Translate this page into:
Extensive larva migrans
Correspondence Address:
S D Shenoi
Dept of Skin and STD, Kasturba Medical College, Manipal - 576104, Karnataka
India
| How to cite this article: Mehta V, Shenoi S D. Extensive larva migrans. Indian J Dermatol Venereol Leprol 2004;70:373-374 |
Abstract
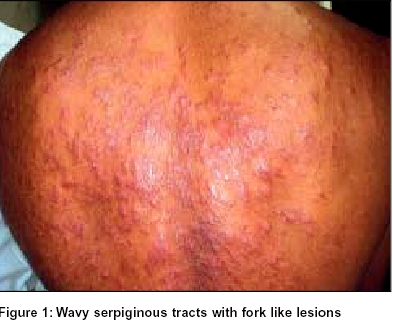
Larva migrans is characterized by tortuous migratory lesions of the skin caused by larvae of nematodes. A 26-year-old fisherman presented to us with complaints of an itchy eruption on his back and arms of two months' duration. Clinical examination revealed multiple wavy serpentine tracts and fork like lesions with a raised absolute eosinophil count of 3800 cells/cmm. Biopsy was inconclusive. This case is reported to highlight the extensive involvement by larva migrans.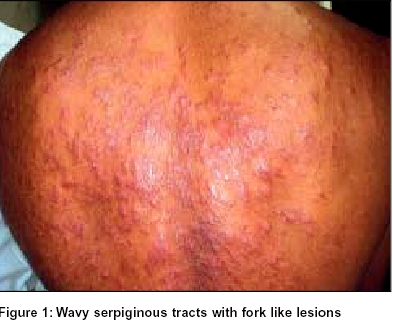 |
 |
INTRODUCTION
Cutaneous larva migrans is a common tropically acquired dermatosis. It presents as an erythematous, serpiginous, pruritic, cutaneous eruption caused by percutaneous penetration and subsequent migration of larvae of various nematode parasites.
CASE REPORT
A 26-year-old male came with complaints of an itchy eruption on his back and arms of 2 months′ duration. He was a fisherman by occupation and gave a history of sleeping on the beach for long hours. He was treated with antihistamines, but without any response. Cutaneous examination revealed multiple erythematous papules, plaques and wavy serpentine tracts on the back and posterior aspect of arms [Figure - 1].
The baseline laboratory parameters were normal, with a raised absolute eosinophil count of 3800 cell/cmm. A biopsy from the lesion showed only spongiosis with exocytosis. Based on the history and clinical findings a diagnosis of extensive larva migrans was considered. Treatment with albendazole 400 mg twice daily for a week led to complete resolution of lesions on the back and arms.
DISCUSSION
Larva migrans, also known as creeping eruption or sandworm eruption, is characterized by tortuous migratory lesions of the skin caused by larvae of nematodes.[1] It is seen in tropical and subtropical areas. International travel and increasingly exotic diets have resulted in an increase in cases of cutaneous larva migrans in industrialized countries.[2] Ankylostoma braziliensis, A. caninum, Uncinaria stenocephala, Gnathostoma species are commonly implicated in its causation. It occurs when the larvae of cat or dog hookworm penetrate the intact exposed skin and migrate through the epidermis progressing at the rate of few millimeters to about 3 cm/day.
The incubation period ranges from 1 to 6 days. An intensely itchy, bizarre, serpentine eruption appears most commonly on the feet but the back, buttocks, and abdomen may also be affected. Eosinophilic pustular folliculitis may also be associated with the serpentine eruption.[3] Larva migrans occurring over the penis,[4] oral mucosa and in an infant have also been reported. If a large number of larvae are active at the same time a series of disorganized loops and tortuous tracts are seen, as in our case. Dermatitis may occur due to scratching and secondary bacterial infection. The disease is self limiting as the larvae eventually die in 2-8 weeks. Diagnosis is established by the typical clinical features. Biopsy is of no utility in diagnosis as larvae advance ahead of the serpiginous tract. Cryotherapy with liquid nitrogen, oral ivermectin, albendazole and thiabendazole[5] are useful treatments. Topical albendazole ointment has also been tried for cutaneous larva migrans in young children.[6]
| 1. |
Bryceson AD, Hay RJ. Parasitic worm and protozoa. In: Champion RH, Burton JL, Ebling FJG, editors. Rook/Wilkinson/Ebling Textbook of Dermatology. 5th Ed. Oxford: Blackwell; 1992. p. 1217-64.
[Google Scholar]
|
| 2. |
Gillispie SH. Cutaneous larva migrans. Curr Infect Dis Rep 2004;6:50-3.
[Google Scholar]
|
| 3. |
Opie KM, Heenan PJ, Delaney TA, Rohr JB. Two cases of eosinophilic pustular folliculitis associated with parasitic infections. Australas J Dermatol 2003;44:217-9.
[Google Scholar]
|
| 4. |
Kartikeyan K, Thappa DM, Jeevankumar B. Cutaneous larva migrans of the penis. Sex Transm Infect 2003;79:500.
[Google Scholar]
|
| 5. |
Gourgiotou K, Nicolaidou E, Panagiotopoulos A, Hatziolou JE, Katsambast AD. Treatment of widespread cutaneous larva migrans with thiabendazole. J Eur Acad Dermatol Venerol 2001;15:578-80.
[Google Scholar]
|
| 6. |
Caumes E. Efficacy of albendazole ointment on cutaneous larva migrans in 2 young children. Clin Infect Dis 2004;38:1647-8.
[Google Scholar]
|
Fulltext Views
2,429
PDF downloads
1,416





