Translate this page into:
Extrafacial lupus miliaris disseminatus faciei: A rare entity
Corresponding Author:
Yogesh Namdev Kalyanpad
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai - 400 012, Maharashtra
India
yogesh.kalyanpad@gmail.com
| How to cite this article: Kalyanpad YN, Dongre AM, Gole PV, Khopkar US. Extrafacial lupus miliaris disseminatus faciei: A rare entity. Indian J Dermatol Venereol Leprol 2017;83:354-357 |
Sir,
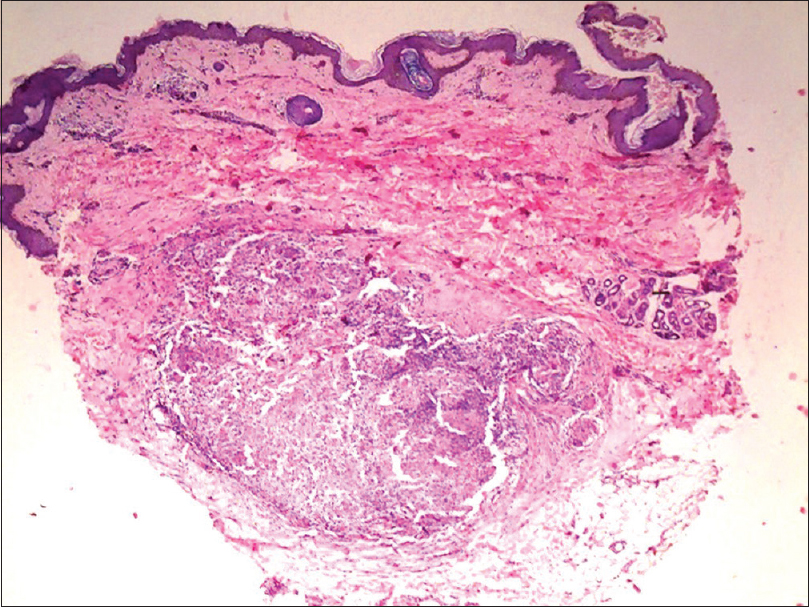
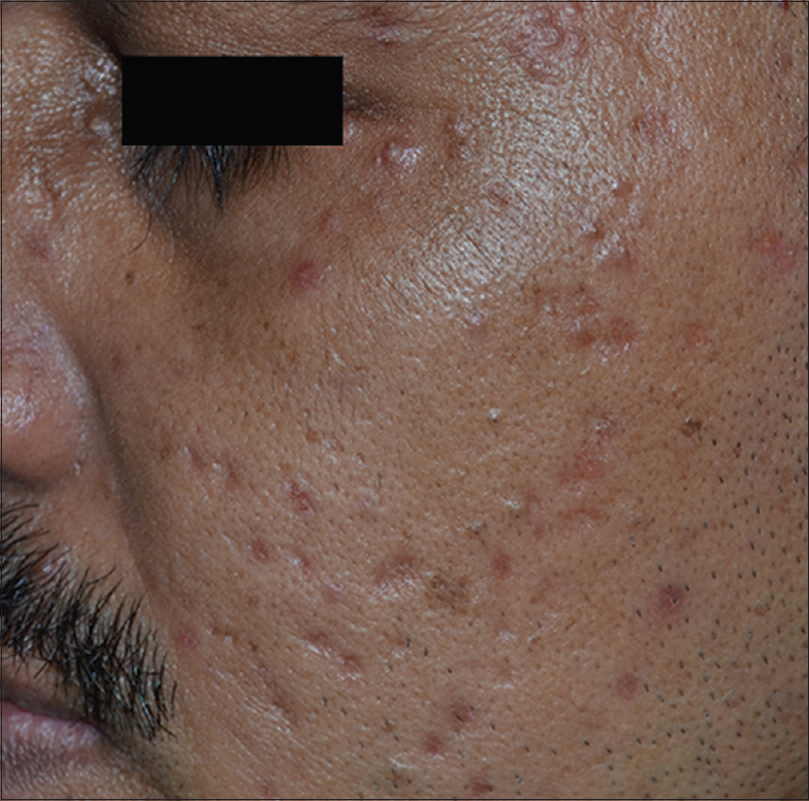
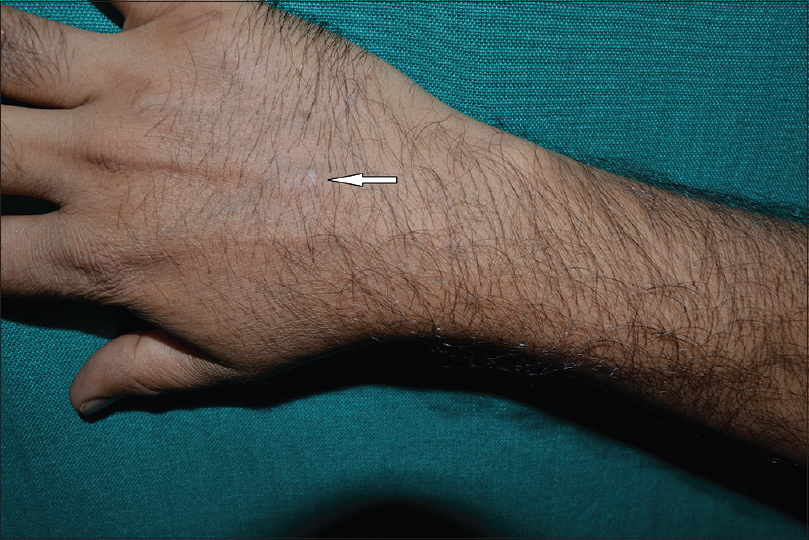
A 32-year-old man presented with multiple, asymptomatic, erythematous papules on the face for 6 months. The lesions gradually increased in size and number to involve the neck and both forearms over the last 2 