Translate this page into:
Extranodal NK/T-cell lymphoma manifesting as cutaneous lesions and intestinal perforation: A case report
Corresponding author: Prof. Xiaojing Kang, Department of Dermatology, People’s Hospital of Xinjiang Uygur Autonomous Region; Xinjiang Clinical Research Center for Dermatologic Diseases; Xinjiang Key Laboratory of Dermatology Research (XJYS1707), 91 Tian-chi Road, Urumqi-830001, XinJiang, China. drkangxj666@163.com
-
Received: ,
Accepted: ,
How to cite this article: Shi J, Jin L, Zhang, D, Kang X. Extranodal NK/T-cell lymphoma manifesting as cutaneous lesions and intestinal perforation: A case report. Indian J Dermatol Venereol Leprol 2023;89:927
Dear Editor,
We report a 70-year-old male patient with multifocal extranodal NK/T-cell lymphoma manifesting as cutaneous lesions and intestinal perforation. This patient presented with a 10-days history of bullae and nodules in the lumbar region, that was initially diagnosed to be varicella zoster infection. However, patient gave history of intermittent fever, and weight loss of about 10 kgs in the last 5 months.
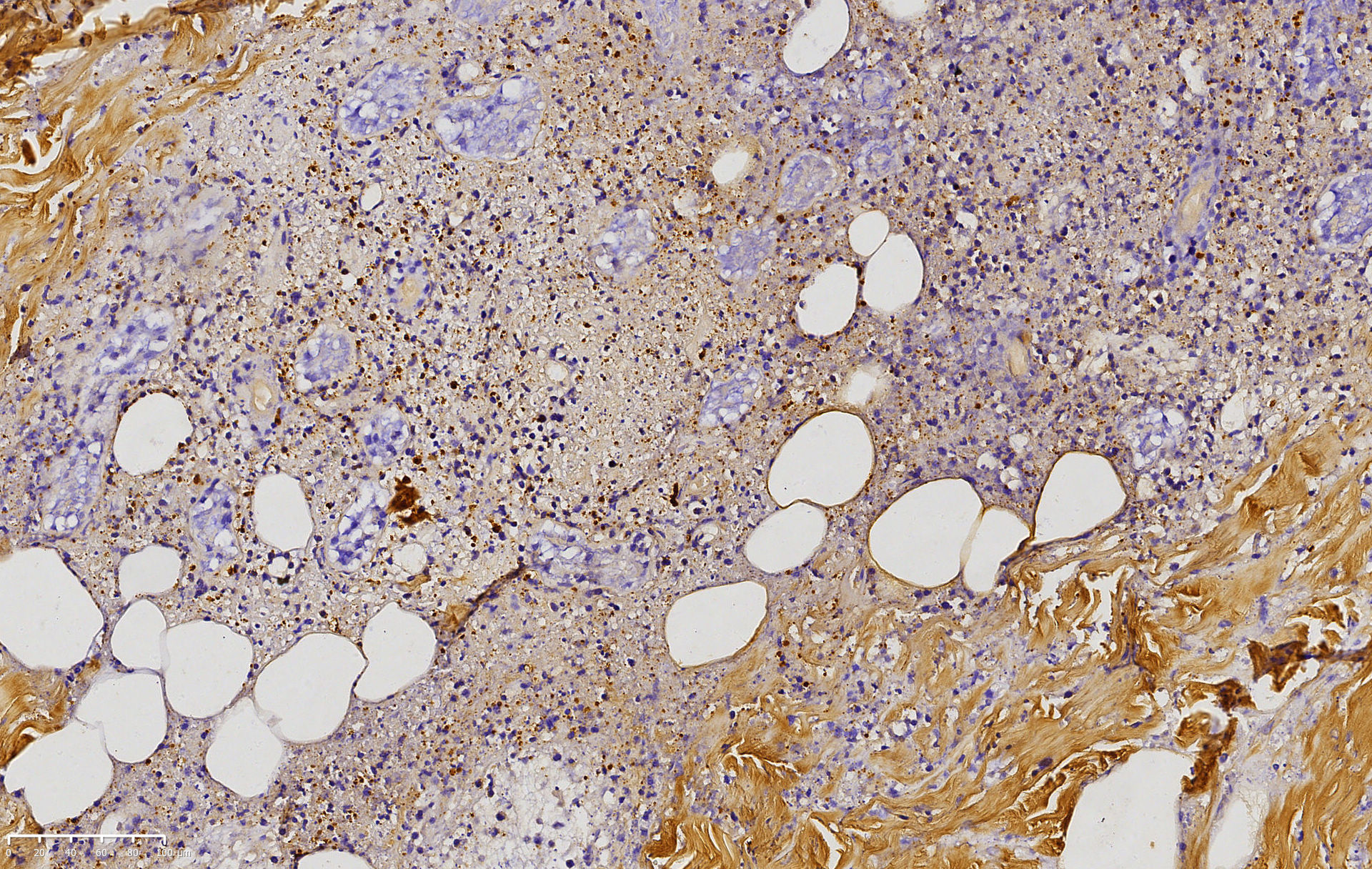
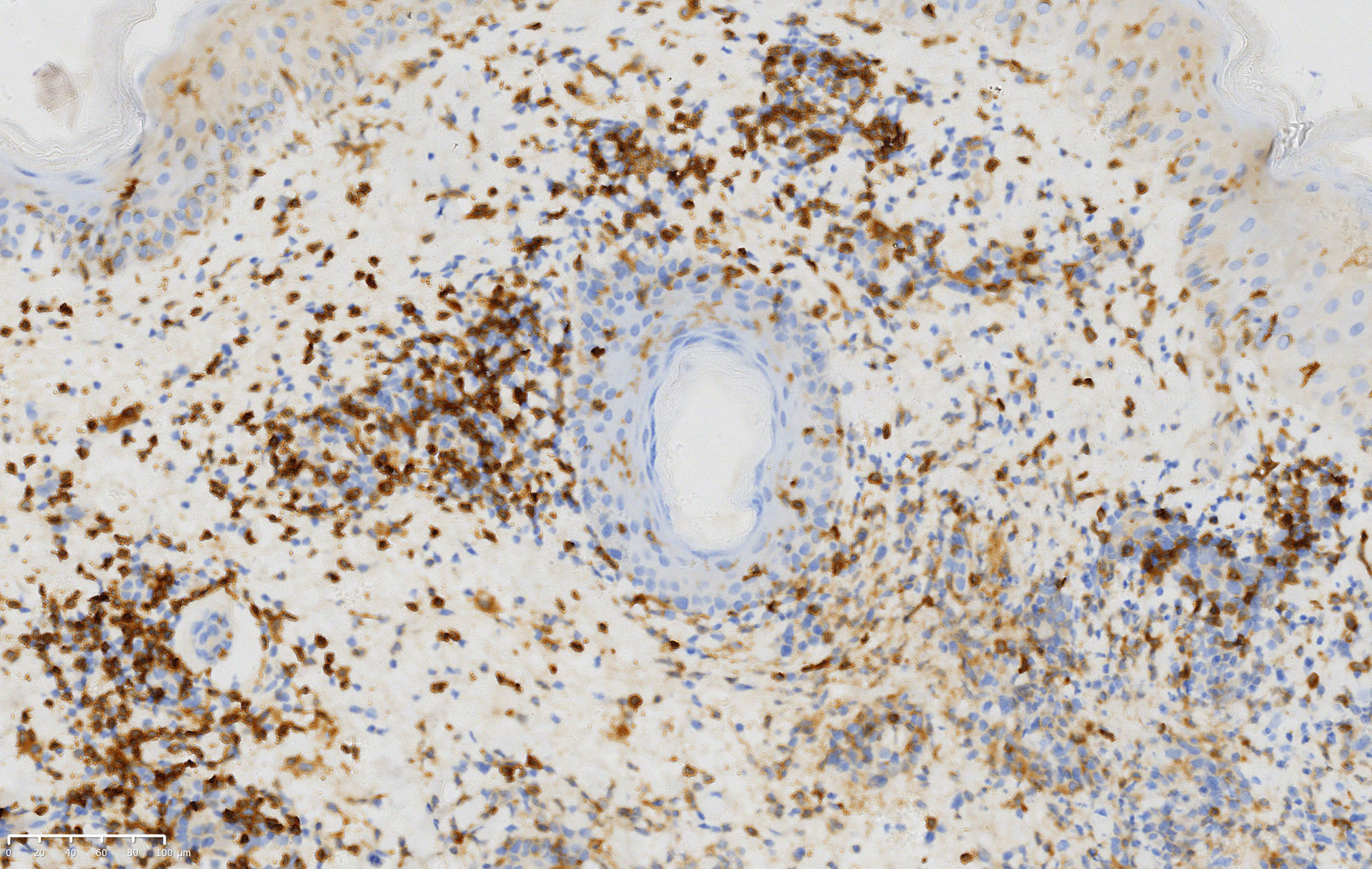
