Translate this page into:
Evaluation of functional impairment in psoriasis
2 Departments of Psychiatry, MIMER Medical College, Talegaon Dabhade, Maharashtra, India
3 Departments of Preventive and Social Medicine, MIMER Medical College, Talegaon Dabhade, Maharashtra, India
Correspondence Address:
Rohini Gaikwad
Department of Skin and STD, MIMER Medical College,Talegaon Dabhade, District Pune, Maharashtra 410507
India
| How to cite this article: Gaikwad R, Deshpande S, Raje S, Dhamdhere D V, Ghate M R. Evaluation of functional impairment in psoriasis. Indian J Dermatol Venereol Leprol 2006;72:37-40 |
Abstract
Background: Psoriasis is a chronic disease, the course of which is punctuated by exacerbations and remissions. The impact of a chronic, relapsing, and disfiguring disease such as psoriasis on occupational, social, and other areas of functioning is substantial and needs attention. Aim: The purpose of this study was to assess the level and nature of functional impairment in psoriasis. Methods: Forty-three consecutive patients attending the dermatology clinic of a rural hospital were studied for psychiatric comorbidity and the level of functioning, using a semistructured questionnaire. Results: Psoriasis affected social functioning of 48% patients, led to decreased work efficiency in 51.1%, and to subjective distress at work in 62.8% of patients. Stress in home environment and interpersonal relationships was reported by 69.8%. Social and occupational functioning worsened with increasing severity of psoriasis after 1-year duration of illness. Patients complaining of pruritis frequently had anxiety disorders. Psychiatric comorbidity was detected in 67.4% cases. Conclusion : Substantial proportion of patients suffered deterioration of functioning, especially with increasing duration of illness. Thus, timely attention by dermatologists is needed in order to limit the disability caused by psoriasis. To achieve this, liaison with psychiatrist would be crucial along with illness education and emotional support.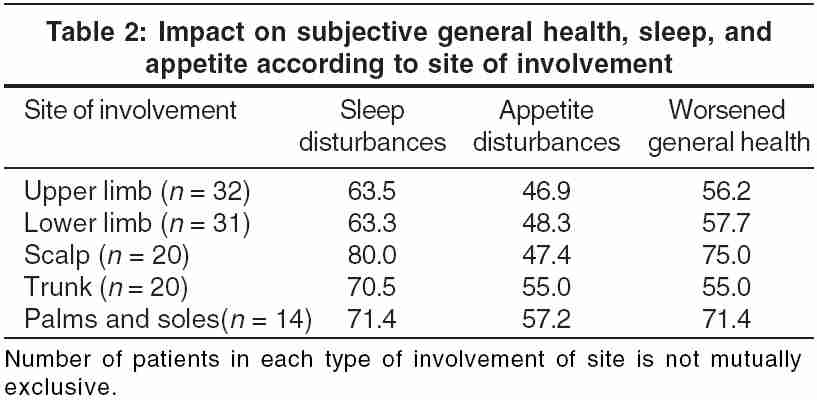
INTRODUCTION
The clinical impact of any medical illness is increasingly being assessed by the level of the patient′s well being and functioning.[1] Dermatological illnesses such as psoriasis often cause disfigurement, which further increase the suffering of the patient. The embarrassment, stigma, and social anxiety caused by the illness often lead to relational conflicts, emotional distancing, isolation, and depression, affecting the quality of life of a person.
This study was undertaken to assess the level and nature of the functional impairment in psoriasis. The role of stress in the exacerbation of psoriasis and triggering relapses has already been extensively studied. However, the functioning of patients in various spheres of life, such as physical and sexual functions, basic biological functions, social and occupational functions, and family relationships have been seldomly studied. Such assessment is likely to improve the insight of patients, which is also known to improve the prognosis in psoriasis.[2],[3],[4],[5]
METHODS
The objectives of the study were to assess the functioning of patients with psoriasis in various spheres of life and to diagnose comorbid psychiatric disorder. The sample consisted of consecutive patients suffering from psoriasis attending the dermatology clinic of a rural general hospital near Pune. The purpose of the study and questionnaire were explained to each patient and their verbal consent was obtained. Detailed dermatological examination and documentation of disease severity was done using psoriasis area severity index (PASI). Basic information about the illness, course, treatment details, family history, history of psychiatric problems, and impact of illness on various areas of occupational, familial, and relational functioning was recorded with the help of a semistructured questionnaire specially designed for the study by a dermatologist and a psychiatrist together. The questionnaire was prevalidated by the peer group.
