Translate this page into:
Extensive and refractory genital herpes in human immunodeficiency virus-infected patient successfully treated with imiquimod: Case report and literature review
Correspondence Address:
Helena Reich Camasmie
Rua Mariz e Barros, 775, Tijuca, 20270-002 Rio de Janeiro
Brazil
| How to cite this article: Camasmie HR, Barbosa C, Lupi O, Lima RB, Serra M, D'Acri AM, Martins CJ. Extensive and refractory genital herpes in human immunodeficiency virus-infected patient successfully treated with imiquimod: Case report and literature review. Indian J Dermatol Venereol Leprol 2017;83:256-259 |
Sir,
Herpes genitalis is the most common sexually transmitted disease worldwide. Its incidence has been increasing, especially among positive human immunodeficiency virus patients.[1] The typical presentations of cutaneous herpes simplex virus are well known and rarely cause diagnostic difficulty. However, in patients with advanced human immunodeficiency virus infection, unusual and severe manifestations of herpes simplex virus infection are common and are included among the opportunistic processes that define the acquired immunodeficiency syndrome.[2] The unusual clinical presentations increasingly observed in clinical practice have led to the use of new treatment modalities such as immunomodulatory agents, in particular topical imiquimod cream as an adjunctive therapy to the first-line drug acyclovir with satisfactory results.[1] Our case report describes a human immunodeficiency virus-infected man with a herpetic infection that was refractory to acyclovir but not to imiquimod, followed by literature review of similar cases.
A 54-year-old human immunodeficiency virus-infected man presented with a 5-month history of painful penile erosions. Physical examination revealed extensive herpetiform erosions involving the penis [Figure 1a]. His CD4 cell count was 299/µL and his viral load was undetectable. He had been receiving antiretroviral therapy and had no previous history of genital herpes infection. He had already been treated in a primary health-care unit with acyclovir (4 g daily), penicillin and azithromycin with no improvement. Results of blood tests were positive for syphilis (venereal disease research laboratory 1:32; fluorescent treponemal antibody-absorption positive) and herpes simplex virus (immunoglobulin M negative; immunoglobulin G positive), cytomegalovirus (immunoglobulin M negative; immunoglobulin G positive) and chlamydia (immunoglobulin M negative; immunoglobulin G positive). Skin biopsy was inconclusive. The patient was hospitalized and began empiric treatment with crystalline penicillin and intravenous acyclovir (800 mg three times daily) for 15 days due to oral acyclovir refractory herpes simplex. He was discharged with partially improved but still unhealed genital ulcers.
 |
| Figure 1a: Genital penile erosions before treatment |
A second skin biopsy revealed typical herpes inclusions and multinucleated giant cells and immunohistochemical studies supported the diagnosis of herpes simplex virus 1 and 2 infections [Figure 2a] and [Figure 2b]. Subsequently, the patient was treated initially with famciclovir (500 mg two times daily for 8 weeks), but due to high medication cost, it was changed back to acyclovir (400 mg six times daily for 12 weeks). Despite these multiple treatment attempts, he experienced no clinical improvement. The patient was given a trial regimen of topical 5% imiquimod cream applied three times/week for 8 weeks and then five times/week, together with oral acyclovir (400 mg three times daily), for 16 weeks. Complete healing of the lesions was achieved after treatment was completed [Figure 1b].
