Translate this page into:
Evolution of venereology in India
Correspondence Address:
Devinder Mohan Thappa
Department of Dermatology and STD, JIPMER, Pondicherry- 605 006
India
| How to cite this article: Thappa DM. Evolution of venereology in India. Indian J Dermatol Venereol Leprol 2006;72:187-196 |
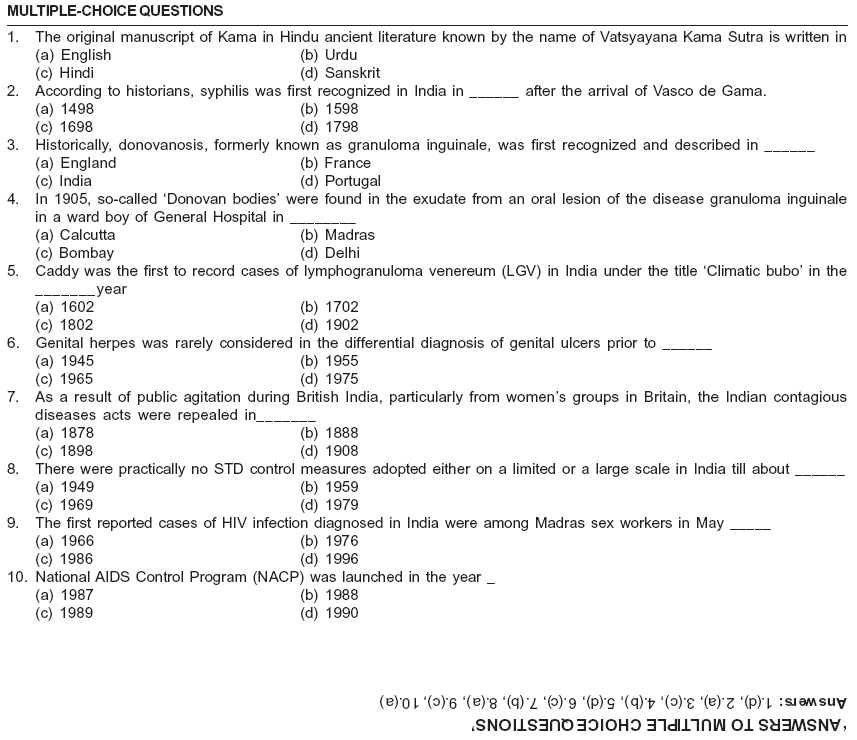
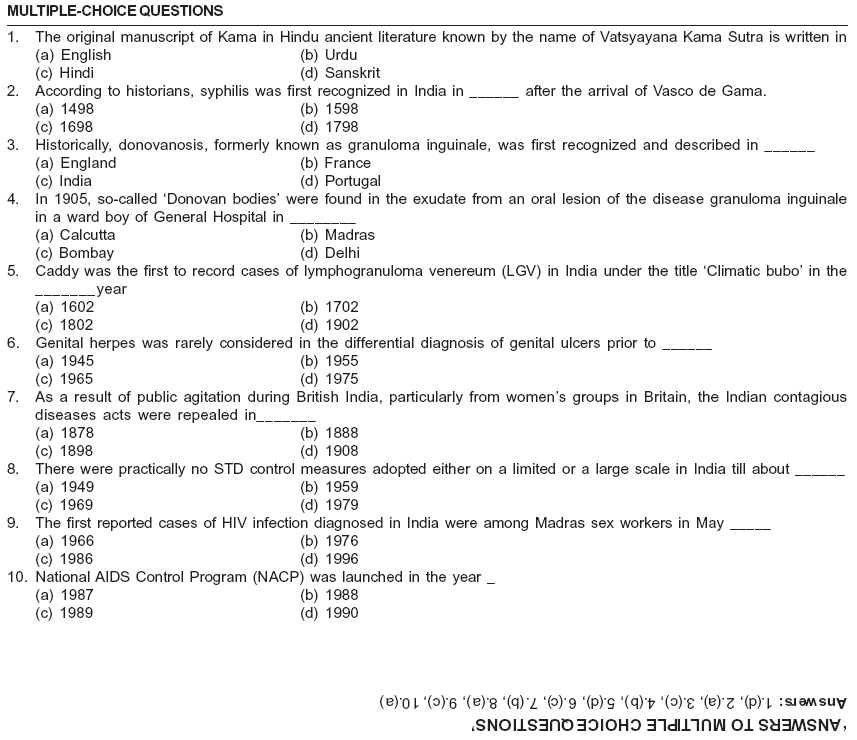
The older terminology of ′venereal diseases′ (VDs) largely has been superseded in the past 50 years by ′sexually transmitted diseases′ (STDs) and more recently by ′sexually transmitted infections′ (STIs).[1] To some, venereal diseases came to be viewed as a narrow and pejorative term limited to gonorrhea, syphilis, chancroid, lymphogranuloma venereum and granuloma inguinale and related VD control laws. The term ′sexually transmitted diseases′ more easily incorporates the many newly discovered sexually transmitted agents and syndromes.[1],[2] Sexually transmitted disease (STD) includes diseases that are transmitted by sexual intercourse. Sexual transmission requires the agent to be present in one partner, the other partner to be susceptible to infection with that agent and that the sex partners engage in sexual practices that can transmit the pathogen. Sexually transmitted infection (STI) differs from sexually transmitted disease (STD) in that STD conventionally includes infections resulting in clinical diseases that may involve the genitalia and other parts of the body participating in sexual interaction, e.g., syphilis, gonorrhea, chancroid, donovanosis, nongonococcal urethritis, genital warts, herpes genitalis, etc. STI, in addition, includes infections that may not cause clinical disease of genitals but are transmitted by sexual interaction, e.g. all STDs and hepatitis B, HIV, HTLV-1, etc. Nowadays, the term STI is preferred, since it covers all the diseases that can be transmitted by sexual intercourse. However, for all practical purposes, both STI and STD are used synonymously and in European countries, they come under the specialty of genitourinary medicine.[3]
Venereology (the study of venereal diseases) today encompasses more than the five classical venereal diseases (syphilis, gonorrhea, chancroid, donovanosis and lymphogranuloma venereum).[4] A growing number of other diseases are being identified that might be considered the new generation of sexually transmitted diseases (STDs). Their importance is newly recognized due to the development of laboratory techniques of diagnosis and increasing awareness of the consequences of STDs in areas of health and society.[4] This article briefly deals with various facets of evolution of venereology in India.
