Translate this page into:
Extranodal natural killer T-cell lymphoma mimicking cellulitis and venous thrombosis: A case report
2 Department of Dermatology, Second Xiangya Hospital, Central South University, Changsha, China
Correspondence Address:
Rong Xiao
Department of Dermatology, Second Xiangya Hospital, Central South University, 139 Ren-Min Road, Changsha 410011
China
| How to cite this article: Liu R, Chen J, Zhang G, Xiao R. Extranodal natural killer T-cell lymphoma mimicking cellulitis and venous thrombosis: A case report. Indian J Dermatol Venereol Leprol 2017;83:689-692 |
Sir,
A 50-year-old previously healthy Chinese male presented to our hospital with a 2-month history of left leg pain and a 20-day history of erythema, swelling, and erosion over the left medial malleolus. The pain was exacerbated on walking long distances. During an initial evaluation at another hospital, the patient was diagnosed with cellulitis and venous thrombosis over the left lower extremity. Antibiotics and anticoagulants, platelet aggregation inhibitors, and intravenous antibiotics were administered for two weeks without improvement. During an initial evaluation at another hospital, the patient was diagnosed with cellulitis and venous thrombosis, and treated with anticoagulants, platelet aggregation inhibitors, and intravenous antibiotics for two weeks. Hence, the patient was moved to the dermatology ward. The patient was referred to a surgeon as he showed no response to conventional treatment of cellulitis. The patient was moderately built and nourished without any comorbidities and in no acute stress, he denied mosquito bites, nose or throat illness, or weight loss since the onset of the lesion. Dermal inspection revealed a 5-cm diameter reddish infiltrative plaque with a 3-cm diameter superficial ulcer covered with crust and exudates [Figure - 1]. Several bean-sized (1.5 × 1.5 cm) lymph nodes were palpated in the bilateral inguinal region. Routine laboratory studies indicated the following: white blood cell (WBC) 4.0 × 109/L; neutrophil count (NC) 2.8 × 109/L; NC 70.9%; no atypical lymphocytes in peripheral blood smears, the d-dimer level was elevated to 0.6 ug/ml (normal 0.1–0.5 ug/ml), and EBV serology was positive for IgM and negative for IgG antibodies. Urinalysis, renal function tests, and serum immunoglobulin analysis were within the normal range; serology for human immunodeficiency virus, Treponema pallidum, and hepatitis B and C were negative. A lesion biopsy revealed a subepidermal blister, a diffuse dense infiltrate of atypical mononuclear cells involving the dermis and subcutis with angiocentric and angiodestructive features [Figure 2a] and [Figure 2b]. Thrombosis and fibrinoid vessel necrosis were also present [Figure 2c]. Sweat glands and nerves were invaded [Figure 2d]. Immunochemistry identified infiltrated atypical cells as positive for CD56/Ki-67 (80%) [Figure 3a] and [Figure 3b], and focally positive for CD30 [Figure 3c]. In-situ hybridization staining for Epstein–Barr virus (EBV)-encoded small nonpolyadenylated RNA-1 was positive [Figure 3d], and a bone marrow biopsy was normal as was a chest X-ray.