 |
| Figure 1b: Clinical result after imiquimod therapy |
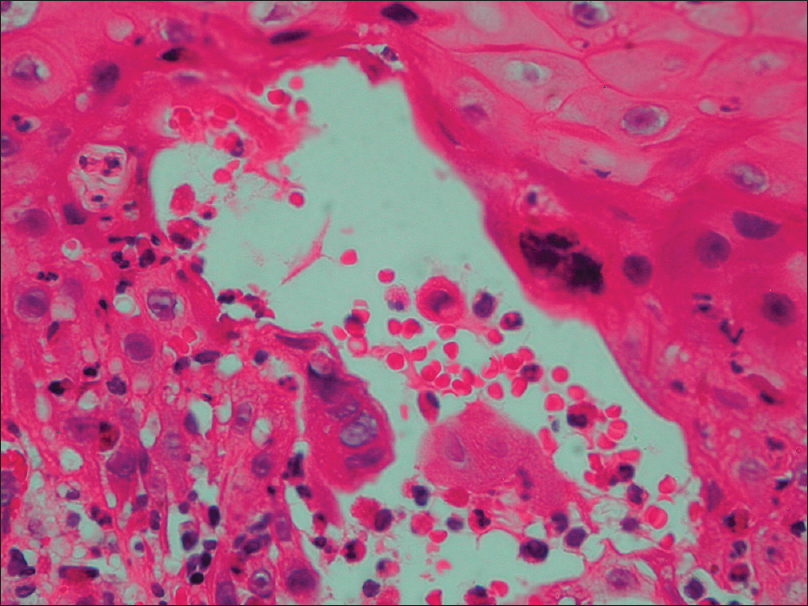 |
| Figure 2a: Multinucleated giant cells with viral nuclear inclusions and nuclear molding (H and E, ×400) |
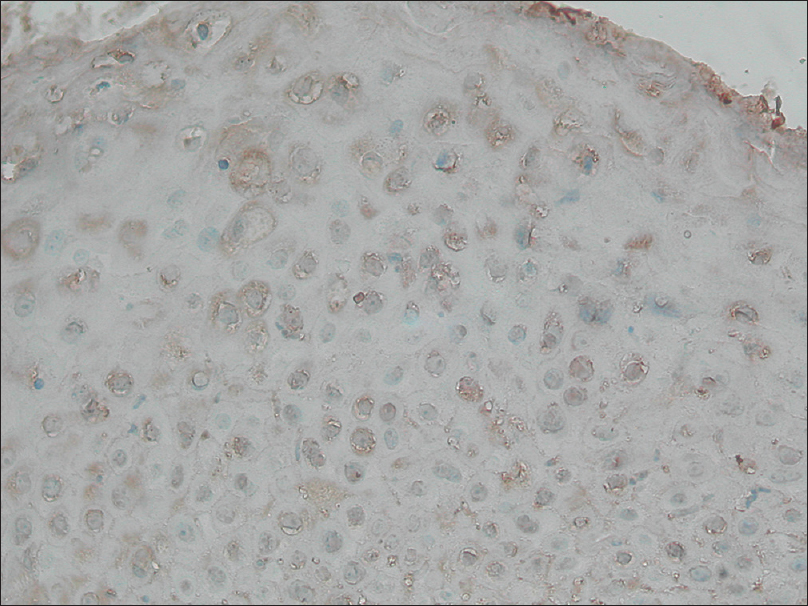 |
| Figure 2b: Immunohistochemical study (×400) positive for herpes simplex virus |
Herpes simplex virus infections are exceedingly common and pose a particular problem in immunocompromised patients. They may experience an excessive number and size of lesions in both primary and reactivated herpes simplex virus infections in comparison with immunocompetent patients. As CD4 cell counts drop and immunosuppression worsens, recurrent episodes increase in frequency and severity until there is no period of complete healing between episodes. Nonhealing ulcers of the genital region in immunocompromised patients should elicit a high degree of suspicion of chronic herpes simplex virus infection. Chronic herpes simplex virus ulcer of more than 1 month duration is an acquired immunodeficiency syndrome-defining illness in human immunodeficiency virus-infected patients.[3]
Treatment with antivirals such as acyclovir is still the mainstay of prescribed therapy. For the treatment of recurrent episodes, the use of antivirals can reduce the time of healing, time of cessation of viral shedding and duration of symptoms.[1] Increased dosages of acyclovir, valacyclovir and famciclovir may be required.[3]
The emergence of drug-resistant herpesvirus strains is associated with the increase in the use of acyclovir.[4] Foscarnet sodium has been the drug of choice in cases of acyclovir resistance. However, it has also been associated with drug-resistant strains that replicate despite drug presence.[5] Success with topical imiquimod in cases of nonhuman immunodeficiency virus-associated recurrent genital herpes simplex virus infection with documented acyclovir resistance was reported.[6] Topical imiquimod is an immunomodulatory drug that signals through toll-like receptors 7 to stimulate cell-mediated immune responses, showing promising results for the treatment of herpes simplex virus infection and in atypical cases, studies showed that imiquimod provides an added benefit.[1] Therefore, imiquimod presents itself as a valuable ally when treating acyclovir refractory herpes simplex virus infections, particularly in the setting of emerging resistance.