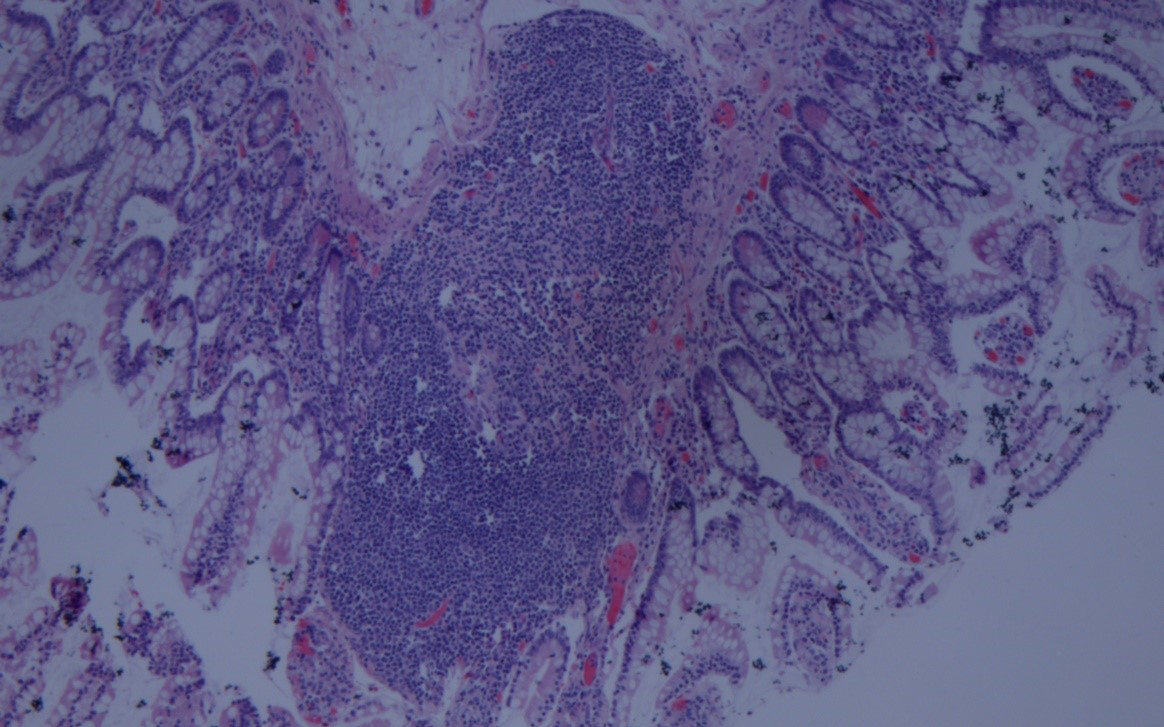
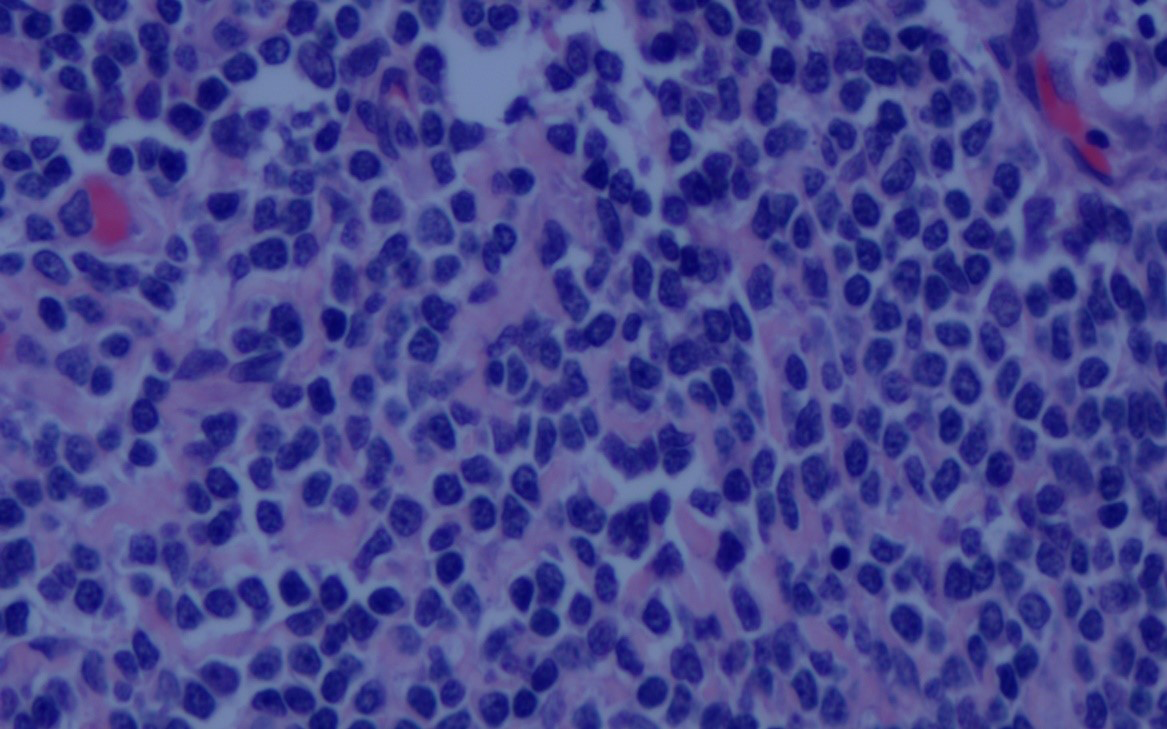
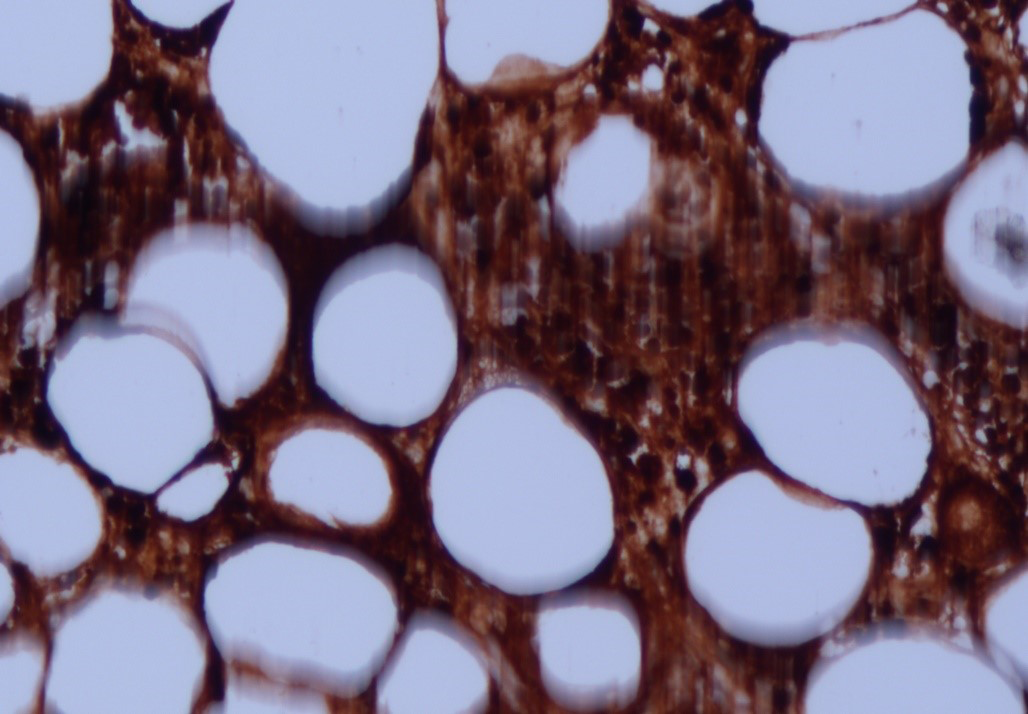
The skin lesions progressed to ulcers with necrotic crusting over his back, abdomen and left thigh, along with closely set pustules under his right breast [Figures 1a and 1b]. Routine laboratory examinations results have been tabulated [Table 1]. Abdominal computed tomography revealed that the wall of the local transverse colon was thickened, rough and significantly enhanced, with some gas shadows around this area and in the abdominal cavity A skin biopsy from the lesion under the right breast and abdomen revealed many necrotic keratinocytes with epidermal ulceration There was predominantly angiocentric and angiodestructive lymphocytic infiltration in the entire dermis and fat lobules [Figures 3a–3c]. Immunohistochemistry showed that the tumour cells were positive for CD3, CD4, CD8 and CD56 and negative for CD20 [Figures 4a–4h]. Immunohistochemical staining of the left abdominal skin lesion showed that the neoplastic cells were positive for CD30, Epstein-Barr virus-encoded small RNAs and Ki-67 additionally.