Origin of STDS
The origins of venereal (sexually transmitted) diseases are obscure.[2] Medical and other historians have often suggested that well-known diseases such as syphilis, gonorrhea, chancroid and lymphogranuloma venereum have existed since earliest times. This may or may not be true and some of these individuals may have drawn conclusions from ancient texts and manuscripts that may not be accurate. While the infections certainly exist in Homo sapiens , did they occur in the preceding species Homo erectus prior to 150,000 BC? No one knows, but the French philosopher Voltaire summed it up well when he declared in his Dictionnaire philosophique that venereal diseases are like the fine arts - it is pointless to ask who invented them.[2] Among the uneducated and uninformed people in India, we often hear remarks to the effect that the occurrence of venereal disease is a ′visitation from God,′ ′a sign of growing adolescence,′ ′a sign of maturity,′ ′the result of eating nettle leaves′ and ′from sexual intercourse with menstruating woman′.[5] Such fallacious ideas about the causation of venereal diseases are still prevalent all over the world with varying emphasis.
In the field of medicine, the ancient Hindus carried their researches farther than any of their contemporaries.[6] The Upanishads contain the most convincing evidence of their passion for enquiry into the nature of things. Padmini, or the Lotus woman, is the symbol of woman beauty in Hindu literature.[6] According to Hindu mythology, in the beginning, the Lord of Beings (Brahma) created men and women and laid down rules for regulating their existence with regard to Dharma (acquisition of religious merit), Artha (acquisition of wealth, property, etc.) and Kama (love, pleasure and sensual gratification).[6] The commandments related to Kama were expounded by Nandi, the follower of Mahadeva. This document written by Nandi, known as Kama Sutra (aphorisms on love), was transformed into a small volume of Sanskrit literature by Vatsyayana between the 1st and 6th century of the Christian era. This manuscript is known by the name of Vatsyayana Kama Sutra. This document was withheld from public gaze as sex was considered a taboo amongst Hindus. This Sanskrit document was later translated into English by Sir Richard Burton and F. F. Arbuthanot and was published in England in 1883. There is no mention of venereology in the days of Kama Sutra.[6]
Syphilis
In the past, some attempts have been made to identify syphilis and gonorrhea in ancient Hindu (Ayurvedic) texts, but evidence strongly suggests that syphilis, at least, was unknown in India before the early 16th century.[7] So explosive was the nature of epidemic in this region during that time and so deep was the cultural and national impact that various religious/cultural communities started blaming each other as the source.[5],[8] Careful examination of available records shows that Charaka and Sushruta, two ancient ayurvedic physicians, did not know anything about syphilis.[5] However, Bloomfield, Hirsch, Hessler and other Orientalists have suggested that syphilis was prevalent in ancient India.[5] Some of the first references to the disease and its treatment are to be found in the Bhavaprakasa, a mid-sixteenth-century text, reputedly the work of Bhavamisra, an Ayurvedic physician at Benares. During that period and subsequently for a long time, syphilis was known in India as the Portuguese disease, or firanga or firangi roga, terms that identified it with the firangis (′Franks′), or Europeans.[5],[7] According to historians, the disease was first recognized in India in 1498 after the arrival of Vasco de Gama, who had left Portugal in 1497. It seems probable that the Portuguese introduced the disease to India from Europe in the early 16th century.[5] The researches of Okamura in Japan, Susuki in China and Jolly and others in India show that syphilis was introduced into this country from Europe.[5] By the early 19th century, when the British had gained ascendancy over a large part of the subcontinent, syphilis was already widely disseminated, though the extent of its incidence can only be guessed at.[7]
Gonorrhea
Authentic records of gonorrhea in India can only be found during the British Empire in India. During British Raj, in official statistics of the army, venereal diseases like syphilis, gonorrhea and soft chancre (now called as chancroid) figured.[9] In regiments of the British army stationed in India, the percentage of troops admitted to hospital with venereal diseases (identified in almost equal proportion as primary syphilis and gonorrhea) rose to 205 per 1,000 in 1875 and peaked at 522 per 1,000 in 1895.[7] For unexplained reasons, syphilis was relatively more common and gonorrhea less common in the army personnel of Indian origin than in the British army in India.[9]
Chancroid
Chancroid, one of the five classic venereal diseases, was first described by Brassereau in 1852 in France.[10] The venereal diseases in the British Army were regarded as comprising of syphilis, gonorrhea and soft chancre, but it was decided to ignore the last named as not of public health importance in the run-up to the Royal Commission of 1916.[11] In the Army in India (71,001 men), the venereal disease rate in the year 1912 was 55.5 per 1,000 (10.1% of all admissions). In the army at home, in India, the total venereal disease rate of 56.5 per 1,000 consisted of 18.7 for primary and secondary syphilis, 29.5 for gonorrhea and 8.3 for soft sore .[11]
Donovanosis