This semi-structured questionnaire yielded a score of the functional level of these patients. Social and occupational functioning was assessed by social and occupational functioning assessment scale (SOFAS), whereas relational functioning was assessed by global assessment of relational functioning (GARF).[6] In these scales, functioning of an individual is considered on a continuum from excellent to grossly impaired functioning. It includes impairments owing to physical limitations, as well as owing to mental impairments. The GARF scale indicates the overall adjustment of a family or relationships on a hypothetical continuum ranging from competent optimal relational functioning to a disrupted, dysfunctional relationship within a range of 100-0.[7],[8] Statistical tools such as mean and standard deviation were used to summarize data. Analysis was done using nonparametric tests such as c[2]-test and indicators such as relative risk. Feedback regarding the nature of their illness and related problems was given to patients at the time of the interview, and the course and further plan of treatment was explained.
RESULTS
In all, 43 patients were included in the study, 27 from semiurban areas and 16 from adjacent rural areas. The sample included 27 males and 16 females aged 13-66 years. Out of these, 21% were unmarried. The occupational background showed that 37% were dependent, 12% were laborers, 16% had a small business, and 35% were in the service class. The educational background revealed 16.3% were illiterate, 34.9% were primary educated, 23.3% were secondary educated, 20.9% had completed a diploma, 2.3% were graduates, and 2.3% were postgraduates.
Their PASI scores ranged from 3.8 to 74 (mean = 42.1 ± 21). The mean SOFAS score was 66.6 ± 13 and the mean GARF score was 61.5 ± 13.7; the range for both was 40-90.
Impact of psoriasis on various spheres of functioning:
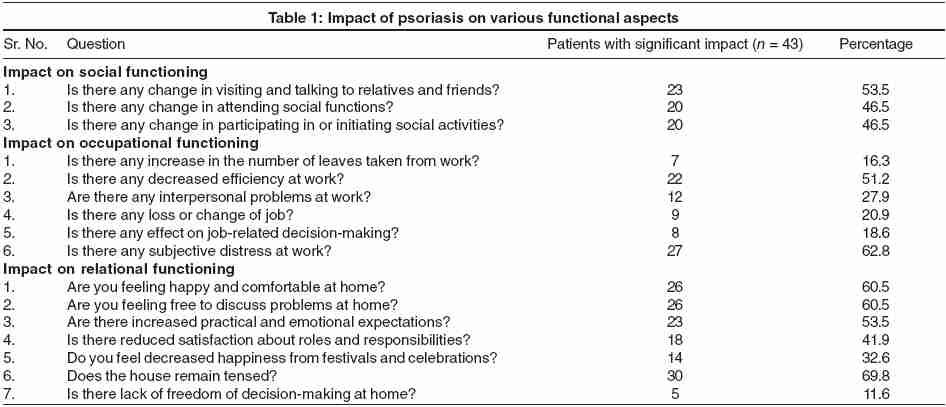
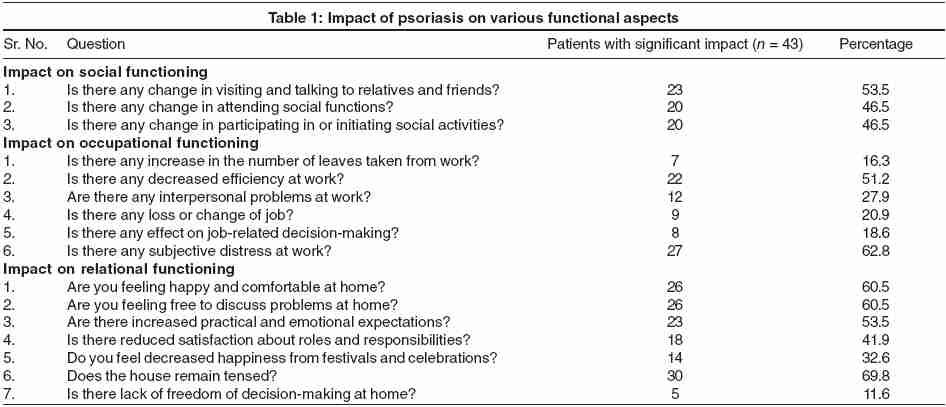
1. Social functioning: As shown in [Table - 1], social functions such as visiting and talking to relatives and friends were decreased in 51.5% of patients.
2. Occupational functioning: Subjective distress at work was reported by 62.8% of patients, followed by decreased efficiency at work by half of them [Table - 1].
