Extra-mammary Paget’s disease of the axilla: A rare occurrence
Corresponding author: Prof. Archana Singal, Department of Dermatology and STD, University College of Medical Sciences and GTB Hospital, Delhi, India. archanasingal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal S, Bisherwal K, Singal A, Tanveer N, Kumar PS, Agrawal H. Extra-mammary Paget’s disease of the axilla: A rare occurrence. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1322_2024
Dear Editor,
Extra-mammary Paget’s disease (EMPD) is an uncommon intraepithelial adenocarcinoma with a predilection for apocrine gland-rich areas like vulva, penis, scrotum, axilla, and occasionally eyelids.1 We present a rare case of EMPD involving axilla in a woman with a brief review of the literature.
A 40-year-old woman presented with a single, asymptomatic, gradually progressive, erythematous plaque in the left axilla of 12-year duration with no systemic complaints. Cutaneous examination revealed a solitary, well-demarcated, non-tender, and firm plaque of size 4×3 cm over the left axilla with scaling and fissuring over the central area and peri-lesional hyperpigmentation [Figure 1a]. Bilateral breasts and contralateral axillary examination were normal. Differential diagnoses of inverse psoriasis, hypertrophic lichen planus and lupus vulgaris were considered. Dermoscopy of the plaque (Dinolite AM 7515 MZT dermatoscope) showed multiple white structureless areas on a pinkish background with superficial white scales [Figure 1b] and multiple white shiny lines interspersed with glomerular vessels [Figure 1c]. Ultrasonography of both breasts and axilla was unremarkable. Lesional skin biopsy demonstrated hyperkeratosis with single and small clusters of round to oval atypical cells in the epidermis. These cells had abundant pale, amphophilic cytoplasm with large irregular nuclei and conspicuous nucleoli with few mitotic figures. At a few places, these cells formed ill-defined glands. No melanin could be identified. The dermis showed mild inflammation with no identifiable tumour [Figure 2a]. The tumour cells showed strong membranous immunopositivity for cytokeratin-7 (CK7), epithelial membrane antigen (EMA), Her-2-neu, and elevated Ki-67 labelling index [Figure 2b]. Based on histopathology and immunohistochemistry findings, a final diagnosis of EMPD was made and wide local excision was performed. Histopathology of the excised lesion showed 7 mm of tumour-free margins. There was no evidence of recurrence at the 6-month follow-up visit [Figure 3].

- A solitary, well-demarcated plaque over the left axilla with peripheral hyperpigmentation, scaling, and fissuring over the central area.
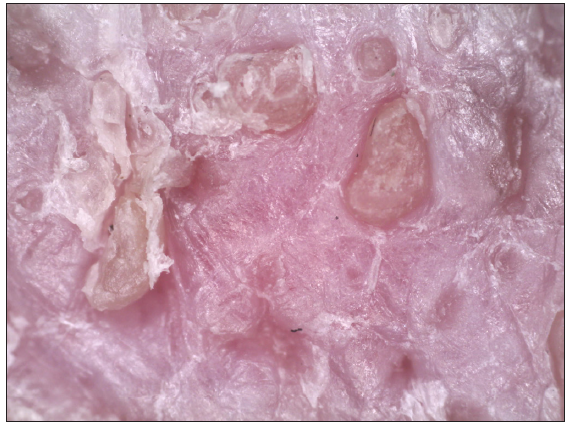
- Dermoscopy of the lesion showing multiple white structureless areas on a pinkish background with multiple superficial white scales (Dermlite DL4, Non-polarised, 10x magnification).
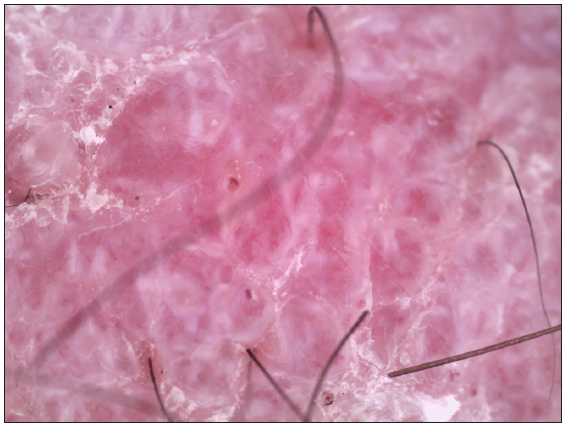
- Polarised dermoscopy of the lesion showing multiple white shiny lines with glomerular vessels (Dermlite DL4, polarised, 10x magnification).
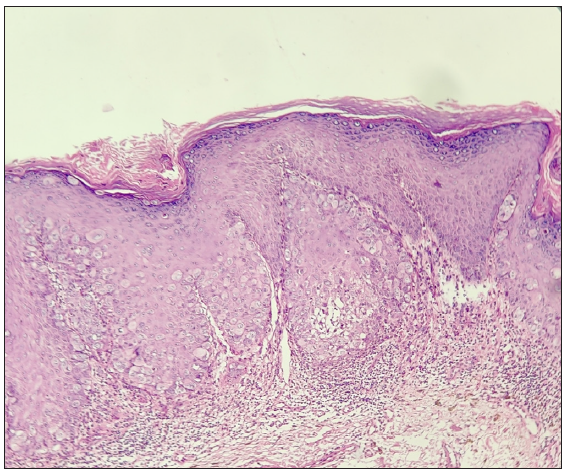
- Epidermis showing multiple, round to oval atypical cells with abundant amphophilic cytoplasm and conspicuous nucleoli. Few mitotic figures are also seen. (Haematoxylin and eosin, 10x).