Historically, donovanosis, formerly called as granuloma inguinale, was first recognized and described in India. It was first described in 1881 in Madras, India, under the name of ′serpiginous ulcer′ by Kenneth MacLeod, a Scot, who joined the Indian Medical Service and became professor of surgery in Calcutta.[12] Cause of it was found by Colonel Charles Donovan.[11] In 1905, he described the intracellular bodies, which bear his name and was the co-discoverer of the etiological agent in kala-azar.[13],[14] So-called ′Donovan bodies′ were found in the exudate from an oral lesion of the disease in a ward boy of General Hospital in Madras. The nature of these was disputed from the beginning. Donovan himself thought that they were protozoa. It was not until 1943 that it was clearly shown that the ′Donovan bodies′ were bacterial in nature.[15] The natural history of donovanosis and its probable venereal nature was subsequently elucidated by others.[14],[16]
Lymphogranuloma venereum
In 1902, Caddy was the first to record cases of lymphogranuloma venereum (LGV) in India under the title ′Climatic bubo′.[17] At the Institute of Venereology in Madras, 3,884 cases of LGV were diagnosed between 1968 and 1977, accounting for 6% of STD cases seen in the same period.[18] Towards the end of the 19th century, most authors in India held the opinion that disease was due to climatic influences (mainly tropical) and consequently, many textbooks today still refer to LGV as ′Climatic bubo′.[19],[20]
Other STDS
However, no description of genital warts, herpes genitalis and trichomoniasis is found in the comparatively modern Indian literature of the early 20th century.[4] Despite considerable doubt by most observers, by 1920s and 1930s many venereologists had concluded that genital warts are sexually transmitted diseases.[2] Genital herpes was rarely considered in the differential diagnosis of genital ulcers prior to 1965.[21] It was only in 1966 that herpes genitalis was recognized as a venereal disease. At present, it is the most common STD in some of the STD clinics in India.[4] Donne first described the protozoal organism Trichomonas vaginalis in 1836,[22] which he observed in purulent genital secretions from both men and women. Microbiological investigations of chlamydial infections began in 1907 when Halberstaedter and Prowazek detected intracytoplasmic chlamydial inclusions in the conjunctival scrapings of nonhuman primates that were experimentally infected with material collected from the conjunctiva of patients with active trachoma. Similar inclusions were later demonstrated in conjunctival cells of trachomatous patients, in scrapings from the conjunctiva of the eyes of babies with ophthalmia neonatorum, from the endocervix of mothers of these babies and from the urethra of patients with bacterial urethritis. In a study published in 2000, among 319 women with vaginal discharge attending a reproductive health clinic in New Delhi, India, the most common infection was bacterial vaginosis (26%).[23] At least one sexually transmitted infection was detected in 21.9% of women. The prevalence of C. trachomatis infection was 12.2%, trichomoniasis 10% and syphilis 2.2%.[23]
British India and STD control measures
In 19th century India, the British military authorities did not rely solely upon mercury to try to deal with STDs, especially syphilis, in the army (mainly contracted from prostitutes).[7] From about the 1780s onwards, lock hospitals were used to confine and treat prostitutes associated with the army and found to be suffering from STDs.[9] There was no specialist venereologist in India before 1910; but there was an army adviser who laid down treatment schedules and special wards were provided for difficult cases in military hospitals in Britain.[9]
During the 19th century, attempts to control STDs centered on the control of prostitutes.[9] The authorities′ concern related entirely to the effect of STDs on the army and the prostitutes associating with it. The Contagious Diseases Acts were promulgated between 1864 and 1869.[9] They ensured that in garrison towns and major ports, women named to the police as prostitutes had to undergo a regular medical examination. If found to be infected, they were confined to a lock hospital for up to 3 months for treatment, after which they were regarded as cured. The sole object was to protect soldiers. Indian prostitutes were segregated in special enclosures called ′chaklas′ within the cantonments where there was usually a lock hospital. A prostitute wishing to take up residence in a ′chakla′ had to apply for permission to be placed on the register of prostitutes. Registered prostitutes in ′chaklas′ were called ′Lal Kurti,′ ′queen′s ladies.′ The ′chaklas′ were supervised by ′mahaldarnis,′ appointed by the government. They were required to control them and also act as pimps and provide women for the use of soldiers at the request of their commanding officers.[9] There were scanty data on the extent of STDs in the civilian population.[7] A report on Jafer Suleman Dispensary for women and children in Bombay by the pioneer woman doctor Edith Pechey recorded that among the 2,817 patients examined in the second half of 1884, 74 women and 23 children were suffering from syphilis; 55 had gonorrhea.[24]
As a result of public agitation, particularly from women′s groups in Britain, the Indian Contagious Diseases Acts were repealed in 1888.[9] Traditionally, the military authorities had accepted that an outlet for their soldiers′ sexual energy was essential. However, the army was not prepared to abandon all controls over the army prostitution and through a series of cantonment acts from 1889 onwards, it retained many of the formally renounced measures of the previous year (like registration and licensing of prostitutes, the old rigid lock hospital system).[7],[9] Provision of women - registered, inspected and available - was seen as a preferable alternative to masturbation or particularly homosexuality, which was dreaded.[9] But the women had to be presentable.
