Translate this page into:
Evaluation of leprosy patients with 1 to 5 skin lesions with relevance to their grouping into paucibacillary or multibacillary disease
2 Leprosy Temporary Hospitalization Ward (THW), Gandhi Hospital, Secunderabad, India
3 BPRC- LEPRA India, Hyderabad, India
Correspondence Address:
P Narasimha Rao
B-48, Income tax colony, Mehdipatnam, Hyderabad - 500 028, AP
India
| How to cite this article: Rao P N, Pratap D, Ramana Reddy A V, Sujai S. Evaluation of leprosy patients with 1 to 5 skin lesions with relevance to their grouping into paucibacillary or multibacillary disease. Indian J Dermatol Venereol Leprol 2006;72:207-210 |
Abstract
Background: Patients with 1 to 5 skin lesions are arbitrarily categorized as belonging to the paucibacillary (PB) group for treatment purposes. With the decreasing prevalence of leprosy in India and modifications in leprosy program, the relevance of this grouping needs further study. Aims: To study a group of leprosy patients with 1 to 5 skin lesions and compare the clinical parameters with histopathological findings and bacteriological status of the skin and nerve to evaluate the relevance of this grouping. Methods: Seventy seven patients of leprosy with 1 to 5 skin lesions were included in the study. The number of skin lesions was recorded. Slit skin smears (SSS) and skin biopsies were taken in all patients and nerve biopsy was performed in 19 of them. The biopsies were evaluated for the type of pathology and AFB status. Results: In these 77 patients (single skin lesions, 42; two lesions, 18; three lesions, 10; four lesions, 5; and five lesions, 2 patients) the clinical classification was indeterminate leprosy (IL) in 4, tuberculoid leprosy (TT) in 4 patients and borderline tuberculoid leprosy (BT) in 69 patients. Skin smears were positive only in 1 patient. The histological diagnoses in the skin were IL in 13, TT in 3, BT in 48 and borderline lepromatous (BL) in 4 patients. Acid-fast bacilli (AFB) were found in 14 out of 77 skin biopsies. Of the 19 nerve biopsies, 17 showed histological features of BT leprosy; of these, 12 demonstrated AFB on Fite staining. The bacillary index of granuloma (BIG) ranged from 1+ to 2+. The clinico-histopathogical correlation was 63% in the BT group, with 4 patients of this group showing features of BL on histopathology. When the presence of AFB was assessed, the percentage of positivity was 1.3% in SSS, 18% in skin biopsies and 63% in nerve biopsies. Conclusion: Our results point to the non-homogeneous nature of this group of leprosy patients with 1 to 5 skin lesions, with varied bacteriological and histopathological features. The significance of MB type findings on histopathology in patients grouped as PB leprosy should be resolved so that these patients may be given the drug therapy and the duration of therapy they warrant.



Introduction
Leprosy patients with 1 to 5 skin lesions are considered as belonging to the paucibacillary (PB) group for treatment purposes without taking into account the size and extent of lesions or the number of nerves involved; the clinical classification of leprosy is not considered relevant. They are uniformly treated with paucibacillary multidrug therapy (MDT-PB) for a fixed duration of 6 months as per the WHO recommendations, after ROM (rifampicin, ofloxacin and minocycline) therapy was discontinued for single skin lesion leprosy patients. Although this grouping is convenient for administrative and field purposes, this group potentially consists of patients with diverse clinical, bacteriological and histopathological features. A slit skin smear examination is not performed in these patients as it is not considered an essential laboratory test in leprosy programmes. This categorization of leprosy based on the number of skin lesions for treatment purposes is arbitrary and is purely for the convenience of field workers.
In 1998 the WHO expert committee on leprosy proposed MDT-PB for leprosy patients with 1 to 5 skin lesions but did not mention any scientific basis for such a recommendation except citing the non-reliability of skin smear services,[1] which were considered relevant till then.
