Exploring the unusual: A case of vulvar Crohn’s disease with concomitant leukocytoclastic vasculitis
Corresponding author: Dr. Neena Khanna, Department of Dermatology, Amrita Institute of Medical Sciences and Research Centre, Sector 88, Faridabad, Haryana, India. neena_aiims@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Gupta S, Sharma V, Bhat B, Khanna G, Khanna N. Exploring the unusual: A case of vulvar Crohn’s disease with concomitant leukocytoclastic vasculitis. Indian J Dermatol Venereol Leprol. 2024;90:796-8. doi: 10.25259/IJDVL_167_2023
Dear Editor,
Crohn’s disease is a chronic inflammatory disorder that affects the gastrointestinal tract and is often associated with extra-intestinal manifestations including cutaneous ones, which are estimated to be present in 18–44% patients.1 These cutaneous manifestations could be due to contiguous spread from the gastrointestinal tract (sinuses and fistulae), or non-contiguous spread (metastatic) or reactive spread (erythema nodosum, pyoderma gangrenosum, vasculitis). Of these, the reactive manifestations are most common. Here, we report an interesting combination of vulvar Crohn’s disease (a metastatic manifestation) with leukocytoclastic-vasculitis (a reactive manifestation) without overt evidence of gastrointestinal tract involvement.
A 24-year-old, unmarried woman presented for progressive asymptomatic swelling of the labia for the past four years and recurrent rashes over lower extremities for the past two years. The swelling initially started as a small (0.5 cm) papulo-nodule on left labia majora. This increased in size and new nodules developed to involve both labia majora and adjoining areas over the next six months. Two years later, she started developing recurrent palpable purpura on the lower extremities [Figure 1]. Though the genital lesions were not biopsied, biopsy from leg lesions showed perivascular neutrophils with fibrinoid necrosis suggestive of leukocytoclastic-vasculitis. She had received methotrexate (15 mg/week) and tapering doses of oral corticosteroids, to which the vasculitis had responded but the genital lesions had not. She did not give a history of abdominal pain, diarrhoea or weight loss and neither did she give a history of any ocular or respiratory symptoms.
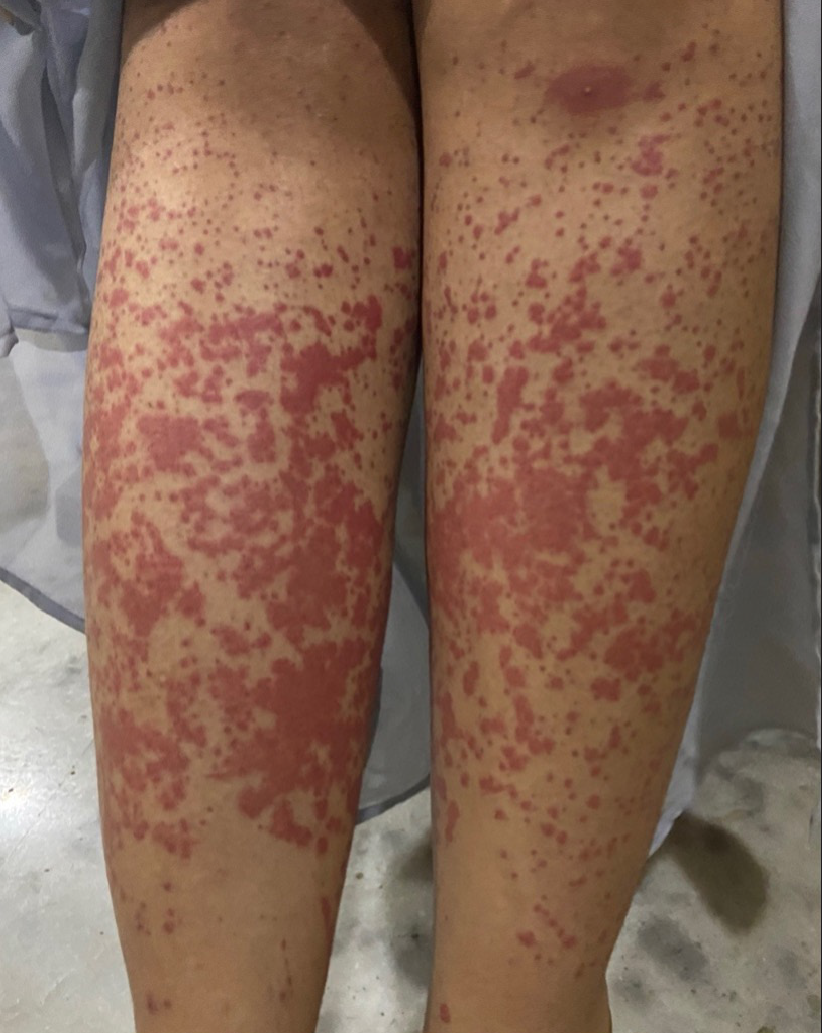
- Palpable purpura over the lower extremities.