M. I. Balfour, a leading member of the Women′s Medical Service, remarked in 1924 on the basis of 30 years′ work in India that STDs were responsible for ′much of the gynecological disease which fills our women′s hospitals and also no doubt for much of the high rate of infant mortality and the many miscarriages and stillbirths.′[25] The extent of STDs just before independence can be gauged from the report of Sir John Megaw, Director-General of the Indian Medical Services.[26] His survey in 1933 recorded 37 cases of syphilis and gonorrhea for every 1,000 cases attending hospitals and clinic; it was also estimated that there were as many as 5.5 million cases of syphilis and 7.5 million of gonorrhea in India at that time.
Independent India and STD control measures
There were practically no control measures adopted either on a limited or a large scale in India until about 1949.[5] At the request of the Government of India (GoI), World Health Organization (WHO) sent a venereal disease demonstration team in 1949 to work side by side with a national matching team to establish a center for a survey and mass treatment of syphilis in Himachal Pradesh in India. The Venereal Disease (VD) Main Clinic and Laboratory at Shimla, in Himachal Pradesh, was established in May 1949. This is one of the states to have a full-time venereologist in control of a state VD organization. Subsequently, more VD clinics were established in Himachal Pradesh in the next 2-3 years. As a consequence of this, the percentage of seropositivity for syphilis was brought down from 40-45% in 1949-1951 to 18% by 1959.[5]
The WHO VD demonstration team in Himachal Pradesh trained medical and paramedical personnel from different states in India and South East Asia region.[5] This team was withdrawn in December 1951, but as a result of the efforts of trained personnel in other states in India, in 1953 alone, about 1,00,000 new cases of syphilis were identified and treated. In view of the prevailing high incidence of venereal diseases in the country, the Directorate General of Health Services (DGHS) in the Ministry of Health of Government of India (GoI) included certain measures for VD control in the first Five Year Plan.[5],[7] A full-scale VD organization came into existence in Himachal Pradesh. A VD training and demonstration center was established in New Delhi. The VD department of the Government General Hospital, Madras, was upgraded to a postgraduate training center in 1952. Measures were taken to make India self-sufficient in the production of cardiolipin antigen and penicillin.[5]
In the second Five Year Plan, greater emphasis was laid on the problem of venereal diseases than was done in the past.[5] On the advice of the health panel of the planning commission, the GoI, with state governments, made a provision for a central VD organization, strengthening of state VD organizations, setting up of 8 VD clinics and laboratories at the headquarters of states, 75 clinics at district headquarters, arrangements for mass survey and treatment, free supply of penicillin and training of health personnel. A VD section was formed in November 1957 in the DGHS and since then, some planned operations were set in progress. Training facilities for intensive refresher courses for all types of VD workers were afforded in the VD training and demonstration center, Safdarjang Hospital, New Delhi and for short-term refresher courses and a university diploma in VD at the upgraded VD department of Madras General Hospital.[5]
In the third Five Year Plan, it was envisaged to expand existing facilities by providing additional VD clinics, stepping up the epidemiological and health education programs, case finding, routine testing of pregnant women for syphilis and further integration of VD control work within the existing public health services.[5]
As for the various venereal diseases prevalent during 1949 to 1958, a consolidated report from different states in India showed syphilis to be the most common STD, followed by gonorrhea, chancroid and other venereal diseases.[5] The total number of venereal disease cases was 8,67,268 in 1949 (syphilis - 3,45,219, gonorrhea - 2, 43, 696, chancroid - 87,306, other venereal diseases - 27,702); and in 1958, it was 4,84,602.[5] It has been said that for every single patient seeking help at a VD clinic, 20 such patients go elsewhere.[27] In 1970, a modest estimate of the incidence of venereal diseases in India was around 8-10% of the population.[27]
During the first three Five Year Plans, though there was stress on opening one headquarter clinic in each state and at least one district clinic in each district, only 261 VD clinics were established in the whole of India.[27] In the fourth Five Year Plan, only Rs. 1.5 crores was earmarked for the VD control program, which included the establishment of five state headquarter VD clinics, 78 district clinics and a central VD organization, including four mobile units. In spite of this set up, the venereal diseases control program remained far from satisfactory.[27]
Venereal diseases are higher in urban and industrial areas in India.[27] They are also higher in the sub-Himalayan areas and in some of the southern states. A continuous population shift to urban areas from rural areas has led to prostitution. There is plenty of commercialized and individualized prostitution in spite of the suppression of immoral traffic in women and girls in India by law.[27] The scale of prostitution in Bombay today remains a crude human index of the extent of poverty in Indian society, as well as of the continuing humiliation and exploitation of women.[7] Health education, sex education, propaganda and publicity were practically nonexistent in independent India and so also epidemiologic investigations.[33] Thus, there was persistent complacency among the medical and public health administrators in India.[27]
Advent of AIDS in India
The first reported cases of HIV infection diagnosed in India were among Madras sex workers in May 1986.[28] The epidemic of HIV in India was similar in many ways to the experience in sub-Saharan Africa and Thailand. The advent of AIDS in India in the 1980s was not at first regarded as a serious threat, with probable thinking that it is a white man′s disease and is due to Western immorality.[7] In 1988, AIDS began to spread rapidly in India, thus awakening the health authorities.