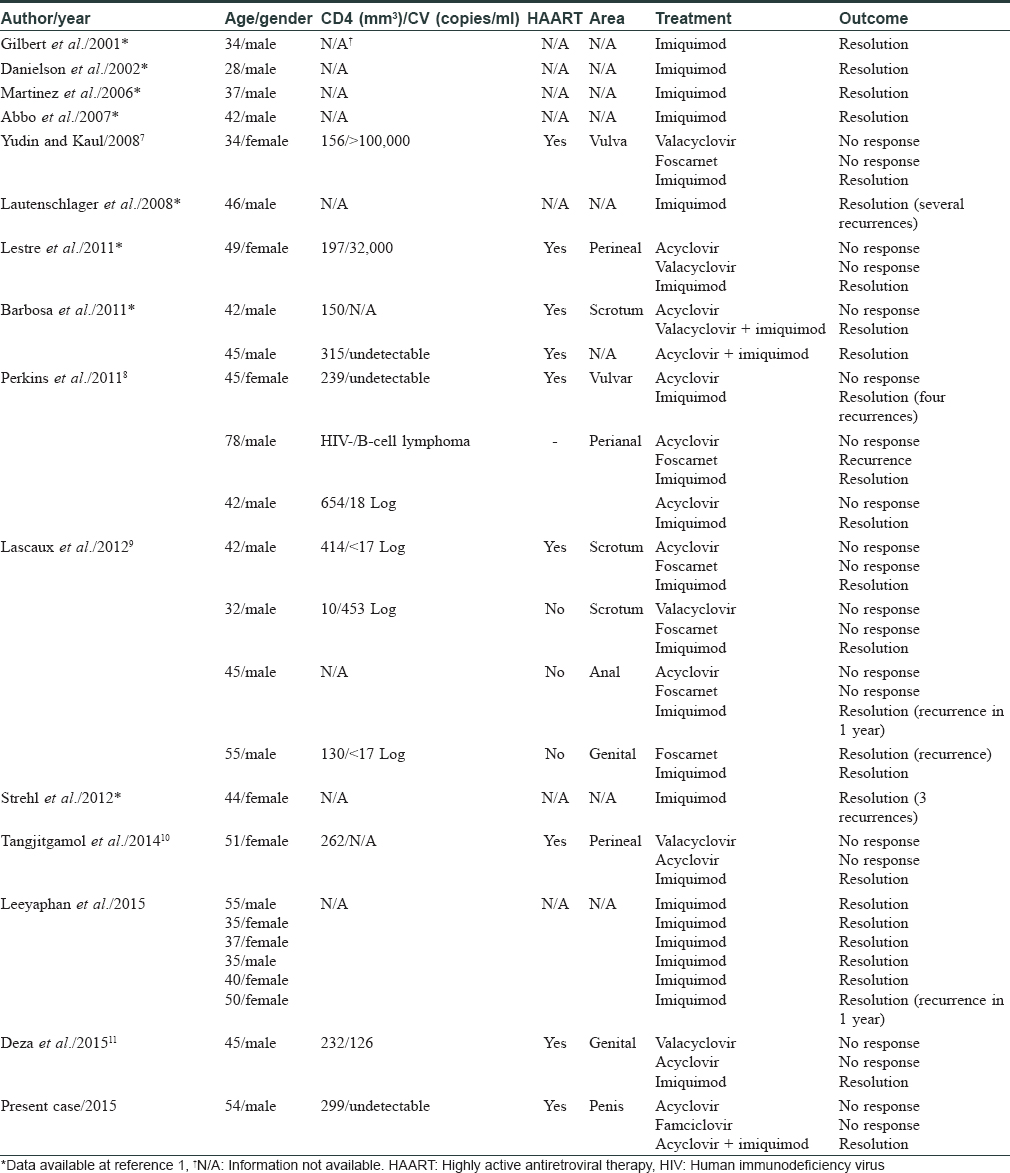
Literature review indicated that despite antiviral resistance, treatment with imiquimod has been successful [Table - 1]. Data on 25 patients from 14 different studies showed that clinical cure was the main result with only some instances of recurrences (n = 5) after topical 5% imiquimod therapy.