3. Relational functioning: The relational functioning was maximally affected. The majority of patients (69.8%) mentioned that their house remained tense after the onset of the illness; 60.5% of patients also agreed that they were not feeling happy and comfortable at home and did not feel free to discuss their problems at home. Practical and emotional expectations from relatives also increased in half of the patients [Table - 1].
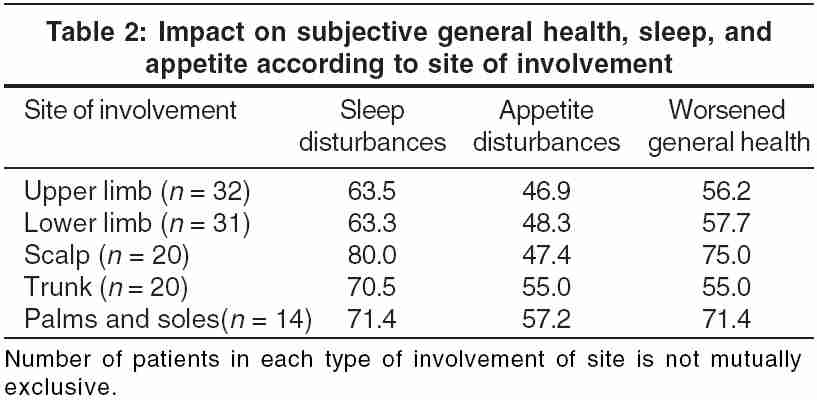
4. Impact on subjective general health, sleep, and appetite according to the site of involvement: Though some patients had extensive psoriasis, the maximum impact on the sleep, general health, and appetite was seen in patients who had lesions on exposed parts of the body. The sleep was most affected-67.4% of patients complained of sleep disturbances. Patients who had lesions on palms and soles and/or on the scalp had the maximum impact [Table - 2].
5. Impact on sexual functioning: Sexual dysfunction and/or effect on sexual life owing to psoriasis were reported by 9 out of 43 (20.9%) of the patients. None of these patients had lesions over the genitalia.
6. Pruritus and anxiety disorders: A statistically significant association was found between the presence of itching and the presence of anxiety and stress-related disorders. (Odd′s ratio = 4.25, c[2] = 5.05, p < 0.001.)
7. Psychiatric comorbidity in psoriasis: Other psychiatric disorders found were adjustment disorders (11 patients), conversion and somatoform disorders (2 patients), anxiety disorders (7 patients), depressive disorders (8 patients), and delusional disorder (1 patient).
Correlations of various sociodemographic factors, illness-related variables, and various factors related to psychopathology were studied. The age and sex of the patient had no statistically significant correlation with the psychiatric problems or the severity of the illness. With increasing PASI score, the score of GARF scale decreased for females, but not for males. This negative correlation was statistically significant ( p < 0.05). With an increase in the duration of illness, relational functioning decreased significantly as the PASI increased. It was statistically significant for males after 3-year duration of illness. A strongly negative correlation between PASI and SOFAS score was noted after 1-year duration of illness. It increased with the duration of the illness. It was similar in males and females. The level of anxiety in these patients as measured by the Hamilton anxiety rating scale increased with the PASI score but only after 5 years of illness. Other sociodemographic factors did not correlate with the severity of illness or psychiatric problems.
DISCUSSION
Psoriasis patients reacting to stress function less well in terms of mental health and experience more disabilities in everyday life.[9] Significant levels of anxiety and depression have been reported in patients with psoriasis in Indian as well as international studies.[10],[11] In our study, 29 out of 43 patients suffered from such problems. But the impact on various spheres of functioning was greater. An increasing PASI score caused worsening of social and occupational functioning, especially when the duration of illness was more than 1 year. The relational functioning was affected more in females than in males with increasing PASI scores and duration of illness. This could be owing to greater emotional sensitivity and familial involvement in females, but needs to be studied further.
Sleep disturbance was found in 29 (67.4%) patients. This was consistent with the results of other studies.[12] Qualitative accounts given by the patients revealed that it was not only owing to dermatological or psychiatric illness, but stigma, shame, guilt, and various illness-related fears were contributory. Although none of the patients had lesions over the genitalia, 9 out of 43 (20.9%) patients reported sexual dysfunction and/or an effect on their sexual life.