To formulate a strategy and plan for implementation of prevention and control of HIV/AIDS in the country, the Ministry of Health and Family Welfare constituted a National AIDS Committee in 1986 under the chairmanship of the Union Ministry of Health and Family Welfare, with representatives from various sectors.[29] The committee was formed with a view to bring together various ministries, nongovernment organizations and private institutions for effective coordination in implementing the program. The National AIDS Control Program (NACP) was launched in 1987. In the initial years, it focussed on generation of public awareness through more communication programs, introduction of blood screening for transfusion and conducting surveillance activities in the epicenters of the epidemic.[29]
In 1989, with the support of WHO, a medium-term plan for HIV/AIDS control was developed with a US$10 million budget provided from external sources.[29] Actual preventive activities like implementation of an education and awareness program, blood safety measures, control of hospital infection, condom promotion to prevent HIV/AIDS and strengthening of clinical services for both STD and HIV/AIDS gained momentum only in 1992. State AIDS cells were created in all the 32 states and union territories of the country for the effective implementation and management of NACP.[29]
The National AIDS Control Project (Phase I) was the first project in India to develop a national public health program in HIV/AIDS prevention and control and was implemented between 1992 and 1999.[29] In order to assess the prevalence of HIV, it conducted anonymous unlinked surveys in commercial sex workers and STD clinics, a high risk group; and in antenatal clinics, the population at risk. The ultimate objective of the project was to slow the spread of HIV to reduce future morbidity, mortality and the impact of AIDS by initiating a major effort in the prevention of HIV transmission.
The Phase II of the NACP became effective from 9th November 1999.[29] This 100% centrally sponsored scheme is being implemented in 32 states/union territories and 3 municipal corporations, namely, Ahmedabad, Chennai and Mumbai, through AIDS control societies. In this effort, nongovernment organizations (NGOs) and voluntary agencies are helping to a great extent.
Current status of HIV epidemic in India
Human immunodeficiency virus infection/acquired immunodeficiency syndrome (HIV/AIDS) is a major health problem in India.[4] The wide diversity of HIV prevalence in various states reflects the wide societal differences within India.[30] Evidence indicates multiple points of entry from multiple sources for the HIV epidemic in India, dating back to 1984. This has led to a heterogeneous pattern of spread, including rapid intravenous drug use related transmission in Manipur and predominantly sexual transmission in Tamil Nadu, Maharashtra and neighboring states (associated with commercial sex). By 2003, it was estimated that 5.1 million people were living with HIV/AIDS in India, second only to South Africa in absolute numbers.[30] Most infections have been acquired through sexual transmission (80.8%), with 5.1% acquired through injecting drug use, 5.5% associated with blood or blood products and less than 1% of cases infected through mother-to-child transmission.[29]
Setting up of government nodal agencies in independent India
There has been a program for the control of STDs among the population of India for many decades.[4] India was plagued by many life-threatening diseases and as in most other countries, STD services were a low priority.[9] Even before the country achieved independence, a National STD Control Program was started in 1946.[4] A Venereal Disease ection was formed in November 1957 in the Directorate General of Health Services.[5] This program continued to operate till 1991 and with the arrival of HIV infection in the country and because of its strong relation with STD, the program was brought under the purview of National AIDS Control Organization (NACO) in the year 1992.[4] The National AIDS Control Program existed from 1987, but NACO was set up in 1992. This program emphasized more on health seeking behavior of the individuals having STDs and removal of the social stigma attached to the problem of STDs.[4]
Academic developments
Europeans introduced modern medicine to India. At the time of independence, there were already 19 medical colleges in undivided India (including two in the princely states of Mysore and Hyderabad).[31] The total number of students admitted each year was about 1,200. Calcutta Medical College and Madras Medical College were founded in 1835.[31],[32] Madras Medical College actually started on 16th November 1664 as a small hospital at the Fort St. George to treat the sick soldiers of the East India Company. Other well-known colleges of the pre-independence days are Grant Medical College, Mumbai (founded in 1845, it gave the opportunity to the native citizens of the presidency to study western medicine from some outstanding teachers); King George Medical College, Lucknow (1911); and Lady Hardinge Medical College (exclusively for women), Delhi (1916).[31],[33] The Institute of Venereology in Madras Medical College was founded in the year 1952 and is thought to be the oldest venereology department in India.[4] In the early formative years, the strength and solidity to this institute was given by Col. Vasudeva Rao. Dr. R. V. Rajam was his founder director, an international figure for his research work on venereal diseases. The successors to Dr. Rajam were Dr. P. N. Rangiah and Dr. C. N. Sowmini. After independence, venereology developed along with dermatology in most parts of India.[4]
In the year 1935, Dr. U. B. Narayan Rao started a private publication, the Indian Journal of Venereology from Bombay (Mumbai).[34],[35] In 1940, the name of this journal was changed to Indian Journal of Venereal Diseases and Dermatology and it was published quarterly. This journal subsequently merged with the Indian Journal of Dermatology and Venereology in the year 1947. On 31st March 1955, the journal became the official publication of the Association. It had three editors: Dr. G. Panja, Dermatology Section; Dr. R. V. Rajam, Venereology Section; and Dr. U. B. Narayan Rao, Managing Editor. After the death of Dr. Narayan Rao in 1960, Dr. T. K. Mehta took over as the Managing Editor. Dr. U. B. Narayan Rao also gets the credit for the creation of an association of dermatologists and venereologists in Bombay in the year 1947. On July 1st, 1947, this Bombay association was inaugurated and it organized an All-India Conference of Dermatologists and Venereologists on December 27 and 28, 1947, at J. J. Hospital, Bombay.[34],[35] In 1973, at a conference held in Udaipur, the Indian Association of Dermatologists and Venereologists merged with other dermatology associations to form the Indian Association of Dermatologists, Venereologists and Leprologists. The name Indian Journal of Dermatology and Venereology was changed to Indian Journal of Dermatology, Venereology and Leprology (IJDVL). Since then, Dr. S. C. Desai, Dr. Bhaktavizam, Dr. (Mrs.) Rachel Mathai, Dr. J. S. Pasricha, Dr. S. G. Deshpande, Dr. Gurmohan Singh and Dr. K. Pavithran had been the chief editors of IJDVL.