On examination, there was thickening of bilateral labia majora causing distortion of vulvar architecture. There were multiple, well-defined, firm erythematous nodules of varying sizes (0.5–5 cm diameter) which had coalesced and were surmounted with cerebriform convolutions and deep furrows with superficial erosions and occasional fissuring in the depth of furrows. There was no vaginal discharge [Figure 2]. Further inspection of the perineum showed no anal fistulae, ulcers, abscesses or scarring. There was no generalised or locoregional lymphadenopathy. Abdominal examination revealed no tenderness or palpable mass and there were no significant systemic findings clinically.

- Multiple, well-defined, firm erythematous nodules of varying sizes (0.5–5 cm diameter) which had coalesced and were surmounted with cerebriform convolutions and deep furrows with superficial erosions and occasional fissuring in the depth of furrows.
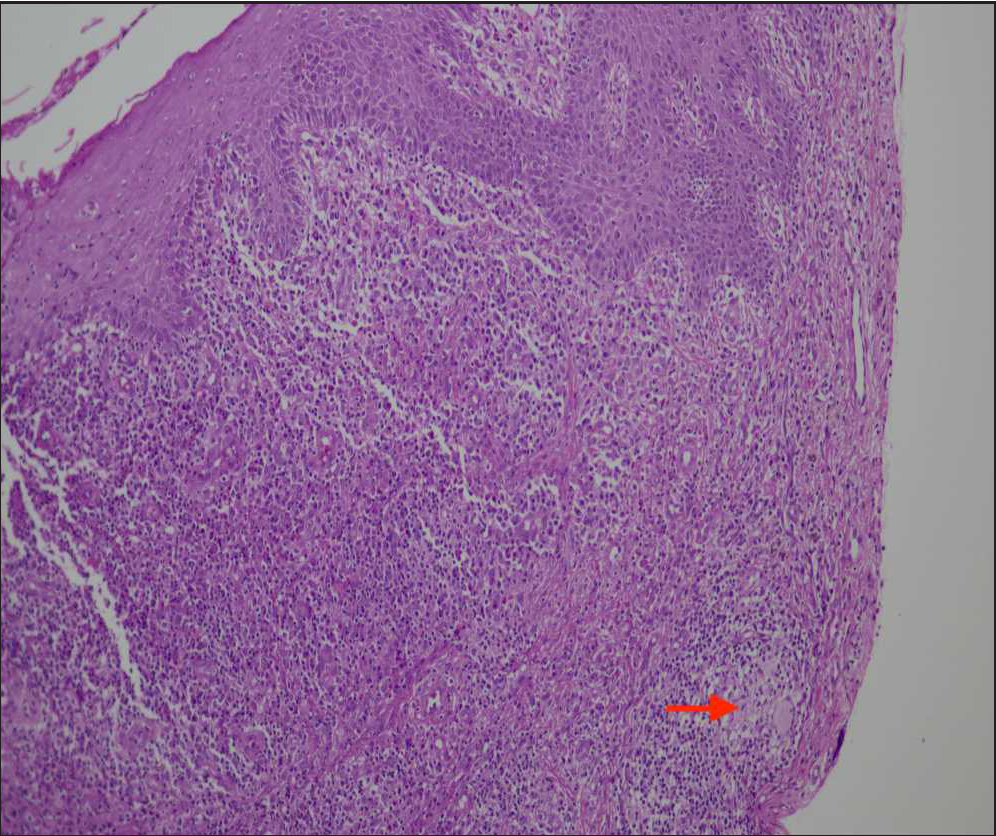
- Haematoxylin & eosin (H&E) staining at 100× showing hyperplastic squamous epithelium in left and upper half of the image, the lower half showing dense mixed inflammation and a non-necrotizing epithelioid cell granuloma (red arrow) at the lower end of the image.
