JJ. Human papillomavirus-associated cancers in patients with human immunodeficiency virus infection and acquired immunodeficiency syndrome. J Natl Cancer Inst 2000;92:1500-10.
[Google Scholar]
|
| 3. |
Sankaranarayanan R, Nene BM, Dinshaw K, Rajkumar R, Shastri S, Wesley R, et al. Early detection of cervical cancer with visual inspection methods: A summary of completed and on-going studies in India. Salud Publica Mex 2003; 45 Suppl 3:S399-407.
[Google Scholar]
|
| 4. |
Park IU, Palefsky JM. Evaluation and management of anal intraepithelial neoplasia in HIV-negative and HIV-positive men who have sex with men. Curr Infect Dis Rep 2010; 12: 126-33.
[Google Scholar]
|
| 5. |
Palefsky JM, Holly EA, Ralston ML, Da Costa M, Bonner H, Jay N, et al. Effect of highly active antiretroviral therapy on the natural history of anal squamous intraepithelial lesions and anal human papillomavirus infection. J Acquir Immune Defic Syndr 2001; 28:422-8.
[Google Scholar]
|
| 6. |
Meade JC, Cornelius DC. Sexually transmitted infections in the tropics. In: Rodriguez-Morales A, editor. Current Topics in Tropical Medicine. InTech; 2012. Available at: http://www.intechopen.com/books/current-topics-in-tropical-medicine/sexually-transmitted-infectins-in-the-tropics. Accessed on October 20, 2014.
[Google Scholar]
|
| 7. |
Conley LJ, Ellerbrock TV, Bush TJ, Chiasson MA, Sawo D, Wright TC. HIV-1 infection and risk of vulvovaginal and perianal condylomata acuminata and intraepithelial neoplasia: A prospective cohort study. Lancet 2002; 359:108-13.
[Google Scholar]
|
| 8. |
Hildesheim A, Brinton LA, Mallin K, Lehman HF, Stolley P, Savitz DA, et al. Barrier and spermicidal contraceptive methods and risk of invasive cervical cancer. Epidemiology 1990; 1:266-72.
[Google Scholar]
|
| 9. |
Williams AB, Darragh TM, Vranizan K, Ochia C, Moss AR, Palefsky JM. Anal and cervical human papillomavirus infection and risk of anal and cervical epithelial abnormalities in human immunodeficiency virus-infected women. Obstet Gynecol 1994;83:205-11.
[Google Scholar]
|
| 10. |
Melbye M, Smith E, Wohlfahrt J, Osterlind A, Orholm M, Bergmann OJ, et al. Anal and cervical abnormality in women – Prediction by human papillomavirus tests. Int J Cancer 1996; 68:559-64.
[Google Scholar]
|
| 11. |
Hessol NA, Holly EA, Efird JT, Minkoff H, Schowalter K, Darragh TM, et al. Anal intraepithelial neoplasia in a multisite study of HIV-infected and high-risk HIV-uninfected women. AIDS 2009; 23:59-70.
[Google Scholar]
|
| 12. |
Slama J, Sehnal B, Dusek L, Zima T, Cibula D. Impact of risk factors on prevalence of anal HPV infection in women with simultaneous cervical lesion. Neoplasma 2015; 62:308-14.
[Google Scholar]
|
| 13. |
Kojic EM, Cu-Uvin S, Conley L, Bush T, Onyekwuluje J, Swan DC, et al. Human papillomavirus infection and cytologic abnormalities of the anus and cervix among HIV-infected women in the study to understand the natural history of HIV/AIDS in the era of effective therapy (the SUN study). Sex Transm Dis 2011; 38:253-9.
[Google Scholar]
|
| 14. |
Tandon R, Baranoski AS, Huang F, de las Morenas A, Vragovic O, Sullivan M, et al. Abnormal anal cytology in HIV-infected women. Am J Obstet Gynecol 2010; 203:21.e1-6.
[Google Scholar]
|
| 15. |
Calore EE, Giaccio CM, Nadal SR. Prevalence of anal cytological abnormalities in women with positive cervical cytology. Diagn Cytopathol 2011; 39:323-7.