The Indian Association for the Study of Sexually Transmitted Diseases (IASSTD) came into existence in the year 1975 with its founder members being Dr. K. N. Gopalan, Dr. G. Chandrashekhar Rao, Dr. K. Vijaylaksmi, Dr. P. K. Dharmalingam and Dr. M. K. Venkataraman.[4] Dr. Sowmini was its president and Dr. C. C. Mohan Ram was its secretary at that time. After the advent of AIDS in India, its name was changed to Indian Association for the Study of Sexually Transmitted Diseases and AIDS (1993). Since its formation, this association is organizing annual conferences. In 1980, this specialty, under the banner of Indian Association for the Study of Sexually Transmitted Diseases, started its own exclusive journal, the Indian Journal of Sexually Transmitted Diseases.[4] The late Dr Sardari Lal was its founder editor and guiding force, who had already made a mark in the field of research, especially donovanosis.[36] Dr. R. C. Sharma and Dr. Rishi Bhargava were the successors to Dr. Sardari Lal.[4]
Somehow, venereology did not prosper, even though it led dermatology and leprology in the field of teaching and in starting its own journal in the early 20th century, probably due to lack of interest and government commitment in the specialty.[4] The extent of teaching of venereology in India can be judged from the report of Webster in 1966.[37] The average time spent in the teaching of venereology as a separate subject in the 437 schools was 17.1 h. The average number of hours devoted to the teaching of venereology in India was 61.2 as compared to 137 in USSR, 106 in Bulgaria, 105 in Iran, 104 in Jamaica, 100.7 in Poland, 90 in Greece, 84 in Malta, 76.8 in Yugoslavia and 66.3 in Mexico. The current teaching program on the subject provides adequate exposure. The monograph by Dr. Rajam and Dr. Rangiah on donovanosis (granuloma inguinale, granuloma venereum) is testimony to the teaching and research standards set by these two giants at the Institute of Venereology, Madras.[14] In 1942, Bombay University appointed a committee to frame rules and regulations for starting a diploma course in dermatology and venereology (DVD). It was a course of 1-year duration and the first DVD examination was held in October 1945 . In 1947, the College of Physicians and Surgeons (Bombay) allowed candidates to appear for their fellowship examination in dermatology and venereology. Since then, many more medical colleges have been recognized for training of postgraduates in this specialty.[35]
Venereology in India has been combined with dermatology in most of the universities.[4],[27] Besides Tamil Nadu and Andhra Pradesh, at Grant Medical College and Sir J. J. Group of Hospitals, Mumbai, Skin and STDs were two different units, which later were merged together. Diploma and degree courses have been started in many universities, but the scope of research in venereology is extremely poor and inadequate due to poorly equipped STD clinics in terms of manpower and infrastructure. As in India, throughout the world, experts in sexually transmitted infections have come from a variety of medical specialties over the course of the 20th century.[1] During the first 50 years and owing to medical importance of syphilis and its dermatologic manifestations, a specialty of dermatolo-venereology emerged in Europe and North America. However, with the near-eradication of syphilis and gonorrhea in the western world in the 1950s, many dermatology training programs lost interest in venereology and journals of syphilology and dermato-venereology ceased publication.
Emerging STIs scenario
With regard to India, most STIs are managed in the informal and private medical sectors or are self treated. STIs survey data are limited in India, but these surveys indicate a very diverse picture.[38] In community-based surveys of married and unmarried women in India, the chlamydia prevalence ranged between 0.5% and 28.7%, gonorrhea between 0% and 4.2% and syphilis between 0.2% and 10.5%.[39] In a recently published retrospective study of the pattern of sexually transmitted diseases during the 10-year period from 1990 at Kottayam, genital ulcer diseases (GUDs) accounted for the maximum number of STDs (73.5%), followed by condyloma acuminatum (17.5%) and gonorrhea (10.1%).[40] Amongst GUDs, syphilis was the most common disease, accounting for 57.3% of them. Granuloma inguinale and lymphogranuloma venereum were found to be rare. The overall trend of STDs was declining, with the total number of patients during the first year of study being 129, while it was 41 during the last year of study. Bacterial STDs showed a striking reduction in numbers. The decline was less marked in the case of viral STDs. During the last 10-15 years, after the emergence of AIDS and owing mainly to fear of AIDS, rates of gonorrhea, syphilis, hepatitis B infection and HIV have declined by 80-95% or more in the USA.[1] For the past 7-9 years, STI rates in homosexual men again are rising modestly. Globally the HIV incidence is still rising in some areas of Africa, Asia and Eastern Europe and declining in others.[1]
In India, the main strategy aimed at achieving effective management for people with established infections has been to integrate STD services into the existing health care system, with special emphasis on integration at the primary health care (PHC) level. The National AIDS Control Organization (NACO) for case management at this level recommends syndromic management.[41] Effectiveness of syndromic management in women is currently under debate.[39] The NACO is now also focusing on women reproductive health issues and involving gynecologists.