- An isolated nodular erythema was observed on the left lower abdomen with black scabs on the surface

- During hospitalisation, there was nodular erythema under the right breast with densely distributed pustules on the surface
| Index | Actual value | Normal value |
|---|---|---|
| lymphocyte count | 0.6 × 109/L | 1.1–3.2 × 109/L |
| lymphocyte percentage | 14.4% | 20–50% |
| neutrophil percentage | 75.8% | 40–75% |
| albumin | 33.4 g/L | 40–55 g/L |
| aspartate aminotransferase | 50.0 U/L | 13–40 U/L |
| lactate dehydrogenase | 370.1 U/L | 120–250 U/L |
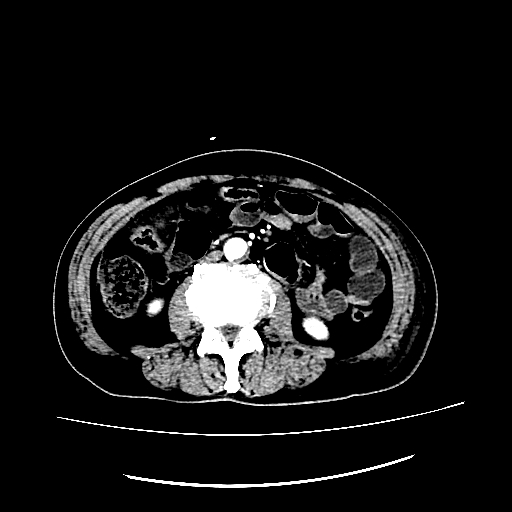
- The local transverse colon was thickened, rough, and significantly enhanced. There were some gas shadows in the abdominal cavity
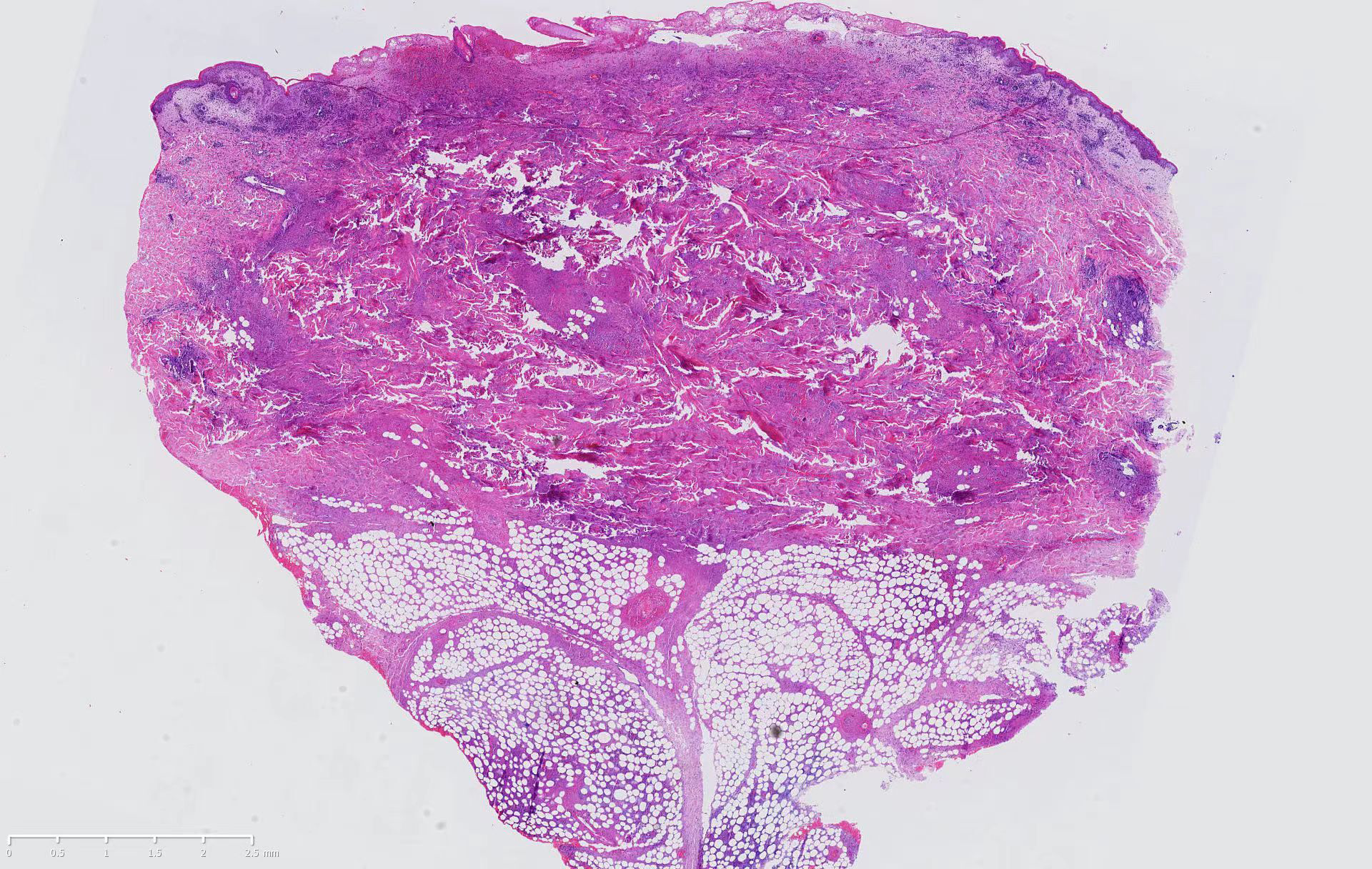
- Histopathology of the left lower abdominal lesion (H and E, ×10) Epidermal necrosis and ulcer formation, epidermal cell edema, a large number of lymphoid cells infiltrating around blood vessels in the superficial dermis, necrosis of collagen fibers in the dermis, and mixed infiltration of lymphoid cells and inflammatory cells into fat lobules.