There has been a substantial decrease in the numbers of leprosy patients after the implementation of MDT for leprosy. In the National Leprosy Elimination Programme in India, the proportion of multibacillary (MB) cases was seen to increase in states heading towards elimination.[2],[3] However, this increase was marginal as PB cases still account for more than 60% of the leprosy cases in India in the year 2004. Study of this PB group for variations and patterns is not only important in the present context but also relevant in devising future strategies in leprosy control programs. In the present study, we analyzed the clinical, bacteriological and histopathological features of this group of patients based on detailed clinical examination, skin smear findings and skin and nerve histopathology.
Methods
Seventy-seven patients of leprosy (male 57 and female 20) with 1 to 5 skin lesions attending the Department of Dermatology, Osmania General Hospital, Hyderabad and Gandhi Hospital. Secunderabad India, between 1999 and 2003 were included in this retrospective study. Clinical findings were recorded in a specially prepared case sheet. The diagnosis of leprosy was based on the presence of hypopigmented, hypoesthetic skin lesions and cutaneous and/or peripheral nerve thickening. The clinical features, morphology and number of lesions were recorded. Patients with reactions were excluded from the study.
Slit skin smears and skin biopsy were performed on the most representative lesion in all patients. A nerve biopsy was performed in 19 patients on a pure sensory nerve, either the sural nerve or the radial cutaneous nerve. The specimens were stained with Haematoxylin and Eosin (H and E) and modified Fite stains. The sections were reviewed by a pathologist who was blinded to the clinical details. The type and character of granuloma and presence of acid fast bacilli (AFB) were noted. The bacillary index of the granuloma (BIG) was calculated in the tissue biopsy specimen.
Results
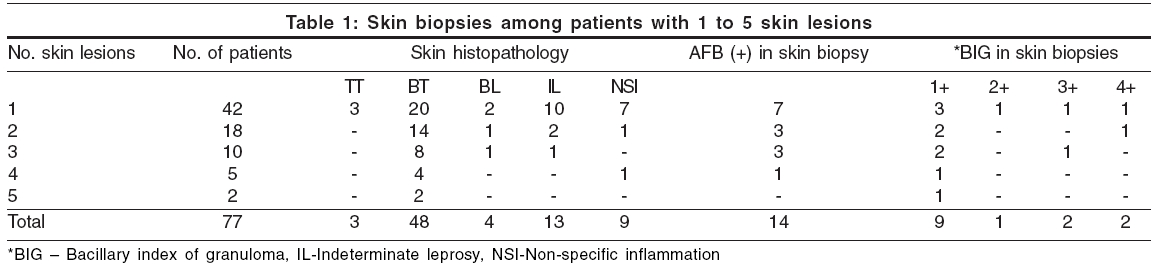
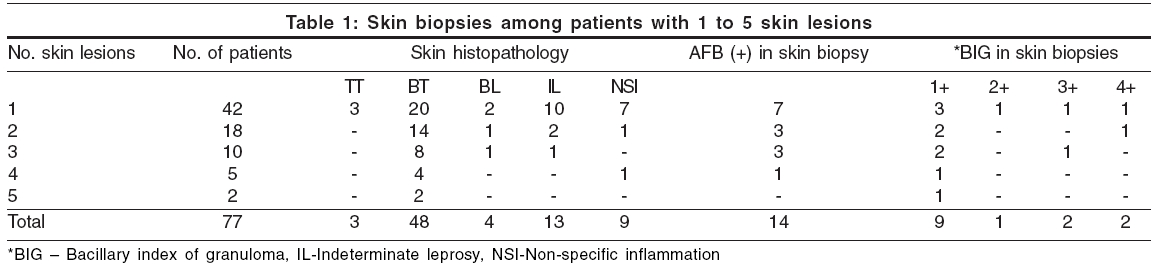
Of the 77 patients [Table - 1][Table - 2], 42 had a single skin lesion of leprosy, 18 had two, 10 had three, five had four and two had five skin lesions. Their clinical classification was indeterminate leprosy (IL) in four patients, tuberculoid leprosy (TT) in four patients and borderline tuberculoid leprosy (BT) in 69 patients. Slit skin smear for AFB was positive in only one patient, who had BT leprosy.
