Translate this page into:
Extramammary Paget's disease: Analysis of 17 Chinese cases
Correspondence Address:
Quanzhong Liu
154 An Shan Road, Tianjin - 0086 300052
China
| How to cite this article: Qi Y, Hu J, Sun C, Zhang J, Liu Q. Extramammary Paget's disease: Analysis of 17 Chinese cases. Indian J Dermatol Venereol Leprol 2014;80:129-133 |
Abstract
Background/Objective: Extramammary Paget's Disease (EMPD) seems to be more common in Caucasians than Chinese. We report the clinical manifestations, management, and prognostic characteristics in 17 Chinese patients. Methods: Medical records and biopsies of 17 patients who had been treated at a large university hospital in China between March 2005 and January 2012 were reviewed. Results: Of the 17 patients, 14 were men. They had lesions on the scrotum and the penis. Of the three women, two had vulvar and one had inguinal lesions. All patients underwent Mohs micrographic surgery (MMS). Three men had metastasis to the inguinal lymph nodes and underwent an extensive local excision with inguinal lymphadenectomy. Eight patients who had positive excision margins received additional radiation therapy. The mean follow-up duration was 54 months (4-85 months). One patient had two recurrences. Three had metastasis to the inguinal lymph node. One had metastasis to the bone and concomitant prostate cancer. Two patients died of the disease. Conclusion: A striking difference in presentation of EMPD in Chinese compared with Caucasians is the male predominance and location on the penis and scrotum. Mohs micrographic surgery followed by radiotherapy is an effective treatment. Long-term follow-up suggests that the disease has a good prognosis when it does not metastasise.Introduction
Extramammary Paget′s disease (EMPD) was originally described by Crocker [1] in 1989 in a male patient in whom there was involvement of the scrotum and penis. It is a rare neoplastic condition of apocrine gland-bearing skin and usually presents around age 50 and older. It seems to be more common in Caucasians and affects mostly women. It is very rare in men. [2] It is generally slow growing and the most commonly affected sites are the vulva, perineum, perianal region, scrotum, penis, or pubic area. [3] The diagnosis is often delayed because the common presenting eczema-like symptoms and pruritus are relatively nonspecific and attributed to benign disease. [4 ] The disease is notorious for its chronic relapsing clinical course attributed to its probable multicentric nature and frequently positive surgical margins following excision. Moreover, there is a lack of concordance between the visible lesion and the actual extent of the disease. [5] Therefore, Mohs micrographic surgery (MMS) has theoretical advantages because this tumor has clinically indistinct margins and subclinical extensions. [6] The objective of this study was to analyze the clinical characteristics, treatment, and follow-up in patients with extramammary Paget′s disease seen in our institution between March 2005 and January 2012, and to compare the results with those found in Caucasians.
Methods
From March 2005 to January 2012, we treated 17 patients with extramammary Paget′s disease. Before treatment, all cases were confirmed by biopsy [Figure - 1]. All patients underwent Mohs micrographic surgery for treatment. We took a 1.5-2 cm margin for the first frozen sections and proceeded to further stages according to the pathology results. During Mohs micrographic surgery, we removed a clinically suspicious regional lymph node, if present, for examination. Subsequent lymph node dissection was performed if there was evidence of nodal involvement. Reconstruction was performed by rotation flap, advancement flap, or primary closure in situ [Figure - 2]. The patients with positive margins received radiation therapy after surgery.
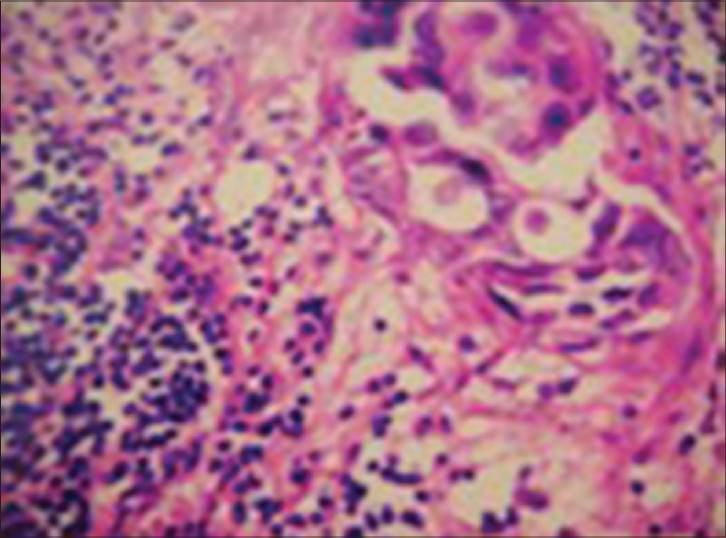 |
| Figure 1: Typical histopathological features of EMPD |
 |
| Figure 2a-c: Surgical reconstructions by rotation fl ap, advancement fl ap or primary closure in situ |
All participants were followed-up at the outpatient department or through individual telephone contact. Patients were followed up every 3-6 months. Routine surveillance biopsies were not performed in asymptomatic patients; however, any change in the clinical appearance prompted further investigations, including a detailed examination and consideration for punch biopsy.
