Translate this page into:
Extranodal natural killer/T cell lymphoma, nasal type presenting as recurrent facial cellulitis
2 Department of Pathology, Singapore General Hospital, Singapore
Correspondence Address:
Colin WX Tan
Department of Dermatology, Singapore General Hospital, Outram Road
Singapore
| How to cite this article: Tan CW, Tan HY, Chin Hong RG, Pang SM. Extranodal natural killer/T cell lymphoma, nasal type presenting as recurrent facial cellulitis. Indian J Dermatol Venereol Leprol 2017;83:687-689 |
Sir,
A 69-year-old Chinese male presented to our department with persistent progressive facial swelling of 9 months' duration. Over this period, the patient had been under the care of various disciplines including otorhinolaryngology, internal medicine, and dental service. He was diagnosed with and managed for chronic rhinosinusitis and recurrent facial cellulitis, however, his symptoms continued to worsen and progress.
Upon presentation to our department, the swelling and pain had progressed to involve the right face and the patient was febrile. On physical examination, there was midfacial erythema and edema involving the periorbital and maxillary regions, with necrotic eschar located over the left infraorbital region and left supraorbital ridge [Figure - 1].
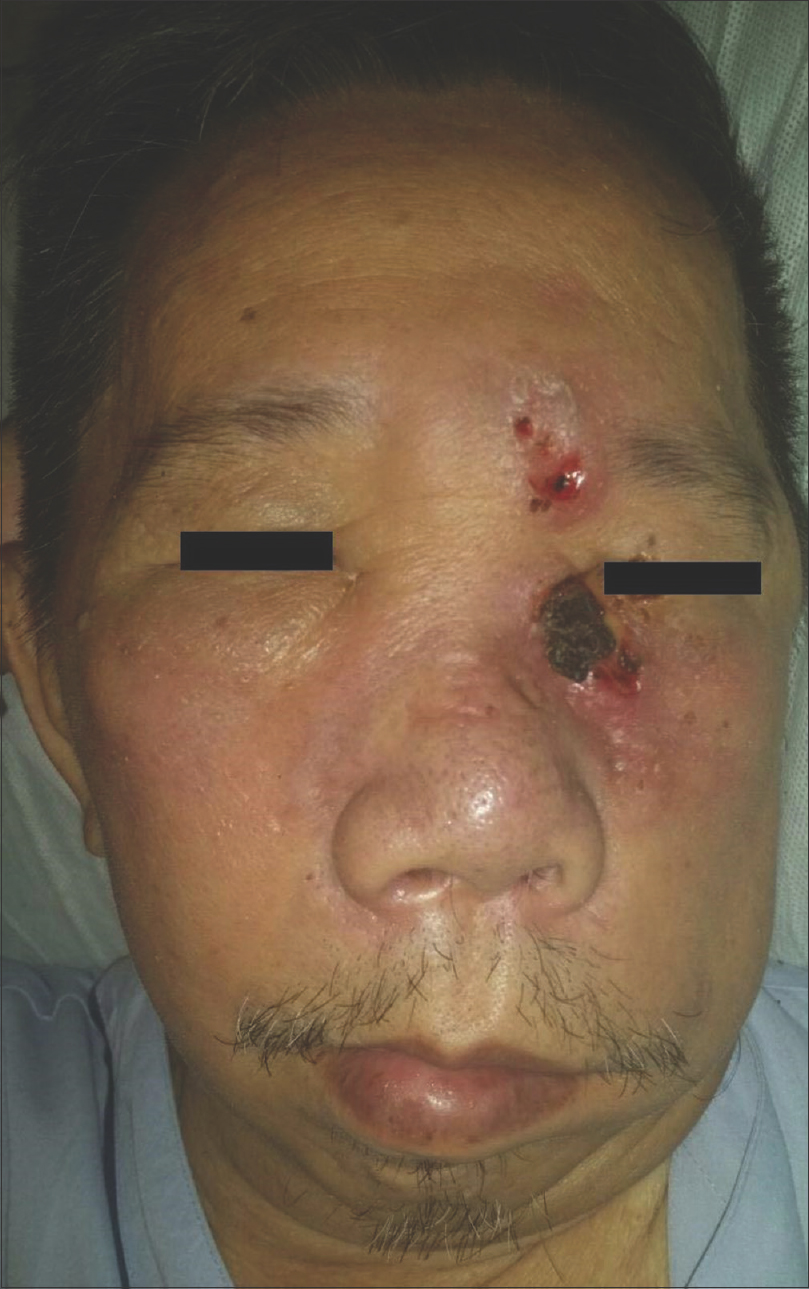 |
| Figure 1: Midfacial swelling and erythema |
Computed tomography (CT) scan of the face was performed which showed diffuse subcutaneous soft tissue thickening and fat stranding. The initial differential diagnoses included a deep fungal infection or mycobacterial infection. Given the history of prior irradiation to the head and neck region, cutaneous malignancy was also considered, and hence, a biopsy was performed.