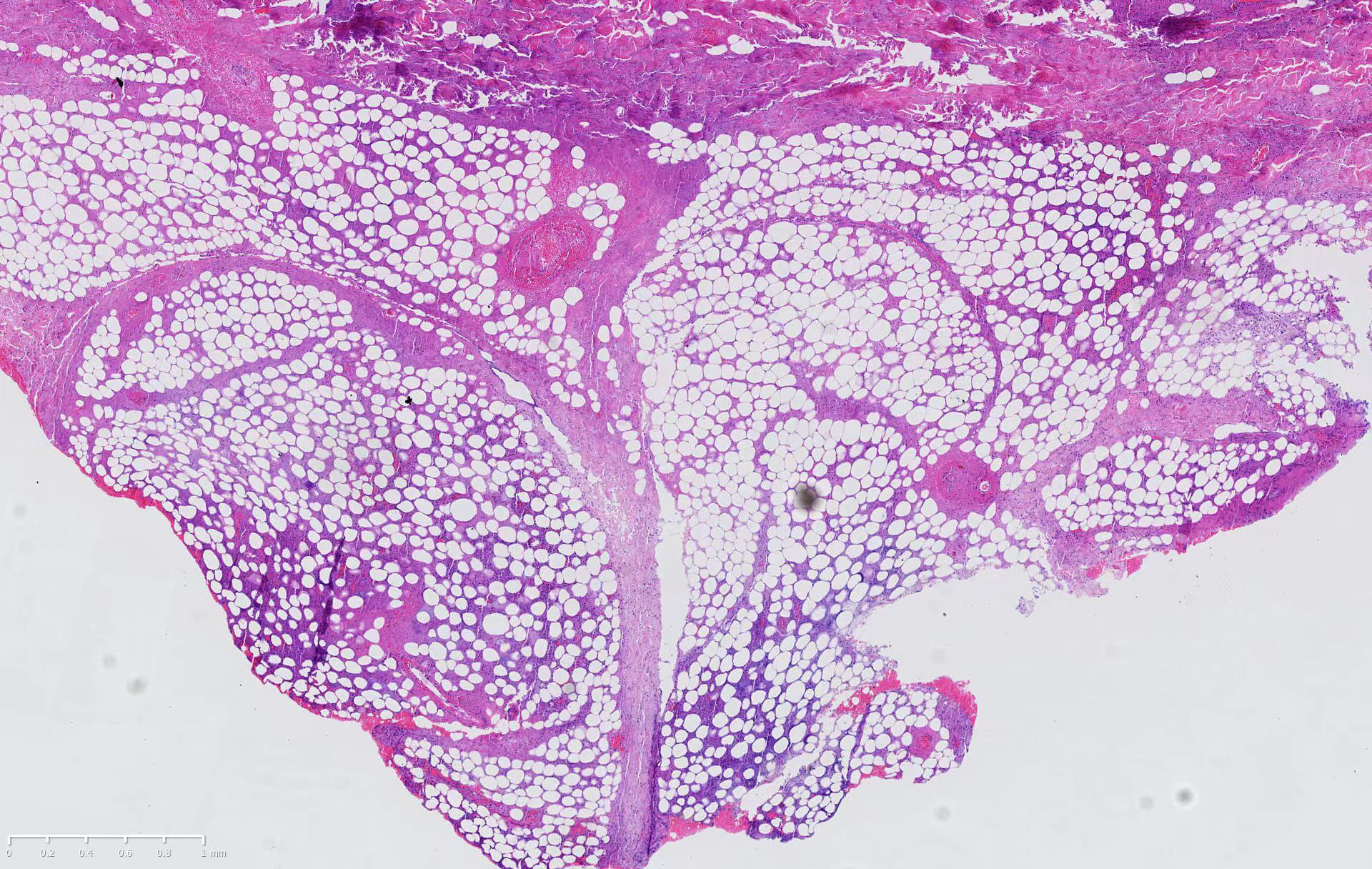
- Biopsy of the left lower abdominal lesion, showing atypical lymphoid cells infiltration of fat lobules mixed with inflammatory cells (H and E, ×20)
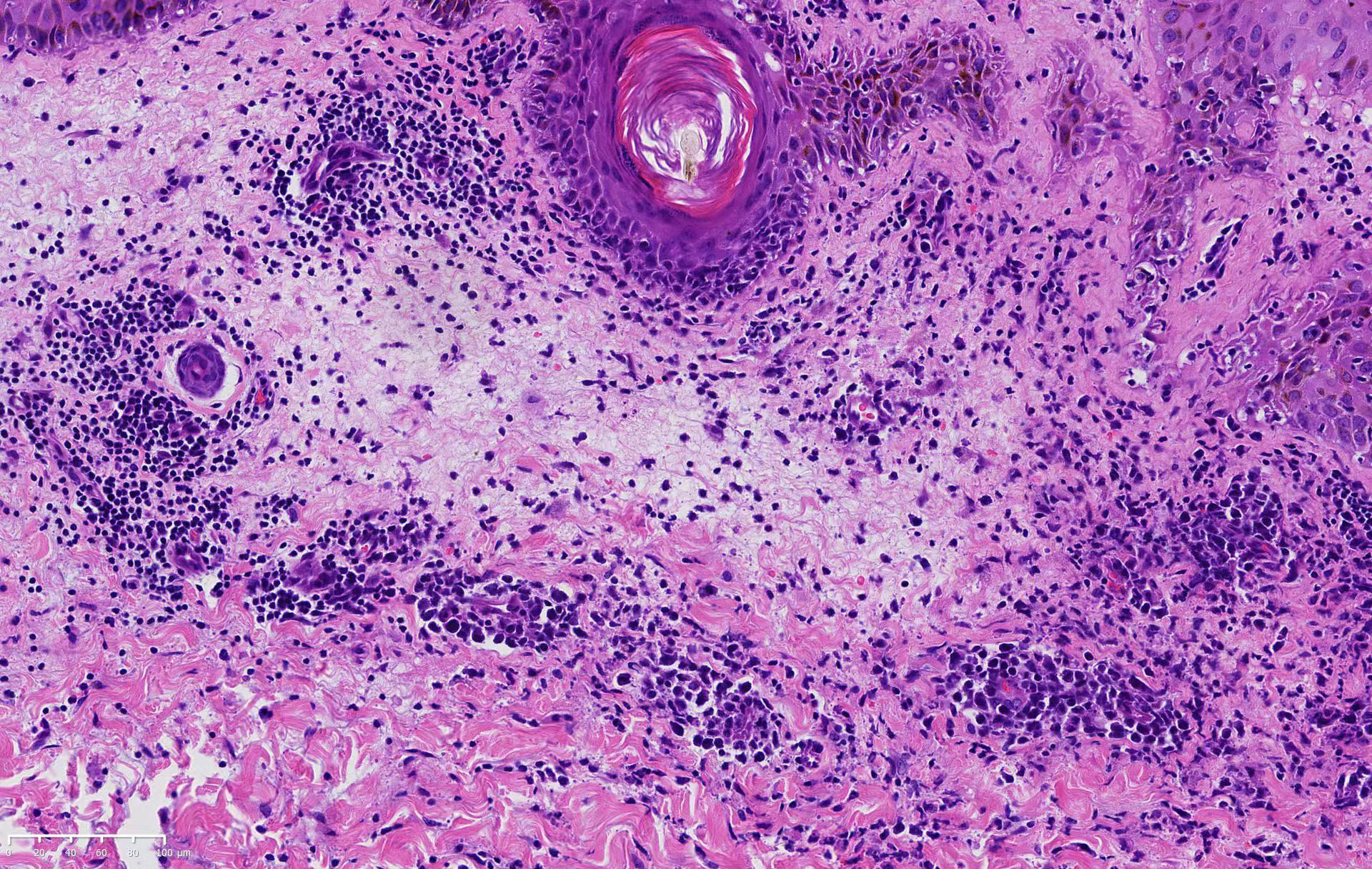