All patients had analysis of full blood cells counts, renal function, hepatic enzymes, biochemical analysis, and urinalysis. In addition, they were checked for occult neoplasms by chest radiography, abdominal, and urinary tract ultrasound.
Results
All 17 patients with extramammary Paget′s disease [Table - 1] were Chinese. There were 14 males and 3 females. The mean age at diagnosis was 61 years (range: 33-76 years). The women presented with disease in the vulva (two cases) and groin (one case). The men presented with disease on the scrotum (three cases); penis (two cases), scrotum and penis (eight cases); and scrotum, penis, and groin (one case). In most patients, there was a long delay from the onset of symptoms to diagnosis; the mean time between the initial lesion and the first consultation was 4.5 years (range: 1 month - 15 years).
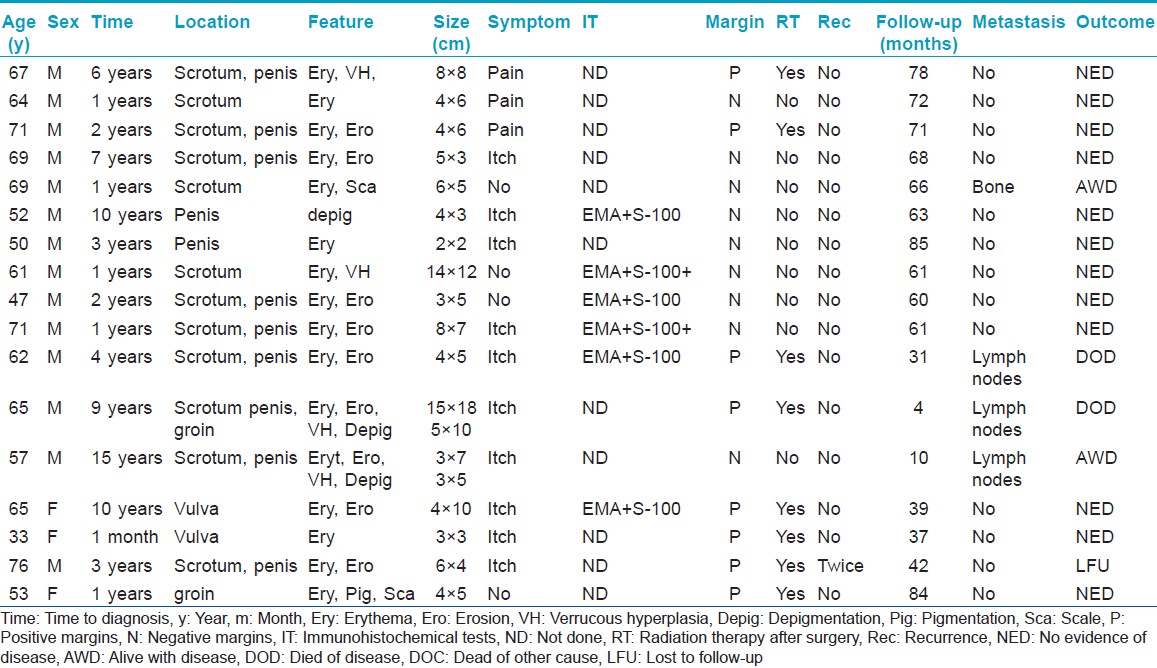
The most common symptom was itch in 10 cases, three cases felt pain and four cases had no specific sensory symptoms. A visible lesion, typically an erythematous plaque, was present in every patient. Four of 17 patients showed verrucous hyperplasia, three showed depigmentation and one showed hyperpigmentation [Figure - 3]. The greatest dimension of the lesion ranged from 2-18 cm (mean 7 cm). Fourteen patients had a single lesion and three had two lesions Immunohistochemical tests were performed in six patients: six showed EMA positivity and two showed S-100 positivity. CK7, CK20, and GCDFP-15 were not tested in any patient.
 |
| Figure 3a-c: Clinical presentations of our patients with extramammary Paget's disease |
All patients underwent Mohs micrographic surgery for treatment. At the first round with a 1.5-2 cm margin, 14 cases still had histologically positive margins. Further excision was undertaken to achieve a negative margin. One patient who was still positive after the first round with 2 cm lateral margins needed two additional rounds with a 1 cm margin. Because the excised area of some patients became too large, eight (47%) patients who were still surgical margin-positive received radiation therapy after surgery. Of these eight, two had lymph node metastases.