months. There were no systemic symptoms. Examination showed multiple, discrete, non-tender, symmetrical, reddish-brown papules on the forehead, both cheeks, neck and eyelids [Figure - 1]. Erythematous papules and nodules were also present on the dorsum of the hands and extensor aspect of the forearms [Figure - 2]. There was no regional lymphadenopathy. Blood investigations such as complete blood count, erythrocyte sedimentation rate and hepatic and renal function tests were normal. Chest X-ray was normal and Mantoux test was negative.
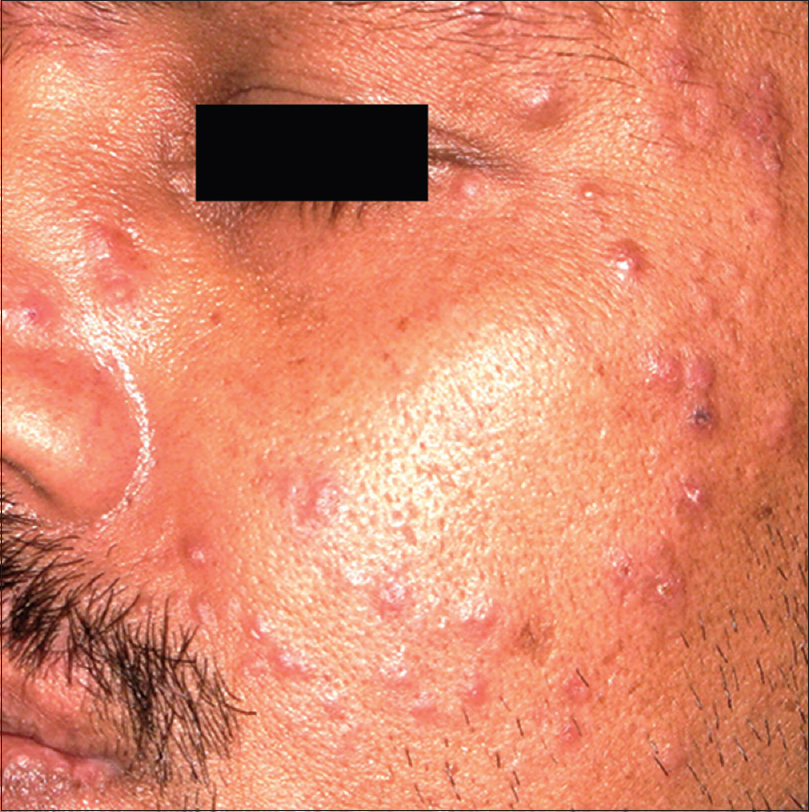 |
| Figure 1: Multiple, discrete, non-tender reddish-brown papules on the cheeks, forehead, nose and eyelids |
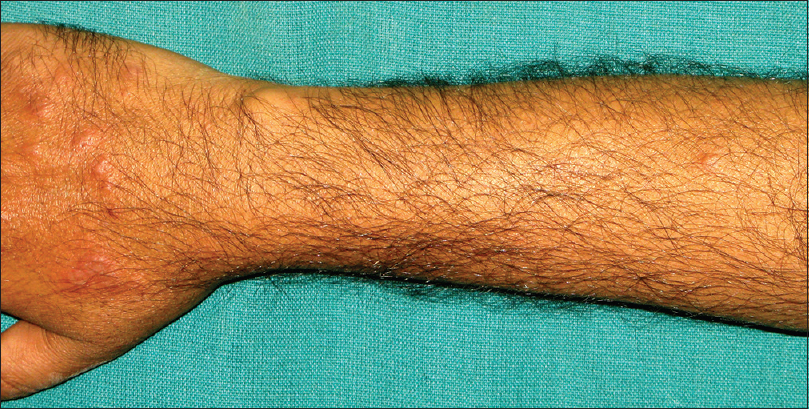 |