The histopathological findings of H and E stained skin biopsies were as follows: IL in 13 patients, TT in 3 patients, BT in 48 patients, non-specific infiltrates in 9 patients and borderline lepromatous (BL) leprosy in four patients. The BIG values on modified Fite stain were 3+ or more in all four patients who showed features of BL on histopathology and were clinically diagnosed as BT. Two of them presented with a single skin lesion. However, slit skin smears were negative in all these patients. Skin biopsies in 14 out of the 77 patients demonstrated AFB, with the BIG ranging from 1+ to 4+.
Out of 19 nerve biopsies, 17 showed histopathological features of BT leprosy and 2 showed nonspecific infiltrates. Of the 17 nerve biopsies showing features of BT leprosy, 12 were positive for AFB, their BIG ranging from 1+ to 2+.
In the BT group, 43 out of 69 patients showed concordance, i.e. clinico-histopathogical correlation was 62% [Table - 3]. Four patients in this group demonstrated histopathological features of BL in skin biopsies and 13 patients showed features of indeterminate leprosy. Good concordance (75%) was observed in four patients of the TT group.
The percentage of positivity of AFB was 1.3% in SSS, 18% in skin biopsies and 63% in nerve biopsies.
Discussion
Leprosy patients with 1 to 5 skin lesions are grouped together for treatment purposes, but we found that they presented with varied clinical and histopathological features, pointing to the non-homogeneous nature of this group. AFB were more abundant in skin and nerve biopsies than in SSS examinations. Four patients with clinical features of BT leprosy had features of BL leprosy on histopathology and BIG values of 3+ or more in their skin biopsies. Nerve biopsies of leprosy patients are known to demonstrate AFB more readily and abundantly than skin biopsies,[4] but we could not perform a nerve biopsy in these patients because there was no involvement of a pure sensory nerve. We found that nerve biopsies demonstrated AFB more frequently than skin biopsies (63% vs. 18%).
The significance of our observations is that patients with 1 to 5 skin lesions, which are grouped together for treatment purposes do not have disease of similar severity. Skin histopathology revealed the MB type of leprosy in a few of them and high bacterial indices were present in the skin and nerve biopsies of some patients. It is known that clinical features in leprosy patients reflect only the gross morphology of the underlying pathological changes. Significant discrepancies have been reported between the bacteriological and immunological status of the nerve and skin compared to the clinical diagnosis.[5],[6],[7] These features should also be considered while establishing treatment programs for leprosy.[8]
Over the years, some procedures in the strategy of leprosy elimination programs have been simplified, particularly in many aspects of MDT regimens (e.g. rules for classification of patients, use of skin smears, post-MDT surveillance, etc). In some instances, these changes merely reflected simplifications in working methods that had been implemented by field staff lacking certain skills. For example, skin smears examinations were regarded as extremely important during the 1980s, but unnecessary by the late 1990s.[9] However, in this case the program managers did not consider those centers that have facilities for systematic investigations of leprosy patients and have not formulated any guidelines as to how to make use of these facilities in providing appropriate treatment.
It has been observed that a few borderline tuberculoid patients harbor AFB in their nerves for many years, even though they become clinically inactive, following MDT.[10] Explanation for this could lie in defective macrophage function. The important macrophage function, its bacteria-clearing capacity within a lepromin-induced granuloma, is not invariably present in all tuberculoid and indeterminate leprosy patients.[11]
These reports point to the importance of treating PB leprosy with as much attention as MB patients, if not more. The definition of PB leprosy has been evolving over the last two decades, with an increasing number of erstwhile PB patients being included in the MB group for treatment purposes. This is one of the important reasons for the progressive shrinking of the pool of PB cases all over the world. With a further reduction in the number of PB cases, the proposal of uniform MDT (U-MDT) for patients of leprosy could become practical,[12] albeit with certain modifications, as the separation of patients into PB and MB groups for treatment purposes is purely arbitrary.