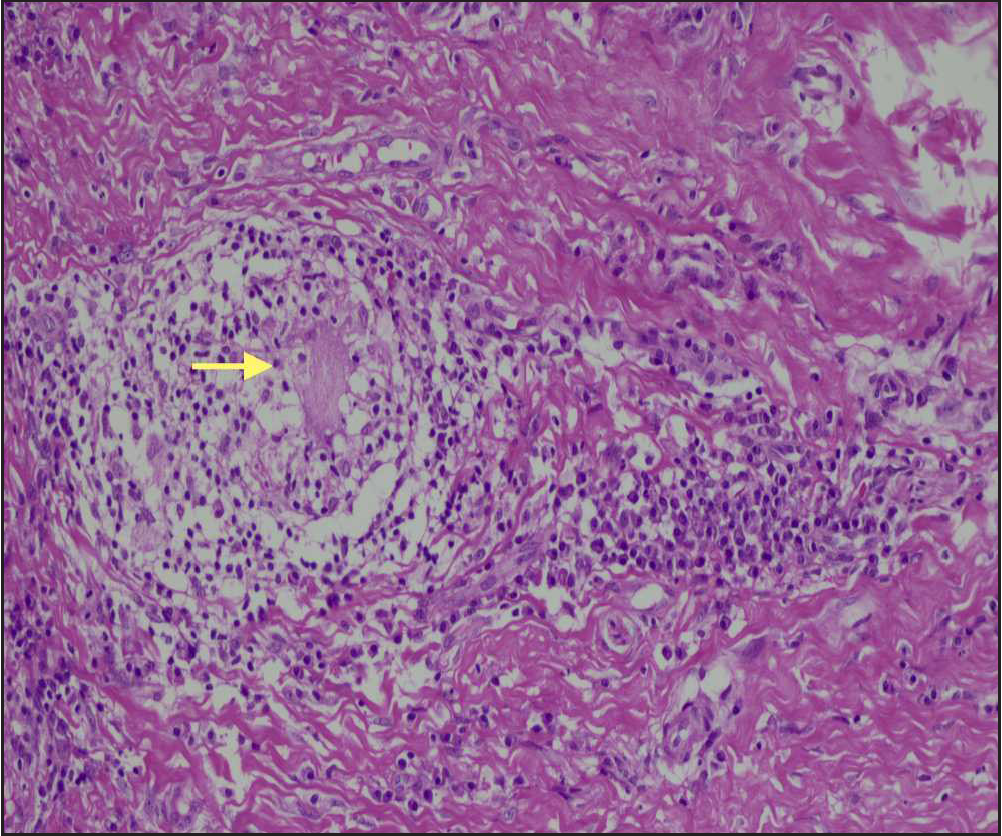
- Haematoxylin & eosin (H&E) at high power (200×) showing a non-necrotizing epithelioid cell granuloma with a Langhans type of giant cell in the centre (yellow arrow) and surrounding lymphocytic cuffing.