- Biopsy of the left lower abdominal lesion, showing atypical lymphoid cells distributed throughout the dermis infiltrated the vascular wall or around the blood vessels (H and E, ×200)
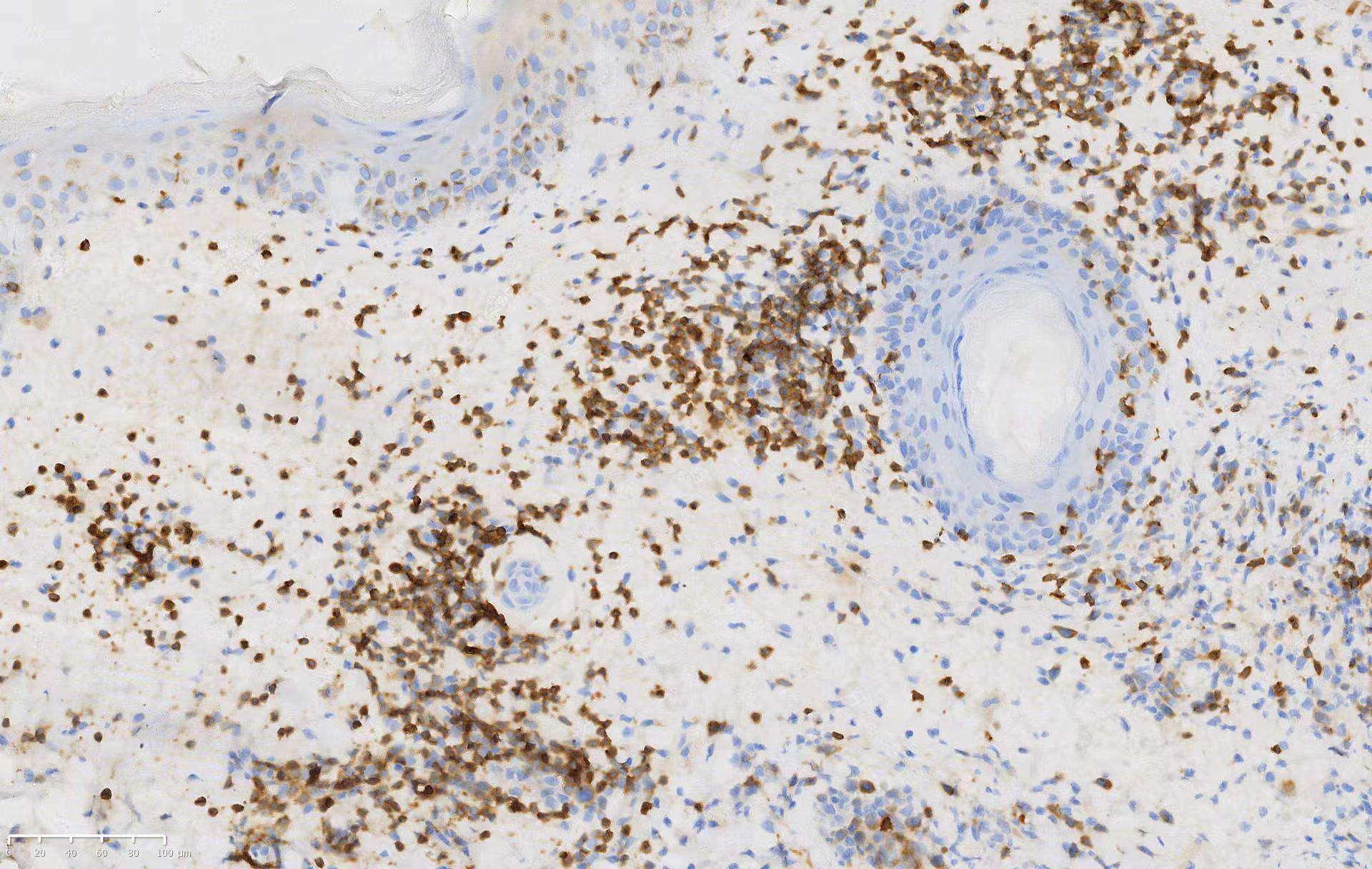
- Atypical lymphoid cells positive for