With a substantial decrease in the numbers of leprosy patients, the workload and financial burden on leprosy program/organizations has significantly decreased over the years. Hence, slit skin smears may again be made an integral part of the leprosy program. Tissue biopsy findings, which are not considered relevant for treatment purposes until now, could be given a status in the categorization and assessment of severity of the disease.[13] The significance of the findings of abundant AFB and histopathology of the MB type of leprosy in tissue biopsies, in patients grouped as PB leprosy should be resolved so that these patients could be given the drug therapy and duration of therapy they warrant. Such techniques that directly evaluate the type and severity of leprosy, when made relevant to the treatment, will provide therapy based on firm scientific parameters, especially in centers where they are available.
| 1. |
WHO expert committee on leprosy, seventh report, WHO technical report series. WHO: Geneva; 1998. p. 874.
[Google Scholar]
|
| 2. |
Mahajan VK, Sharma NL Rana, P Sood N. Trends in detection of new leprosy cases at two centres in Himachal Pradesh, India: a ten-year study. Indian J Lepr 2003;75:17-24.
[Google Scholar]
|
| 3. |
National Leprosy Eradication Programme Chattisgarh. Directorate of Health services (Leprosy cell.) Status report: 2004.
[Google Scholar]
|
| 4. |
Lakshmi TS, Rao PN, Krishna AV, Kumar SV. Histopathology of skin and nerve and clinical classification of leprosy patients. Indian J lepr 1996;68:258-60.
[Google Scholar]
|
| 5. |
Kar PK, Arora PN, Ramasastry CV, Sayal SK, Dhaka RS. A clinical and pathological study of macular lesions in leprosy. Indian J Lepr 1994;66:435-42.
[Google Scholar]
|
| 6. |
Shenoi SD, Siddappa K. Correlation of clinical and histopathologic features in untreated macular lesions of leprosy-a study of 100 cases. Indian J Lepr 1988;60:202-6.
[Google Scholar]
|
| 7. |
Mukherjee A, Misra RS. Comparative histology of skin and nerve granulomas in leprosy patients. Lepr Rev 1988;59:177-80.
[Google Scholar]
|
| 8. |
Nilsen R, Mengistu G, Reddy BB. The role of nerve biopsies in diagnosis and management of leprosy. Lepr Rev 1989;60:28-32.
[Google Scholar]
|
| 9. |
Sansarricq H. Lessons learnt. In : Multi drug therapy for leprosy - Development and implementation over the past 25 years. World health organization: Geneva; 2004.
[Google Scholar]
|
| 10. |
Shetty VP, Suchitra K, Uplekar MW, Antia NH. Persistence of Mycobacterium leprae in peripheral nerves as compared to skin in multidrug treated leprosy patients. Lepr Rev 1992;63:329-36
[Google Scholar]
|
| 11. |
Chaudhuri S, Hajra SK, Mukherjee A, Saha B, Mazumder B, Chattapadhya, et al . Why relapse occurs in PB leprosy patients after adequate MDT despite they are Mitsuda reactive: lessons form Convit's experiment on bacteria-clearing capacity of lepromin-induced granuloma. Int J Lepr Other Mycobact Dis 1998;66:182-9.
[Google Scholar]
|
| 12. |
U-MDT. In : Report on the third meeting of the WHO technical advisory group on elimination of leprosy. Brasillia, World health organization: Geneva; 2002.
[Google Scholar]
|
| 13. |
Srinivas D, Rao PN, Lakshmi TS, Suneetha S. Bacterial index of granuloma and its relevance compared to BI of skin smears. Lepr Rev 2002;73:79-80.
[Google Scholar]
|
Fulltext Views
1,817
PDF downloads
739