The average length of follow-up was 54 months (range: 4-85). One (5.9%) patient experienced two episodes of recurrence after the first resection; the first recurrence was at 11 months while the second recurrence was at 37 months. Four cases (24%) had metastases: Three (18%) had lymph node metastases; one (5.9%) had bone metastasis with concomitant malignancy (prostate cancer).
In 12 patients (71%), there was no evidence of disease on the last date of follow-up, two patients (12%) were alive with disease, one patient (5.8%) was lost to follow-up while two patients died from extramammary Paget′s disease during the follow-up period. Thus, the extramammary Paget′s disease-related death rate was 11.8%.
Discussion
Extramammary Paget′s disease is a rare neoplastic lesion which is more frequently seen in Caucasians and rarely seen in blacks. In Caucasian patients, a female predominance has been reported, with a female-to-male ratio of 4:1 and a mean age of 65. [1],[2],[3],[4] In our study, we noted a male predominance (82%) with an almost similar mean age of 60. This male predominance (69-100%) is also reported in other Asian publications from China, Japan, and Korea. [8],[9],[10] Extramammary Paget′s disease also appears to be much more common in Asia than previous reports about the occurrence in Caucasians would indicate. There are various possibilities to explain this difference: (1) Because of the large populations in Asia extramammary Paget′s disease is more frequently seen in dermatology departments. In the literature, we were unable to find reports on the population prevalence of extramammary Paget′s disease. (2). In China patients with serious diseases are more likely to attend university hospitals. (3). Differences in concepts of health, cultural attitudes, and the healthcare referral system from Western countries. (4). Different genotypes and related gene expressions in different races may play a role. The molecular pathogenesis of extramammary Paget′s disease may be associated with overexpression of Sp1, P53, MAPK, p-AKT, p-Stat3, Stat5a, p-ATF2, NGF, BDNF, and their high-affinity receptors. [11],[12],[13],[14],[15]
In our study, one female was only 33 years old raising the possibility of mammary Paget′s disease that, in contrast to extramammary Paget′s disease, is occasionally reported at a relatively young age. [12] However, our patient did not have mammary Paget′s disease and no other signs of breast cancer. There are antigenic differences between primary intra-epidermal Paget′s disease (CK7 positive, CK20 negative, GCDFP-15 positive) and Paget′s disease that has spread from an associated internal carcinoma (CK7 positive, CK20 positive, GCDFP-15 negative) [16] Unfortunately, we did not undertake these immunohistochemical tests.
Extramammary Paget′s disease usually progresses slowly, and in our study the mean time until the diagnosis was 4.5 years. Because of the nonspecific presentation the diagnosis is easily missed or delayed and many patients are too shy to seek early medical help.
There is still no effective treatment for extramammary Paget′s disease. The mainstay of treatment is wide surgical excision on both the surface and deeply. [17],[18],[19] Nevertheless, the disease is notorious for its high recurrence rate, ranging between 12% and 58%, with an average of 33%. Mohs micrographic surgery is a surgical technique performed in cases with a high risk of recurrence. In this procedure, between 1 and 10 mm of tumor margin is resected depending on the tumor type and the estimated extent of subclinical spread. [20] Mohs micrographic surgery is the only method that enables surgeons to confirm the clearance of the entire margin of the tumor. The effectiveness of intraoperative frozen section evaluation of the surgical margins in obtaining negative permanent margins and reducing recurrence rate is controversial. [19],[21] There is no standardized procedure for determining tumor margins prior to removing the first stage during Mohs micrographic surgery. Some Mohs surgeons perform light curettage of the tumor, which not only debulks the friable tumor tissue to facilitate tissue processing, but more importantly, can potentially help delineate its margins. [22]
In our study, all patients underwent Mohs micrographic surgery. Our pathology results indicated that excision of 2-3 cm of uninvolved lateral margins may not be sufficient in extramammary Paget′s disease which has a multicentric origin and satellite lesions.