| Figure 2: Erythematous papulonodular lesions on the dorsum of hands and few on the extensor forearm |
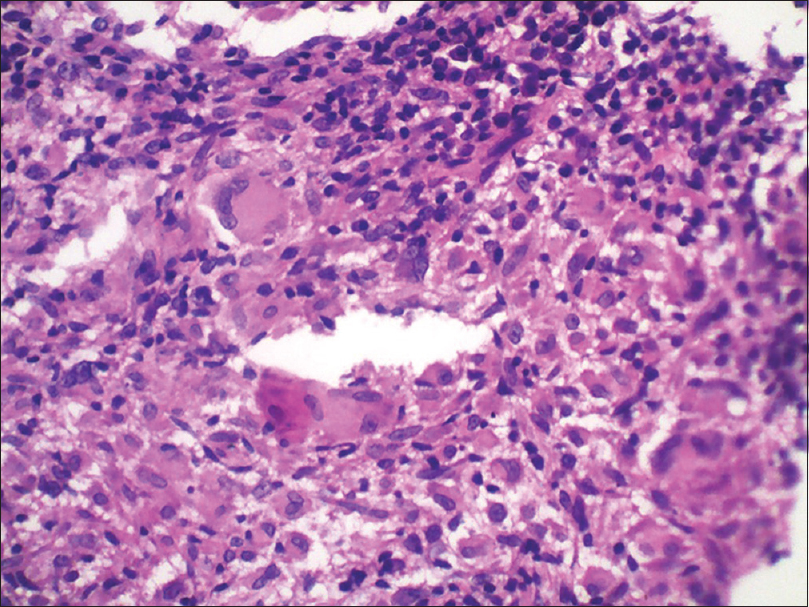
Biopsy was taken from a facial lesion as well as a lesion on the forearm. Histopathology of lesion from face showed central areas of caseation necrosis in the dermis with surrounding tuberculoid granulomatous infiltrate consisting of histiocytes, epithelioid cells, giant cells and lymphocytes [Figure - 3] and [Figure - 4]. Biopsy from the papule on the forearm showed similar histological features as seen in facial lesion [Figure - 5] and [Figure - 6]. Special stains for tubercle bacilli were negative. The patient was treated with doxycycline leading to resolution of the lesions leaving behind pitted scars over a period of 3 months of treatment [Figure - 7] and [Figure - 8].