Incisional skin biopsy from labia majora showed ulcerated and hyperplastic epithelium with dense active inflammatory granulation tissue, focal acute inflammatory exudate and few non-necrotizing epithelioid cell granulomas with a few Langhans giant cells [Figures 3a and 3b]. ZN stain for AFB was negative.
Routine investigations were normal. CECT abdomen was normal without any evidence of Crohn’s disease, tuberculosis or sarcoidosis. In view of the absence of systemic symptoms, normal ACE levels and no lymphadenopathy, sarcoidosis was ruled out. The absence of cough, fever and other systemic symptoms, a normal chest radiogram and CT abdomen and a negative Mantoux test were indicators of the absence of tuberculosis. Occult blood in the stool and CECT abdomen were normal, making intestinal Crohn’s disease unlikely.
In view of the clinical presentation, histopathology, presence of leukocytoclastic-vasculitis and absence of gastrointestinal tract involvement, the final diagnosis was metastatic Crohn’s disease with leukocytoclastic-vasculitis. Patient was given oral metronidazole 250 mg daily and three sessions of intralesional steroids which resulted in 20–30% improvement over two months’ follow-up period.
Metastatic Crohn’s disease is a rare but under-recognised phenomenon characterised by granulomatous inflammation of the skin, non-contiguous from the gastrointestinal tract. The most common areas of involvement for metastatic Crohn’s disease are the vulva, penis, trunk, upper extremity and face. Around 70–90% of patients present with a prior intestinal Crohn’s disease, but in 10–30% of cases, as in our case, the gastrointestinal tract is not involved.2
Vulvar Crohn’s disease (anogenital granulomatosis) is a variant of metastatic Crohn’s disease and is defined by granulomatous inflammation independent of fistulizing Crohn’s disease. Although most cases of vulvar Crohn’s disease cause minimal discomfort, vulvar pain and pruritus can be seen in up to one third of the patients.3
Clinically, vulvar Crohn’s disease has a variable presentation with the most common type being inflammatory asymmetrical vulvar oedema, which can affect both labia majora and minora and the vaginal wall. It can also manifest as single or multiple, asymptomatic or painful ulceration, which can be aphthoid and superficial or deep with an indurated base. Linear ‘knife-cut’ ulcerations may extend to the groins and are characteristic of genital Crohn’s disease. Hypertrophic lesions could occur, either localised or extensive. Rarely there could be chronic suppuration leading to abscess formation.4
There are a few reports of leukocytoclastic-vasculitis occurring in patients with Crohn’s disease.5 The lesions of leukocytoclastic-vasculitis are characterised by the appearance of palpable purpura, urticaria and ulcero-necrotic papulo-nodules predominantly on the lower extremities which improve with immunosuppressive therapy. We were unable to find any specific characteristics that have been reported for leukocytoclastic-vasculitis associated with Crohn’s disease. To the best of our knowledge, the combination of leukocytoclastic-vasculitis with metastatic Crohn’s disease has not been previously documented.
This case highlights the rare but under-recognised phenomenon of metastatic Crohn’s disease. Its association with leukocytoclastic-vasculitis makes it even more noteworthy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Skin Manifestations of Inflammatory Bowel Disease. Clin Rev Allergy Immunol. 2017;53:413-27.
- [CrossRef] [PubMed] [Google Scholar]
- Metastatic cutaneous Crohn’s disease of the face. Eur J Gastroenterol Hepatol. 2011;2:954-6.
- [CrossRef] [PubMed] [Google Scholar]
- Metastatic Crohn’s disease: an underestimated entity. J Dtsch Dermatol Ges. 2021;19:973-82.
- [CrossRef] [PubMed] [Google Scholar]
- Leukocytoclastic Vasculitis as an Extraintestinal Manifestation of Crohn’s Disease. Case Rep Gastroenterol. 2021;15:825-31.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