 |
| Figure 1: Single raised ulcerated reddish plaque with central crusts on the left medial malleolus |
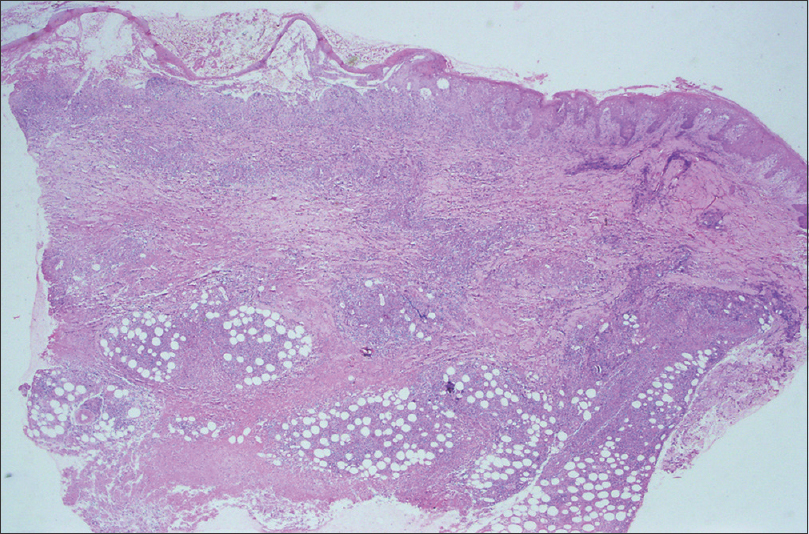 |
| Figure 2a: Intraepidermal and subepidermal blister, dermal papilla edema, a dense dermal, and subcutaneous lymphoid infiltrate (H and E, ×20) |
 |
| Figure 2b: Diffuse atypical lymphocytic infiltration involving the dermis and subcutaneous fat (H and E, ×400) |
 |
| Figure 2c: Diffuse atypical lymphocytic infiltration involving the vaculature (H and E, ×200) |
 |
| Figure 2d: Diffuse atypical lymphocytic infiltration involving the nerve (H and E, ×400) |
 |
| Figure 3a: Immunohistochemistry of skin biopsy: Tumor cells positive for CD56 (diaminobenzidine chromogen, ×400) |
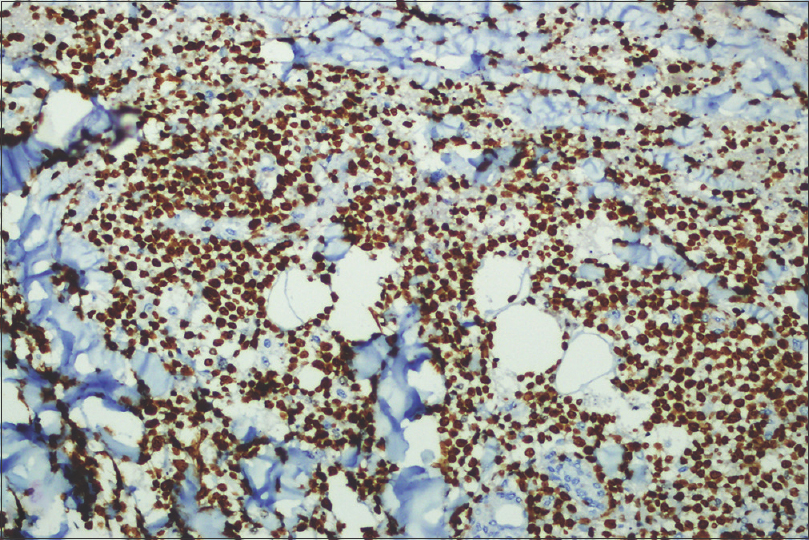 |
| Figure 3b: Immunohistochemistry of skin biopsy: Tumor cells positive for Ki-67 (diaminobenzidine chromogen, ×200) |
 |
| Figure 3c: Immunohistochemistry of skin biopsy: Tumor cells positive for CD30 (diaminobenzidine chromogen, ×200) |
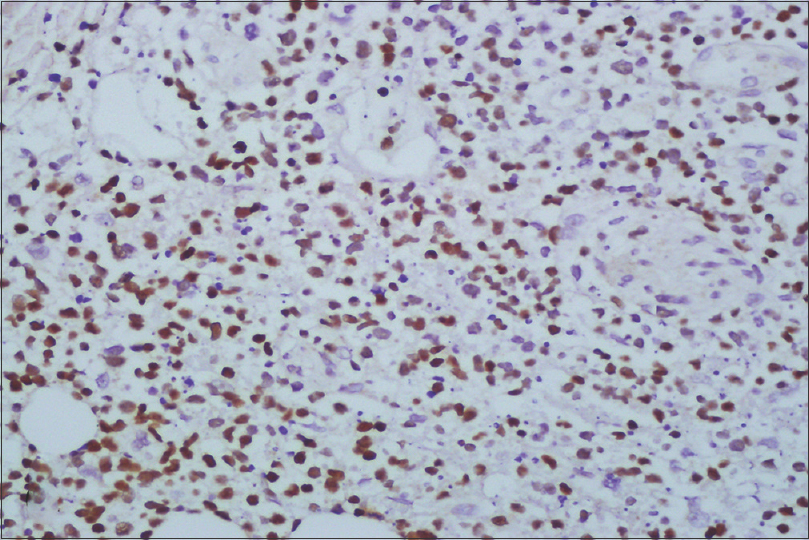 |
| Figure 3d: Immunohistochemistry of skin biopsy: Tumor cells positive for Epstein-Barr virus encoded RNAs (diaminobenzidine chromogen, ×200) |
Color Doppler ultrasound revealed arteriosclerosis of the bilateral lower limbs and multiple plaques. Slow blood flow of the left popliteal and femoral superficial vein, which did not exclude the mural thrombus. Multiple enlarged lymph nodes appeared bilaterally in the groins, the root of the thigh, and the left popliteal fossa. Positron emission tomography (PET)-CT scans indicated markedly hypermetabolic soft tissue masses involving the posterior aspect of the left ankle and femur. Increased fluorodeoxyglucose uptake corresponded to infiltrative lesions in the subcutaneous adipose tissue of the left leg and foot. Bilateral shank muscle heterogeneity, increased glucose metabolism, and enlarged lymph nodes with fluorodeoxyglucose activity in the bilateral popliteal and inguinal areas were also evident. Bilateral pleural and pericardial effusion and reactive hyperplasia lymph nodes were present in the mediastina. Thus, a cutaneous IV, BE stage lymphoma of the left lower extremity was diagnosed involving the bilateral shank muscle.