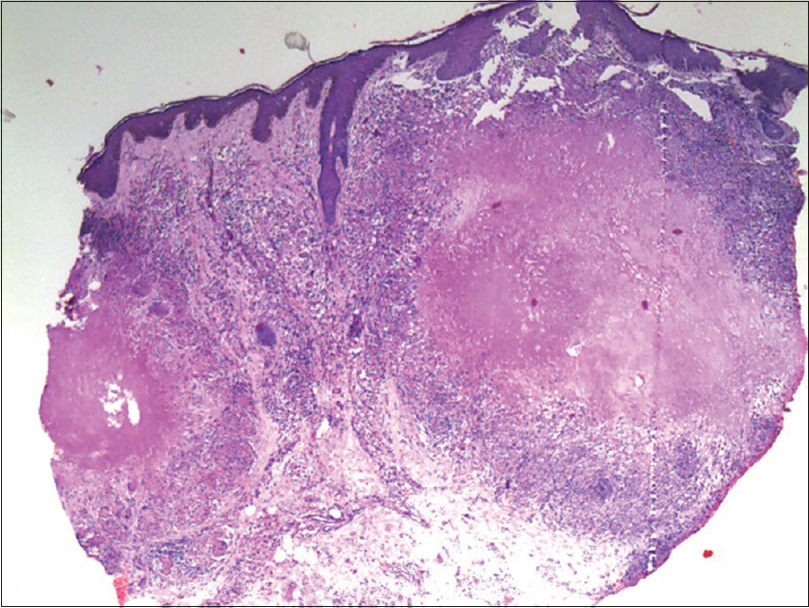 |
| Figure 3: Biopsy from facial papule showed epidermal hyperplasia with caseation necrosis and granulomatous infiltrate in the dermis (H and E, ×100) |
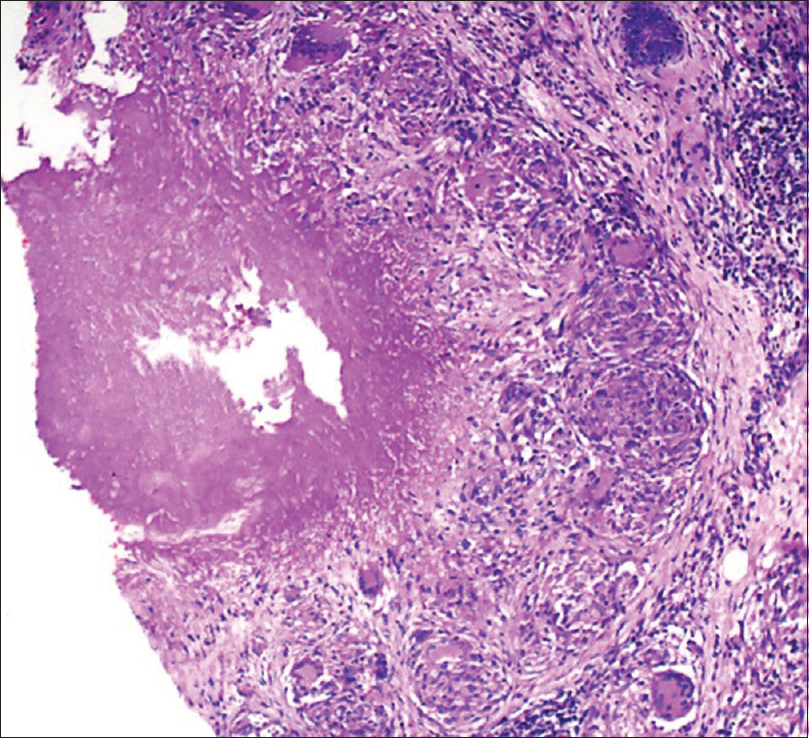 |
| Figure 4: Higher magnification showed caseation necrosis surrounded by tuberculoid granulomas consisting of histiocytes, epithelioid cells, giant cells and lymphocytes (H and E, ×200) |
 |
| Figure 5: Histopathology of the lesion on the forearm showing foci of caseation necrosis with granulomatous infiltrate in mid and deep dermis (H and E, ×100) |
 |
| Figure 6: Caseation necrosis surrounded by granulomas consisting of epithelioid cells, giant cells and lymphocytes (H and E, ×200) |
 |
| Figure 7: Lesions resolving with multiple varioliform scars with some papules in periorbital region |
 |
| Figure 8: Resolution of lesions with scarring on the dorsum of the right hand |
Lupus miliaris disseminatus faciei is an uncommon, chronic, inflammatory dermatosis characterized by multiple, monomorphic, symmetrical, reddish-brown papules on chin, forehead, cheeks and eye lids. The lesions usually regress spontaneously within months to some years leaving behind depressed scars.