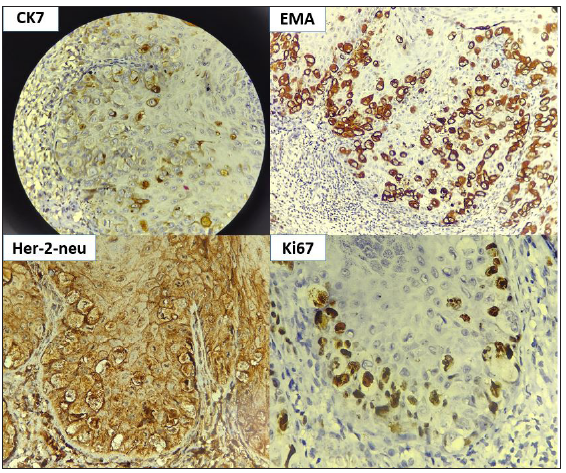
- Immunohistochemistry (IHC) showing cells with positivity for CK7, epithelial membrane antigen (EMA), Her-2-neu, and elevated Ki67 (IHC, 40x).
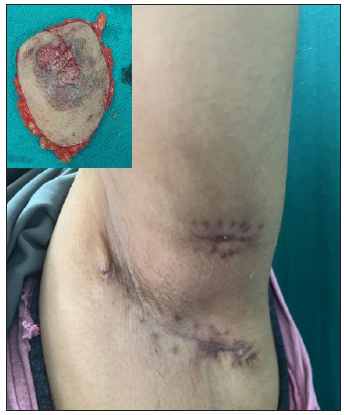
- Image of the patient at 3 months post-surgery. Inset showing excised specimen.
EMPD comprises 6.5% of all cases of Paget’s disease, axillary involvement reported in only 0.9% cases.2,3 Though the exact incidence of axillary EMPD remains unknown, Zhao et al. reported an incidence of 5.3% (16/303) in their case series over a period of 10 years with an average age of 63.9 years (40–80 years)3 at diagnosis and a female preponderance in patients with isolated axillary involvement (F: M=1.3:1).1,3,4
The most accepted theory for EMPD is multicentric theory which states that oncogenic stimulus can generate intraepidermal and adnexal adenocarcinoma.
Clinically, EMPD presents with asymptomatic, erythematous plaques with erosion, verrucous hyperplasia, dyspigmentation, and occasionally pruritus. Differential diagnoses include psoriasis, lichen planus, Bowen’s disease, eczema, and superficial spreading melanomas. Dermoscopy can help clinical diagnosis. Mun JH et al. have published the dermoscopic characteristics of 35 patients with EMPD, but only one had axillary involvement.5 Some of our dermoscopic findings (structureless white areas, shiny white lines, and glomerular vessels) were consistent with this study.
The presence of underlying carcinoma in axillary EMPD has been reported in 35% (8/23) cases (breast, apocrine adenocarcinoma, and squamous cell carcinoma). Our case did not show any features of underlying malignancy.
Histopathological evidence of Paget cells (large atypical cells with central nuclei and abundant cytoplasm with nuclear atypia) confirms the diagnosis.2 Immunohistochemistry shows positive staining for CK7, CEA, CAM5.2 and GCDFP15 and negative staining for S100, CK20 and melanocytic markers. The main differential diagnoses of Paget’s disease (both mammary and extra-mammary) include Bowen’s disease and melanoma in situ. While Bowen’s disease would show individual cell keratinisation and immunonegativity for CK7 and Her-2-neu, melanoma in situ would show CK7 immunonegativity and immunopositivity for HMB-45 along with melanin pigment in tumour cells.
Management options for EMPD include wide local excision, Mohs’ micrographic surgery (MMS), topical and systemic chemotherapy, laser therapy, and radiotherapy. MMS is preferred due to lower recurrence rates.3 Axillary lesions have shown clear margins within 1 cm of excision in 76.5% of cases.3 In our case, wide local excision was performed due to the unavailability of MMS with 7 mm of tumour-free margins. The prognosis of axillary EMPD is usually favourable with no recurrences post-surgery on follow-up of 6–166 months irrespective of the presence of underlying carcinoma due to well-defined and clear anatomy of the axillary region. However, recurrences have been noted in genital (32–50%) and perianal (50–70%) EMPD after local resection.1,3
EMPD of axilla poses a diagnostic dilemma due its unusual location. A high index of suspicion is necessary, especially in patients with long-standing chronic eczematous lesion. Further studies are needed to validate the dermoscopic findings. Screening for internal malignancies and early diagnosis can lead to prompt treatment and a favourable prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Extramammary Paget’s disease of the unilateral axilla: A review of seven cases in a 20-year experience. Int J Dermatol. 2011;50:157-60.
- [CrossRef] [PubMed] [Google Scholar]
- Extramammary Paget’s disease of the axilla: A case report and a review of literature. Int J Clin Exp Pathol. 2017;10:7107-111. Available from: https://ijcep.com/files/ijcep0050312.pdf
- [Google Scholar]
- Extramammary Paget’s disease involving the axilla: Case series and literature review. Int J Dermatol. 2023;62:933-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pigmented extramammary Paget’s disease of the axilla mimicking melanoma: Case report and review of the literature. J Cutan Pathol. 2009;36:995-1000.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical and dermoscopic characteristics of extramammary Paget disease: A study of 35 cases. Br J Dermatol. 2016;174:1104-7.
- [CrossRef] [PubMed] [Google Scholar]