Histological examination showed a diffuse infiltrate of atypical small to medium-sized lymphocytes in the dermis with marked pseudoepitheliomatous hyperplasia and focal ulceration [Figure - 2] and [Figure - 3]. There was a strong reactivity for Epstein-Barr virus (EBV)-encoded RNA [Figure - 4]. Immunohistochemical analysis showed weak positivity for cytoplasm CD3 and weak but extensive positivity for CD56 [Figure - 5]. Cytotoxic granule proteins granzyme-B and T-cell-restricted intracellular antigen-1 were strongly positive, and the atypical lymphocyte populations were double negative for T-cell coreceptors CD4 and CD8. Based on these findings, extranodal NK/T cell lymphoma, nasal type, was diagnosed.
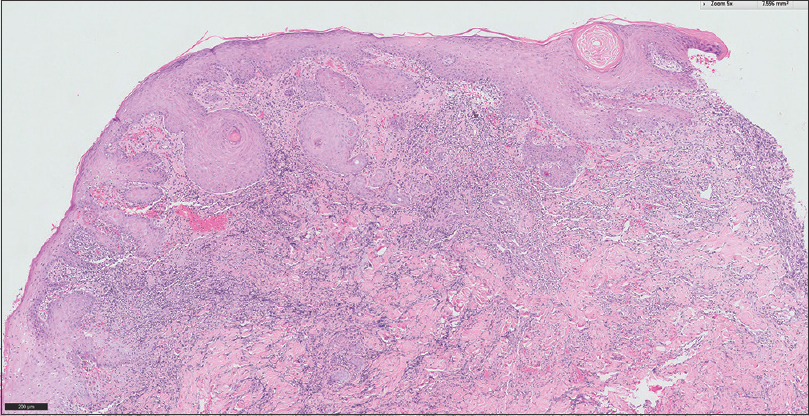 |
| Figure 2: Hematoxylin and eosin stain demonstrating pseudoepitheliomatous hyperplasia and a dense perivascular infiltrate of atypical small-to-medium sized lymphocytes (×40) |
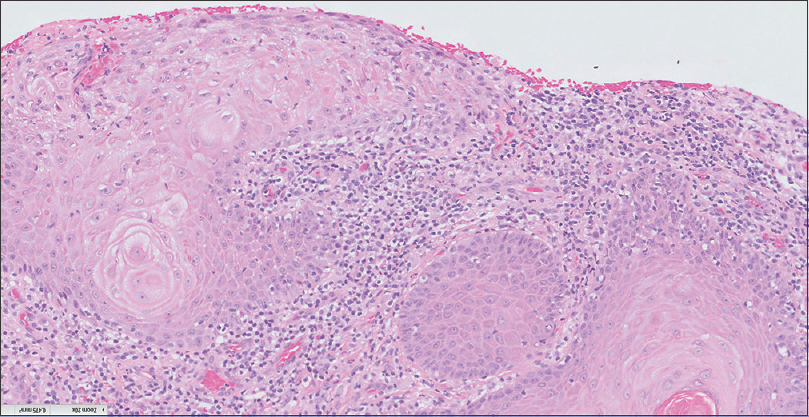 |
| Figure 3: Hematoxylin and eosin stain demonstrating pseudoepitheliomatous hyperplasia and a dense perivascular infiltrate of atypical small-to-medium sized lymphocytes (×100) |
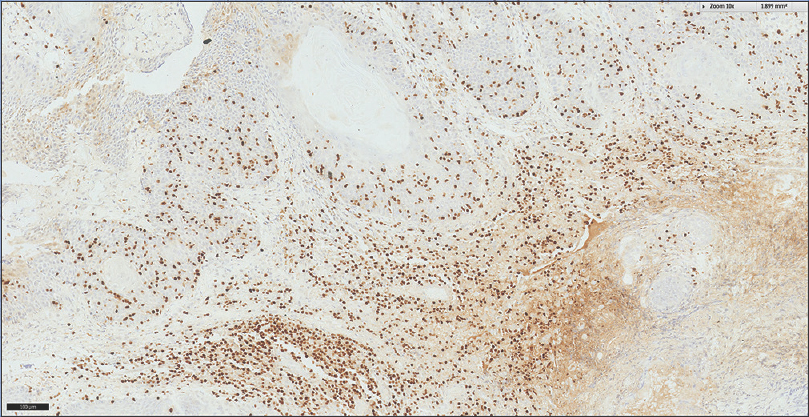 |
| Figure 4: Immunohistochemical stain demonstrating a strong reactivity for EBV-encoded RNA in-situ hybridization (×100) |
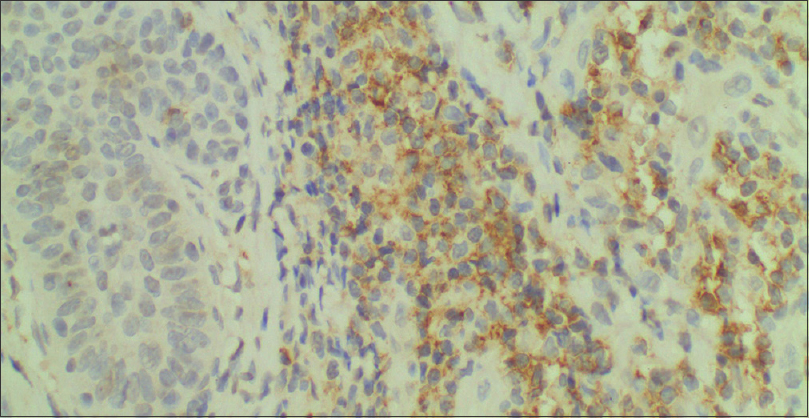 |