Our patient failed to respond to classic acyclovir monotherapy, showing a great response after the addition of topical imiquimod cream. Imiquimod may be considered as a possible adjuvant therapy in resistant genital herpes simplex virus infections in light of our experience with this difficult case.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.[11]
| 1. |
Leeyaphan C, Surawan TM, Chirachanakul P, Prasertworonun N, Punyaratabandhu P, Omcharoen V, et al. Clinical characteristics of hypertrophic herpes simplex genitalis and treatment outcomes of imiquimod: A retrospective observational study. Int J Infect Dis 2015;33:165-70.
[Google Scholar]
|
| 2. |
Abbo L, Vincek V, Dickinson G, Shrestha N, Doblecki S, Haslett PA. Selective defect in plasmacyoid dendritic cell function in a patient with AIDS-associated atypical genital herpes simplex vegetans treated with imiquimod. Clin Infect Dis 2007;44:e25-7.
[Google Scholar]
|
| 3. |
Carrasco DA, Trizna Z, Colome-Grimmer M, Tyring SK. Verrucous herpes of the scrotum in a human immunodeficiency virus-positive man: Case report and review of the literature. J Eur Acad Dermatol Venereol 2002;16:511-5.
[Google Scholar]
|
| 4. |
Gilbert J, Drehs MM, Weinberg JM. Topical imiquimod for acyclovir-unresponsive herpes simplex virus 2 infection. Arch Dermatol 2001;137:1015-7.
[Google Scholar]
|
| 5. |
Sauder DN. Immunomodulatory and pharmacologic properties of imiquimod. J Am Acad Dermatol 2000;43(1 Pt 2):S6-11.
[Google Scholar]
|
| 6. |
Brummitt CF. Imiquimod 5% cream for the treatment of recurrent, acyclovir-resistant genital herpes. Clin Infect Dis 2006;42:575.
[Google Scholar]
|
| 7. |
Yudin MH, Kaul R. Progressive hypertrophic genital herpes in an HIV-infected woman despite immune recovery on antiretroviral therapy. Infect Dis Obstet Gynecol 2008;2008:592532.
[Google Scholar]
|
| 8. |
Perkins N, Nisbet M, Thomas M. Topical imiquimod treatment of aciclovir-resistant herpes simplex disease: Case series and literature review. Sex Transm Infect 2011;87:292-5.
[Google Scholar]
|
| 9. |
Lascaux AS, Caumes E, Deback C, Melica G, Challine D, Agut H, et al. Successful treatment of aciclovir and foscarnet resistant herpes simplex virus lesions with topical imiquimod in patients infected with human immunodeficiency virus type 1. J Med Virol 2012;84:194-7.
[Google Scholar]
|
| 10. |
Tangjitgamol S, Loharamtaweethong K, Thawaramara T, Chanpanitkitchot S. Vulvar pseudoepitheliomatous hyperplasia associated with herpes simplex virus type II mimicking cancer in an immunocompromised patient. J Obstet Gynaecol Res 2014;40:255-8.
[Google Scholar]
|
| 11. |
Deza G, Martin-Ezquerra G, Curto-Barredo L, Villar García J, Pujol RM. Successful treatment of hypertrophic herpes simplex genitalis in HIV-infected patient with topical imiquimod. J Dermatol 2015;42:1176-8.
[Google Scholar]
|
Fulltext Views
7,693
PDF downloads
2,811