After diagnosis, the patient received multidrug combination chemotherapy including gemcitabine, oxaliplatin, and dexamethasone for 7 cycles. L-asparaginase was added during the last 3 cycles. Primary lesions initially remitted during therapy, however, the patient later returned with an intermittent high fever and two new ulcerative lesions, one on the left lower leg and another at the inguinal lymph node (2.0-cm diameter). The patient was pancytopenic with liver failure, and finally developed disseminated intravascular coagulation. Treatment was stopped after 7 cycles of chemotherapy and the patient died 9 months later.
According to the new classification of cutaneous T- and B-cell lymphomas of EORTC and WHO, extranodal NK/T-cell lymphoma, nasal-type is described as a subtype of Epstein-Barr virus-associated NK/T-cell lymphoma that is aggressive and associated with poor prognosis.[1] Cellulitis accompanied with venous thrombosis was the initial diagnosis, which is a rare presentation for extranodal NK/T-cell lymphoma, nasal-type, as evidenced by the literature confirming that extranodal NK/T-cell lymphoma, nasal-type cases are often misdiagnosed as cellulitis.[2],[3],[4] Although the major causes of venous thrombosis include malignancy, and recent major surgery, etc., we were unable to find any previous reports extranodal NK/T-cell lymphoma, nasal-type cases that have been misdiagnosed as venous thrombosis.[5]
In summary, cutaneous extranodal NK/T-cell lymphoma, nasal-type has varied manifestations, leading to the initial confusion and misdiagnosis as cellulitis and venous thrombosis with color Doppler ultrasound. Angioinvasion of the dermis and subcutis is common but not specific to extranodal NK/T-cell lymphoma, nasal-type, which can lead to extensive tissue necrosis and vessel thrombosis. As a neoplastic cell in entity, it often fails to respond to multiple-agent chemotherapy, and is associated with poor prognosis. This case emphasizes that relying solely on clinical features can cause extranodal NK/T-cell lymphoma, nasal-type misdiagnosis as an infectious disease and angiopathy. Skin biopsy is vital for excluding lymphomas, panniculitis, and cutaneous vasculitis in cases not responding to conventional treatment of cellulitis.
Acknowledgement
We thank Jing W. Zhang, MD, PhD, for excellent, helpful comments (Diplomate, American Board of Pathology Anatomic Pathology and Clinical Pathology Columbia, SC 29204, USA). Written informed consent was obtained from the patient for the publication of this report and any accompanying images.
Financial support and sponsorship
This work was supported by the National Natural Science Foundation of China (No. 81371744).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 2. |
Choi YL, Park JH, Namkung JH, Lee JH, Yang JM, Lee ES, et al. Extranodal NK/T-cell lymphoma with cutaneous involvement: 'Nasal' vs. 'nasal-type' subgroups – A retrospective study of 18 patients. Br J Dermatol 2009;160:333-7.
[Google Scholar]
|
| 3. |
Jia H, Sun T. Extranodal NK/T-cell lymphoma mimicking cellulitis. Leuk Lymphoma 2004;45:1467-70.
[Google Scholar]
|
| 4. |
Kim JW, An JH. Extranodal natural killer/T-cell lymphoma, nasal type, of the orbit mimicking recurrent orbital cellulitis. J Craniofac Surg 2014;25:509-11.
[Google Scholar]
|
| 5. |
Goldhaber SZ. Risk factors for venous thromboembolism. J Am Coll Cardiol 2010;56:1-7.
[Google Scholar]
|
Fulltext Views
2,622
PDF downloads
1,089