The patients who had positive margins after a large excision received radiation therapy. We assumed that this adjunct local radiotherapy postoperatively reduces the recurrence rate.
Because the recurrence rate (5.8%) was low in our study, our treatment protocol appears more effective than traditional excision. The presence of Paget cells in the surgical margin did not predict disease recurrence in our study, as only one out of eight such patients had a recurrence.
Conservative approaches to extramammary Paget′s disease have been studied, including radiotherapy, CO2 laser, topical imiquimod 5%, topical 5-fluorouracil, bleomycin, imiquimod, and, more recently, photodynamic therapy. [23],[24],[25],[26],[27],[28] In our opinion, surgical modalities should be considered to be the first choice for extramammary Paget′s disease treatment until randomized studies with adequate follow-up have evaluated the non-surgical treatments.
Usually, the prognosis of extramammary Paget′s disease is poor. Poor prognostic factors include dermal invasion or metastasis via the lymphatic system. [7],[29] Lymph node metastasis in most cases involves inguinal, peri-rectal, retroperitoneal, iliac, and para-aortic lymph nodes. Distant metastasis involves predominantly the liver, bone, lung, and suprarenal glands. There were not many metastatic lesions in our study: 3 (17.6%) of our 17 patients had metastasis to the inguinal lymph nodes, of whom two died. Extramammary Paget′s disease is often accompanied by another internal malignancy, but in Asian patients this seems to be less common than in Caucasians. Only one of our patients had concomitant prostate cancer and had metastasis to the bone.
| 1. |
Crocker HR. Paget's disease affecting the scrotum and penis. Trans Pathol Soc Lond 1888-1889;40:187-91.
[Google Scholar]
|
| 2. |
Lam C, Funaro D. Extramammary Paget's disease: Summary of current knowledge. Dermatol Clin 2010;28:807-26.
[Google Scholar]
|
| 3. |
Barmon D, Kataki AC, Imchen L, Sharma JD. Extra mammary Paget's disease of the vulva. J Midlife Health 2012;3:100-2.
[Google Scholar]
|
| 4. |
Zhu Y, Ye DW, Yao XD, Zhang SL, Dai B, Zhang HL, et al. Clinicopathological characteristics, management and outcome of metastatic penoscrotal extramammary Paget disease. Br J Dermatol 2009;161:577-82.
[Google Scholar]
|
| 5. |
Kanitakis J. Mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol 2007;21:581-90.
[Google Scholar]
|
| 6. |
Lee KY, Roh MR, Chung WG, Chung KY. Comparison of Mohs micrographic surgery and wide excision for extramammary Paget's Disease: Korean experience. Dermatol Surg 2009;35:34-40.
[Google Scholar]
|
| 7. |
Chen Q, Chen YB, Wang Z, Cai ZK, Peng YB, Zheng DC, et al. Penoscrotal extramammary Paget's disease: Surgical techniques and follow-up experiences with thirty patients. Asian J Androl 2013;15:508-12.
[Google Scholar]
|
| 8. |
Zhang N, Gong K, Zhang X, Yang Y, Na Y. Extramammary Paget's disease of scrotum: Report of 25 cases and literature review. Urol Oncol 2010;28:28-33.
[Google Scholar]
|
| 9. |
Sawada Y, Bito T, Kabashima R, Yoshiki R, Hino R, Nakamura M, et al. Ectopic extramammary Paget's disease: Case report and literature review. Acta Derm Venereol 2010;90:502-5.
[Google Scholar]
|
| 10. |
Lee SJ, Choe YS, Jung HD, Ahn SK, Cha YC, Cho KH, et al. Korean Society for Skin Cancer and Korean Dermatopathology Research Group. A multicenter study on extramammary Paget's disease in Korea. Int J Dermatol 2011;50:508-15.
[Google Scholar]
|
| 11. |
Chen SY, Takeuchi S, Moroi Y, Hayashida S, Kido M, Uchi H, et al. Concordant over-expression of transcription factor Sp1 and vascular endothelial growth factor in extramammary Paget's disease. Int J Dermatol 2008;47:562-6.
[Google Scholar]
|
| 12. |
Liu H, Urabe K, Uchi H, Takeuchi S, Nakahara T, Dainichi T, et al. Expression and prognostic significance of Stat5a and E-cadherin in extramammary Paget's disease. J Cutan Pathol 2007;34:33-8.