| Figure 5: Immunohistochemical stain demonstrating positivity for cytoplasmic CD56 (×200) |
The patient was referred to the oncology service for further management and underwent positron-emission tomography (PET)–CT scan, which demonstrated disease localized to the nasal cavity and facial skin. A bone marrow aspirate showed no bone marrow involvement. GELOX chemotherapy regimen (Gemcitabine, L-Asparaginase, Oxaliplatin) was started followed by radiotherapy, with subsequent improvement of the facial swelling.
Extranodal NK/T cell lymphoma, nasal type, is an uncommon non-Hodgkin lymphoma of NK cell and NK-like T-cell origin. It is more frequently encountered in the Asian and Latin American populations ranging 6–10% of non-Hodgkin lymphomas in these geographic distributions [1],[2] compared to <1% of non-Hodgkin lymphomas in the Caucasian population.[3] Males in their 5th decade are more frequently affected, with gender ratios varying from 1.5:1 to 3:1.[1],[2],[3]
The nasal type of extranodal NK/T cell lymphoma predominates and classically presents as a destructive midline facial lesion originating from the nasal region. It commonly presents with symptoms of nasal obstruction and discomfort, facial swelling, and epistaxis.[1],[2],[3],[4],[5] Differentials at first presentation depend on the degree of invasion/destruction and symptoms manifested, which can be infections, granulomatous disease, and cutaneous malignancy.