Future directions
Donovanosis will be eradicated in several nations, but syphilis eradication will be successful only by 2020.[42] Gonorrhea, chlamydial infections, chancroid and trichomoniasis may also persist despite their curability. With the exception of hepatitis B, HIV and other blood-borne pathogens will continue to flourish until blood supplies and medical injections, as well as illicit drug use and tattooing, are made safe. Anogenital warts and herpes will also persist and possibly increase, as may candidiasis, vulvovaginitis, bacterial vaginosis, balanitis, prostatitis, sexual assault and other forms of sexual abuse. The problems of the spreading HIV epidemic, drug resistance, poor health facilities and financial constraints are a great hindrance in achieving a reduction in the incidence and prevalence of STIs. A worthy vision for 2020 is of a world with universal sexual health as well as a world free of sexual ill health. Our task for the future, therefore, is to work together to ensure that this vision becomes a reality.[42] Vast numbers of people in India are severely disadvantaged in terms of income, education, power structures and gender.[39] Addressing these basic issues of human rights lies at the core of achieving better health outcomes[43] (including reproductive and infectious diseases) in India. Such a challenge is formidable in terms of its required scope and coverage but lies at the heart of improving sexual health for the greatest number of people in India.
| 1. |
Judson F. Introduction. In : Kumar B, Gupta S, editors, Sexually Transmitted Infections. 1st ed. Elsevier: New Delhi; 2005. p. 1-4.
[Google Scholar]
|
| 2. |
Bingham JS. Historical aspects of sexually transmitted infections. In : Kumar B, Gupta S, editors, Sexually Transmitted Infections, 1st ed. Elsevier: New Delhi; 2005. p. 5-17.
[Google Scholar]
|
| 3. |
Sharma VK, Khandpur S. Epidemiology of sexually transmitted diseases. In : Sharma VK, editor. Sexually Transmitted Diseases and AIDS. Viva Books Pvt Ltd: New Delhi; 2003. p. 1-41.
[Google Scholar]
|
| 4. |
Thappa DM. History of venereal diseases and venereology in India. Indian J Sex Transm Dis 2002;23:67-79.
[Google Scholar]
|
| 5. |
Tampi RB. Venereal diseases in India. Central Health Education Bureau, New Delhi: DGHS, Ministry of Health, Government of India, 1962. p. 1-27.
[Google Scholar]
|
| 6. |
The Kama Sutra of Vatsyayana-The classic Hindu treatise on love and social conduct, translated by Sir Richard F Burton and FF Arbuthnot, 15th Jaico Impression. Jaico Publishing House: Mumbai; 2005.
[Google Scholar]
|
| 7. |
Arnold D. Sexually transmitted diseases in nineteenth and twentieth century India. Genitourin Med 1993;69:3-8.
[Google Scholar]
|
| 8. |
Kumar B, Gupta S, Muralidhar S. Mucocutaneous manifestations of secondary syphilis in North Indian patients: A changing scenario. J Dermatol 2001;28:137-44.
[Google Scholar]
|
| 9. |
Roy RB. Sexually transmitted diseases and the Raj. Sex Transm Infect 1998;74:20-6.
[Google Scholar]
|
| 10. |
Ronald AR, Plummer FA. Chancroid and Haemophilus ducreyi. Ann Intern Med 1985;102:705-7.
[Google Scholar]
|
| 11. |
Willcox RR. Fifty years since the conception of an organized venereal diseases service in Great Britain: The Royal commission of 1916. Br J Venereal Dis 1967;43:1-9.
[Google Scholar]
|
| 12. |
MacLeod K. Precis of operations performed in the wards of First Surgeon, Medical College Hospital during the year 1881. Indian Med Gazette 1882;17:112-23.
[Google Scholar]
|
| 13. |
Donovan C. Medical cases from Madras General Hospital: ulcerating granuloma of the pudenda. Indian Med Gazette 1905;40:414.
[Google Scholar]
|
| 14. |
Rajam RV, Rangiah PN. Donovanosis. (Granuloma inguinale, Granuloma venereum) World Health Organization: Geneva; 1954. p. 10.
[Google Scholar]
|
| 15. |
Goldberg J. Studies on granuloma inguinale VII. Some epidemiologic considerations of the disease. Br J Vener Dis 1964;40:140-5.
[Google Scholar]
|
| 16. |
Ramachandra Rao MG. A case of granuloma inguinale. Indian Med Gazette 1931;66:21.
[Google Scholar]
|
| 17. |
Caddy A. Climatic buboes-twelve cases in Calcutta. Indian Med Gazette 1902;27:27.
[Google Scholar]
|
| 18. |
Sowmini CN. Late manifestations of LGV. Paper presented at the 29th General Assembly of International Union Against Venereal Diseases and Treponematoses, Leeds: 1978.
[Google Scholar]
|
| 19. |
Rangiah PN, Vijayalakshmi K, Siddapppa K. Lymphogranuloma venereum. In : Valia RG, Valia AR, editors. IADVL Textbook and Atlas of Dermatology. 1st ed. Bhalani Publishing House: Mumbai; 1994. p. 1225-33.