[Google Scholar]
|
| 13. |
Lin N, Uchi H, Moroi Y, Fukiwake N, Dainichi T, Takeuchi S, et al. Expression of the p38 MAPK, NF-kappaB and cyclin D1 in extramammary Paget's disease. J Dermatol Sci 2007;45:187-92.
[Google Scholar]
|
| 14. |
Chen S, Moroi Y, Urabe K, Takeuchi S, Kido M, Hayashida S, et al. Differential expression of two new members of the P53 family, P63 and P73, in extramammary Paget's disease. Clin Exp Dermatol 2008;33:634-40.
[Google Scholar]
|
| 15. |
Qian Y, Takeuchi S, Chen SJ, Dugu L, Tsuji G, Xie L, et al. Nerve growth factor, brain-derived neurotrophic factor and their high-affinity receptors are overexpressed in extramammary Paget's disease. J Cutan Pathol 2010;37:1150-4.
[Google Scholar]
|
| 16. |
Reddy IS, Swain M, Gowrishankar S, Murthy DB. Primary extramammary Paget's disease with extensive skeletal metastases. Indian J Dermatol Venereol Leprol 2012;78:89-92.
[Google Scholar]
|
| 17. |
Wollina U. Extensive Invasive Extramammary Paget's Disease: Surgical Treatment. J Cutan Aesthet Surg 2013;6:41-4.
[Google Scholar]
|
| 18. |
Tanaka VD, Sanches JA, Torezan L, Niwa AB, Festa Neto C. Mammary and extramammary paget's disease: A study of 14 cases and the associated therapeutic difficulties. Clinics (Sao Paulo) 2009;64:599-606.
[Google Scholar]
|
| 19. |
Roh HJ, Kim DY, Kim JH, Kim YM, Kim YT, Nam JH. Paget's disease of the vulva: Evaluation of recurrence relative to symptom duration, volumetric excision of lesion, and surgical margin status. Acta Obstet Gynecol Scand 2010;89:962-5.
[Google Scholar]
|
| 20. |
Asilian A, Momeni I. Comparison between examination with naked eye, curretage and dermoscopy in determining tumor extension before Mohs micrographic surgery. Adv Biomed Res 2013;2:2.
[Google Scholar]
|
| 21. |
Fujii M, Terashi H, Hashikawa K, Tahara S. Functional reconstruction of large anogenital defects with bilateral V-Y advancement posterior thigh fasciocutaneous flaps. J Plast Reconstr Aesthet Surg 2007;60:1208-13.
[Google Scholar]
|
| 22. |
Asgari M, Olson J, Alam M. Needs assessment for mohs micrographic surgery. Dermatol Clin 2012;30:167-75.
[Google Scholar]
|
| 23. |
Ho SA, Aw DC. Extramammary Paget's disease treated with topical imiquimod 5% cream. Dermatol Ther 2010;23:423-7.
[Google Scholar]
|
| 24. |
Fien SM, Oseroff AR. Photodynamic therapy for non-melanoma skin cancer. J Natl Compr Canc Netw 2007;5:531-40.
[Google Scholar]
|
| 25. |
Housel JP, Lzikson L, Zeitouni NC. Noninvasive Extramammary Paget's disease treated with photodynamic therapy: Case Series from the Roswell Park Cancer Institute. Dermatol Surg 2010;36:1718-24.
[Google Scholar]
|
| 26. |
Sendagorta E, Herranz P, Feito M, Ramírez P, Floristán U, Feltes R, et al. Successful treatment of three cases of primary extramammary Paget's disease of the vulva with Imiquimod: Proposal of a therapeutic schedule. J Eur Acad Dermatol Venereol 2010;24:490-2.
[Google Scholar]
|
| 27. |
Li L, Deng Y, Zhang L, Liao W, Luo R, Huang Z. Treatment of perianal Paget's disease using photodynamic therapy with assistance of fluorescence examination: Case report. Lasers Med Sci 2009;24:981-4.
[Google Scholar]
|
| 28. |
Panasiti V, Bottoni U, Devirgiliis V, Mancini M, Rossi M, Curzio M, et al. Intralesional interferon alfa- 2b as neoadjuvant treatment for perianal extramammary Paget's disease. J Eur Acad Dermatol Venereol 2008;22:522-3.
[Google Scholar]
|
| 29. |
Ito Y, Igawa S, Ohishi Y, Uehara J, Yamamoto AI, Iizuka H. Prognostic indicators in 35 patients with extramammary Paget's disease. Dermatol Surg 2012;38:1938-44.
[Google Scholar]
|
Fulltext Views
4,381
PDF downloads
2,629