A statistically significant association was found between pruritus and anxiety. This finding appears to be clinically relevant in detecting anxious psoriasis patients (relative risk = 2.06). Pruritus is known to play an important role in exacerbating psoriasis.[11] The degree of pruritus has been correlated with depression in one study.[13] In a cross-sectional interview, psychiatric morbidity was detected in 29 patients. There is a need for timely identification and appropriate management of psychiatric disorders in everyday dermatology practice.[14]
Better understanding and communication between psoriasis patients and their physicians may help to improve clinical outcomes in psoriasis.[15] Helping the patient with psoriasis to learn to live with the condition is challenging but important for a dermatologist.[16]
In our study, up to two-thirds of patients with psoriasis suffered from functional impairment. It would be important to limit this impairment in order to help patients with this chronic illness. Clinical parameters such as the presence of pruritus, prolonged duration of illness, and a high PASI score should direct the clinician to detect functional impairment such as subjective distress experienced by the patient at work and at home, interpersonal difficulties, restrictions in social life, sleep and appetite disturbances, and deterioration of general health. The patient′s functioning and his familial relationships are important and should be preserved throughout the course of illness. This would reduce the psychosocial difficulties faced by the patient and improve his compliance as well as satisfaction with the treatment. To achieve this, liaison with a psychiatrist would be crucial along with illness education and emotional support[17].
| 1. |
Wells KB, Stewart A, Hays RD, Burnam MA, William R, Daniels M, et al . The functioning and well being of depressed patients. JAMA 1989;262:914-9.
[Google Scholar]
|
| 2. |
Seville RH. Psoriasis and stress. Br J Dermatol 1977;97:297-302.
[Google Scholar]
|
| 3. |
Seville RH. Psoriasis and stress II. Br J Dermatol 1978;98:151-3.
[Google Scholar]
|
| 4. |
Finlay AY, Khan GK, Luscombe DK, Salek MS. Validation of sickness impact profile and psoriasis disability index in psoriasis. Br J Dermatol 1990;123:751-6.
[Google Scholar]
|
| 5. |
Finlay AY, Coles EC. The effect of severe psoriasis on the quality of life of 369 patients. Br J Dermatol 1995;32:236-44.
[Google Scholar]
|
| 6. |
Goldman HH, Skodol AE, Lave TR. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psych 1992;149:1148-56.
[Google Scholar]
|
| 7. |
Kaplan HI, Sadock BJ, editors. Kaplan and Sadock's synopsis of psychiatry, behavioural science, clinical psychiatry. 8th ed. Maryland: Williams and Wilkins; 2001.
[Google Scholar]
|
| 8. |
Schrader G, Gordon M, Harcourt R. The usefulness of DSM-III: axis IV and axis V assessments. Am J Psych 1986;143:904-7.
[Google Scholar]
|
| 9. |
Fortune DG, Main CJ, O'Sullivan TM, Griffiths CE. Quality of life in patients with psoriasis: the contribution of clinical variables and psoriasis specific stress. Br J Dermatol 1997;137:755-60.
[Google Scholar]
|
| 10. |
Patil A, Sharma S, Dhavale HS. Coping with psoriasis: need for consultation-liaison. Indian J Dermatol 2002;47:143-6.
[Google Scholar]
|
| 11. |
Fried RG, Friedman S, Paradis C Hatch M, Lynfield Y, Duncanson C, et al . Trivial or terrible? The psychological impact of psoriasis. Int J Dermatol 1995;34:101-5.
[Google Scholar]
|
| 12. |
Sharma N, Koranne RV, Singh RK. Psychiatric morbidity in psoriasis and vitiligo-a comparative study. J Dermatol 2001;28:419-23.
[Google Scholar]
|
| 13. |
Gupta MA, Gupta AK, Kirby S, Weiner HK, Mace TM, Schork NJ, et al . Pruritis in psoriasis: a prospective study of some psychiatric and dermatological correlates. Arch Dermatol 1998;124:1052-7.
[Google Scholar]
|
| 14. |
Renzi C, Picardi A, Abeni D, Agostini E, Baliva G, Pasquini P, et al . Association of dissatisfaction with care and psychiatric morbidity with poor treatment compliance. Arch Dermatol 2002;138:337-42.
[Google Scholar]
|
| 15. |
Krueger G, Koo J, Lebwohl M, Menter A, Stern RS, Rolstad T. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient - membership survey. Arch Dermatol 2001;137:280-4.
[Google Scholar]
|
| 16. |
Ramsay B, O'Reagan M. A survey of social and psychological effect of psoriasis. Br J Dermatol 1988;118:195-201.
[Google Scholar]
|
| 17. |
Spiegel David. Healing words: emotional expression and disease outcome. JAMA 1999;281:1328-9.
[Google Scholar]
|
Fulltext Views
1,764
PDF downloads
1,296