Histologically, extranodal NK/T cell lymphoma is characterized by tumor cells of varying sizes with angiocentricity and angiodestruction along with significant necrosis and ulceration.[1],[2] There is often an associated prominent polymorphous inflammatory infiltrate including neutrophils, lymphocytes, eosinophils, and histiocytes. Immunohistochemical staining is required for the diagnosis which shows a characteristic positivity for cytoplasm restricted CD3 or CD3ε and CD56, one or more cytotoxic granule proteins such as granzyme-B, T-cell-restricted intracellular antigen-1, or perforin, and are strongly positive for Epstein-Barr virus-encoded RNA.[1],[2] Surface CD3 and T-cell markers CD4 and CD8 are usually negative.
Diagnosis is often challenging and nasal type extranodal NK/T cell lymphoma may first present to the otorhinolaryngologist. A high index of suspicion is needed to initiate further evaluation, which may only be carried out after repeated courses of antibiotics.[4] Biopsy of suspicious cases can be challenging for the histopathologist because of the mixed inflammatory infiltrate and predisposition for secondary infection, which may obscure the lymphomatous cell population [1]. The time between onset of symptoms and a confirmed histological diagnosis can range between 2 months and 1 year.[1],[2]
Various chemotherapy regimens have been described in treating extranodal NK/T cell lymphoma, usually with L-asparaginase containing regimens which are chosen due to their relative efficacy. Radiotherapy may be used in combination with or after chemotherapy but has a high relapse rate if used alone.[1],[2],[5] Allogenic hematopoietic stem cell transplant has also been used with good results.[5]
This case highlights the need for a high index of clinical suspicion in cases of recurrent facial cellulitis. In the clinical context of recurrent facial cellulitis with symptoms of rhinosinusitis and the relevant patient demographic, extranodal NK/T cell lymphoma, nasal type is an important consideration. Early detection of the disease requires physician awareness to obtain a histological diagnosis so as not to delay treatment and worsen prognosis. We hope that this serves as a timely reminder to re-examine cases of facial cellulitis and sinusitis refractory to antibiotic therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ng SB, Lai KW, Murugaya S, Lee KM, Loong SL, Fook-Chong S, et al. Nasal-type extranodal natural killer/T-cell lymphomas: A clinicopathologic and genotypic study of 42 cases in Singapore. Mod Pathol 2004;17:1097-107.
[Google Scholar]
|
| 2. |
Khan L, Hodgson D, Sun A, Gospodarowicz M, Crump M, Kuruvilla J, et al. Asingle institution experience of extranodal natural killer/T cell lymphoma of nasal type. Leuk Lymphoma 2015;56:80-4.
[Google Scholar]
|
| 3. |
Ai WZ, Chang ET, Fish K, Fu K, Weisenburger DD, Keegan TH. Racial patterns of extranodal natural killer/T-cell lymphoma, nasal type, in California: A population-based study. Br J Haematol 2012;156:626-32.
[Google Scholar]
|
| 4. |
Miyake MM, Oliveira MV, Miyake MM, Garcia JO, Granato L. Clinical and otorhinolaryngological aspects of extranodal NK/T cell lymphoma, nasal type. Braz J Otorhinolaryngol 2014;80:325-9.
[Google Scholar]
|
| 5. |
Tababi S, Kharrat S, Sellami M, Mamy J, Zainine R, Beltaief N, et al. Extranodal NK/T-cell lymphoma, nasal type: Report of 15 cases. Eur Ann Otorhinolaryngol Head Neck Dis 2012;129:141-7.
[Google Scholar]
|
Fulltext Views
2,794
PDF downloads
1,320