[Google Scholar]
|
| 20. |
Rajam RV, Rangiah PN. Lymphogranuloma venereum. Indian J Dermatol Venereol 1955;21:4.
[Google Scholar]
|
| 21. |
Ramana Rao RV, Bose YS, Kumar BS. Viral STDs. In : Valia RG, Valia AR, editors. IADVL Textbook and Atlas of Dermatology, 1st ed. Bhalani Publishing House: Mumbai; 1994. p. 1234-50.
[Google Scholar]
|
| 22. |
King A, Nicol C, Rodin P. Venereal diseases. 4th ed. The English Language Book Society and Bailliere Tindall: London; 1980. p. 309-20.
[Google Scholar]
|
| 23. |
Vishwanath S, Talwar V, Prasad R, Coyaji K, Elias CJ, de Zoysa I. Syndromic management of vaginal discharge among women in a reproductive health clinic in India. Sex Transm Infect 2000;76:303-6.
[Google Scholar]
|
| 24. |
First annual report of the Medical Women for India Fund, 1884 in Home Medical, 32, Sept. National Archives of India: New Delhi; 1886.
[Google Scholar]
|
| 25. |
Balfour MI. 'Venereal disease in India'. J Assoc Med Women India 1924;12:15.
[Google Scholar]
|
| 26. |
Report of the Health Survey and Development Committee 1. Manager of Publications: Delhi; 1946. p. 123.
[Google Scholar]
|
| 27. |
Banerjee BN. Venereology-Conditions in India. JIMA 1971;56:139-40.
[Google Scholar]
|
| 28. |
Simoes EA, Babu PG, John TJ, Nirmala S, Solomon S, Lakshminarayana CS, et al . Evidence for HTLV-III infection in prostitutes in Tamil Nadu (India). Indian J Med Res 1987;85:335-8.
[Google Scholar]
|
| 29. |
National AIDS Control Organization. National AIDS Control Program and Indian Scenario. National AIDS Control Organization (NACO). http://www.naco.nic.in/ Accessed 8th December, 2003.
[Google Scholar]
|
| 30. |
Donovan B, Kaldor JM. The epidemiology of HIV infection and AIDS in Asia and the Pacific: Global perspective. In : Kumar B, Gupta S, editors. Sexually Transmitted Infections, 1st ed. Elsevier: New Delhi; 2005. p. 57-66.
[Google Scholar]
|
| 31. |
IQRA Society for Career Guidance [Course Guide-Chapter 43: Medicine and Dentistry] Hyderabad, Andhra Pradesh, India: IQRA Society for Career Guidance [updated 2002 IQRA; cited 2004 Feb 19]. http://iqra-careers.com/c43.html Accessed 19th February, 2004.
[Google Scholar]
|
| 32. |
Madras Medical College [History of MMC] Chennai, Tamil Nadu, India: Madras Medical College. http://mmcindia.edu/ Accessed 19th February, 2004.
[Google Scholar]
|
| 33. |
King Edward VII Memorial Hospital and Seth Gordhandas Sunderdas Medical College [Seth Gordhandas Sunderdas Medical College and King Edward VII Memorial Hospital, Bombay: Sunil. K. Pandya], Mumbai: King Edward VII Memorial Hospital and Seth Gordhandas Sunderdas Medical College, http://www.kem.edu/college/history.htm Accessed 19th February, 2004 .
[Google Scholar]
|
| 34. |
Sehgal VN. Indian Dermatology. Int J Dermatol 1993;32:838-44.
[Google Scholar]
|
| 35. |
Thappa DM. History of Dermatology, Venereology and Leprology in India. J Postgrad Med 2002;48:160-5.
[Google Scholar]
|
| 36. |
Sharma RC. Obituary. Dr Sardari Lal. Indian J Sex Transm Dis 1993;14:72.
[Google Scholar]
|
| 37. |
Webster B. Teaching of venereal diseases in medical schools throughout the world: Preliminary report. Br J Venereal Dis 1966;42:132-3.
[Google Scholar]
|
| 38. |
Bourne C, Donovan B. The epidemiology of sexually transmitted infections in Asia and the Pacific. In : Kumar B, Gupta S, editors. Sexually Transmitted Infections, 1st ed. Elsevier: New Delhi; 2005. p. 44-56.
[Google Scholar]
|
| 39. |
Hawks S, Santhya KG. Diverse realities: sexually transmitted infections and HIV in India. Sex Transm Infect 2002;78:i31-9.
[Google Scholar]
|
| 40. |
Narayanan B. A retrospective study of the pattern of sexually transmitted diseases during a ten-year period. Indian J Dermatol Venereol Leprol 2005;71:333-7.
[Google Scholar]
|
| 41. |
National AIDS Control Organisation. Country scenario 1997-98. Ministry of Health and Family Welfare: New Delhi; 1998.
[Google Scholar]
|
| 42. |
Philipot R. Future directions for STIs and sexual health in Asia-Pacific region: 2002-2020. In : Kumar B, Gupta S, editors, Sexually Transmitted Infections. 1st ed. Elsevier: New Delhi; 2005. p. 18-26.
[Google Scholar]
|
| 43. |
Aral SO, Mann JM. Commercial sex work and STD: the need for policy interventions to change societal patterns. Sex Transm Dis 1998;25:455-6.
[Google Scholar]
|
Fulltext Views
6,685
PDF downloads
3,118