[Google Scholar]
|
| 16. |
Gingelmaier A, Weissenbacher T, Kost B, Kaestner R, Sovric M, Mylonas I, et al. Anal cytology as a screening tool for early detection of anal dysplasia in HIV-infected women. Anticancer Res 2010;30:1719-23.
[Google Scholar]
|
| 17. |
Lammé J, Pattaratornkosohn T, Mercado-Abadie J, Alkhas A, Robinson A, Lanneau G. Concurrent anal human papillomavirus and abnormal anal cytology in women with known cervical dysplasia. Obstet Gynecol 2014;124 (2 Pt 1):242-8.
[Google Scholar]
|
| 18. |
Salit IE, Lytwyn A, Raboud J, Sano M, Chong S, Diong C, et al. The role of cytology (Pap tests) and human papillomavirus testing in anal cancer screening. AIDS 2010; 24:1307-13.
[Google Scholar]
|
| 19. |
Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, et al. The 2001 Bethesda system: Terminology for reporting results of cervical cytology. JAMA 2002; 287:2114-9.
[Google Scholar]
|
| 20. |
Grulich AE, van Leeuwen MT, Falster MO, Vajdic CM. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: A meta-analysis. Lancet 2007; 370:59-67.
[Google Scholar]
|
| 21. |
Hou JY, Smotkin D, Grossberg R, Suhrland M, Levine R, Smith HO, et al. High prevalence of high grade anal intraepithelial neoplasia in HIV-infected women screened for anal cancer. J Acquir Immune Defic Syndr 2012; 60:169-72.
[Google Scholar]
|
| 22. |
Chaves EB, Folgierini H, Capp E, von Eye Corleta H. Prevalence of abnormal anal cytology in women infected with HIV. J Med Virol 2012; 84:1335-9.
[Google Scholar]
|
| 23. |
Baranoski AS, Tandon R, Weinberg J, Huang FF, Stier EA. Risk factors for abnormal anal cytology over time in HIV-infected women. Am J Obstet Gynecol 2012; 207:107.e1-8.
[Google Scholar]
|
| 24. |
Mallari AO, Schwartz TM, Luque AE, Polashenski PS, Rauh SM, Corales RB. Anal cancer screening in HIV-infected patients: Is it time to screen them all? Dis Colon Rectum 2012; 55:1244-50.
[Google Scholar]
|
| 25. |
Cambou MC, Luz PM, Lake JE, Levi JE, Coutinho JR, de Andrade A, et al. Anal human papillomavirus (HPV) prevalences and factors associated with abnormal anal cytology in HIV-infected women in an urban cohort from Rio de Janeiro, Brazil. AIDS Patient Care STDS 2015; 29:4-12.
[Google Scholar]
|
| 26. |
Bal MS, Goyal R, Suri AK, Mohi MK. Detection of abnormal cervical cytology in Papanicolaou smears. J Cytol 2012; 29:45-7.
[Google Scholar]
|
| 27. |
Mwakigonja AR, Torres LM, Mwakyoma HA, Kaaya EE. Cervical cytological changes in HIV-infected patients attending care and treatment clinic at Muhimbili National Hospital, Dar es Salaam, Tanzania. Infect Agent Cancer 2012; 7:3.
[Google Scholar]
|
| 28. |
Rezza G, Giuliani M, Branca M, Benedetto A, Migliore G, Garbuglia AR, et al. Determinants of squamous intraepithelial lesions (SIL) on Pap smear: The role of HPV infection and of HIV-1-induced immunosuppression. DIANAIDS Collaborative Study Group. Eur J Epidemiol 1997; 13:937-43.
[Google Scholar]
|
| 29. |
Sehnal B, Dusek L, Cibula D, Zima T, Halaska M, Driak D, et al. The relationship between the cervical and anal HPV infection in women with cervical intraepithelial neoplasia. J Clin Virol 2014; 59:18-23.
[Google Scholar]
|
| 30. |
Gaudet M, Hamm J, Aquino-Parsons C. Incidence of ano-genital and head and neck malignancies in women with a previous diagnosis of cervical intraepithelial neoplasia. Gynecol Oncol 2014; 134:523-6.
[Google Scholar]
|
Fulltext Views
3,265
PDF downloads
1,527