Histopathologically, it is characterized by a dermal granulomatous infiltrate with a central area of caseation necrosis. Histopathological findings range from perivascular and periadnexal lymphohistiocytic infiltrate in early lesions and epithelioid cell granuloma with or without central necrosis in well-developed lesions. Late lesions show extensive perifollicular fibrosis with non-specific cell infiltration.
The exact etiopathogenesis of this condition is unclear. Earlier it was thought to be a “tuberculid,” but it is no longer thought to be of tuberculous origin. It is hypothesized that the condition is due to immune response to the follicular antigens that are released due to damage to the hair epithelium, triggering an autoimmune reaction directed against hair-follicles. Other authors consider it to be a variant of granulomatous rosacea due to the centrofacial distribution and granulomatous histopathology. However, some believe that it is an entity distinct from either skin tuberculosis or granulomatous-type rosacea and propose to change its name to “facial idiopathic granulomas with regressive evolution.”[1]
Various treatments have been advocated and these include tetracycline, prednisolone and isotretinoin. Isoniazid and dapsone have also been reported to be useful.[2]
Face is a common site for lupus miliaris disseminatus faciei lesions and extrafacial involvement is rarely seen, with only a few reports of the latter. Extrafacial sites reported include axillae, neck, scalp, legs, trunk and genitalia. Kou et al. have described extrafacial distribution of lesions without face involvement.[3]
Nath et al. have reported the extensive involvement of the face with unusual linvolvement of the ear lobes, neck and the shoulder girdle in an Indian patient.[4] A case of extrafacial lupus miliaris disseminatus faciei alongwith Morbihan disease and with axillary acneagminata has been reported.[3] However, in our patient, these associations were not seen. Bedlow has described a case of two adults with involving axillae with no facial lesions.[5]
We report this case to emphasize the relatively rare extrafacial distribution of lupus miliaris disseminatus faciei involving the dorsae of hands and forearms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Skowron F, Causeret AS, Pabion C, Viallard AM, Balme B, Thomas L. F.I.GU.R.E.: Facial idiopathic granulomas with regressive evolution. Is 'lupus miliaris disseminatus faciei' still an acceptable diagnosis in the third millennium? Dermatology 2000;201:287-9. [Google Scholar] |
| 2. | Kumano K, Tani M, Murata Y. Dapsone in the treatment of miliary lupus of the face. Br J Dermatol 1983;109:57-62. [Google Scholar] |
| 3. | Kou K, Chin K, Matsukura S, Sasaki T, Nozawa A, Aihara M, et al. Morbihan disease and extrafacial lupus miliaris disseminatus faceie: A case report. Ann Saudi Med 2014;34:351-3. [Google Scholar] |
| 4. | Nath AK, Sivaranjini R, Thappa DM, Basu D. Lupus miliaris disseminatus faciei with unusual distribution of lesions. Indian J Dermatol 2011;56:234-6. [Google Scholar] |
| 5. | Bedlow AJ, Otter M, Marsden RA. Axillary acne agminata (lupus miliaris disseminatus faciei). Clin Exp Dermatol 1998;23:125-8. [Google Scholar] |
Fulltext Views
3,753
PDF downloads
2,285