clusters of differentiation 3 in the biopsy (clusters of differentiation 3, ×200)
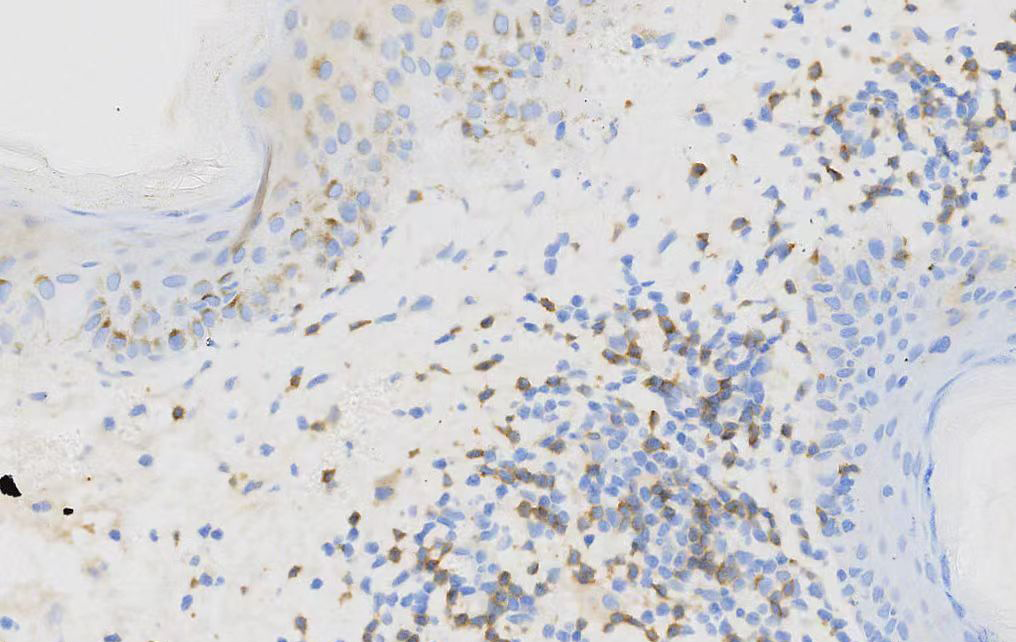
- Atypical lymphoid cells partially positive for clusters of differentiation 8 in the biopsy (clusters of differentiation 8, ×200)
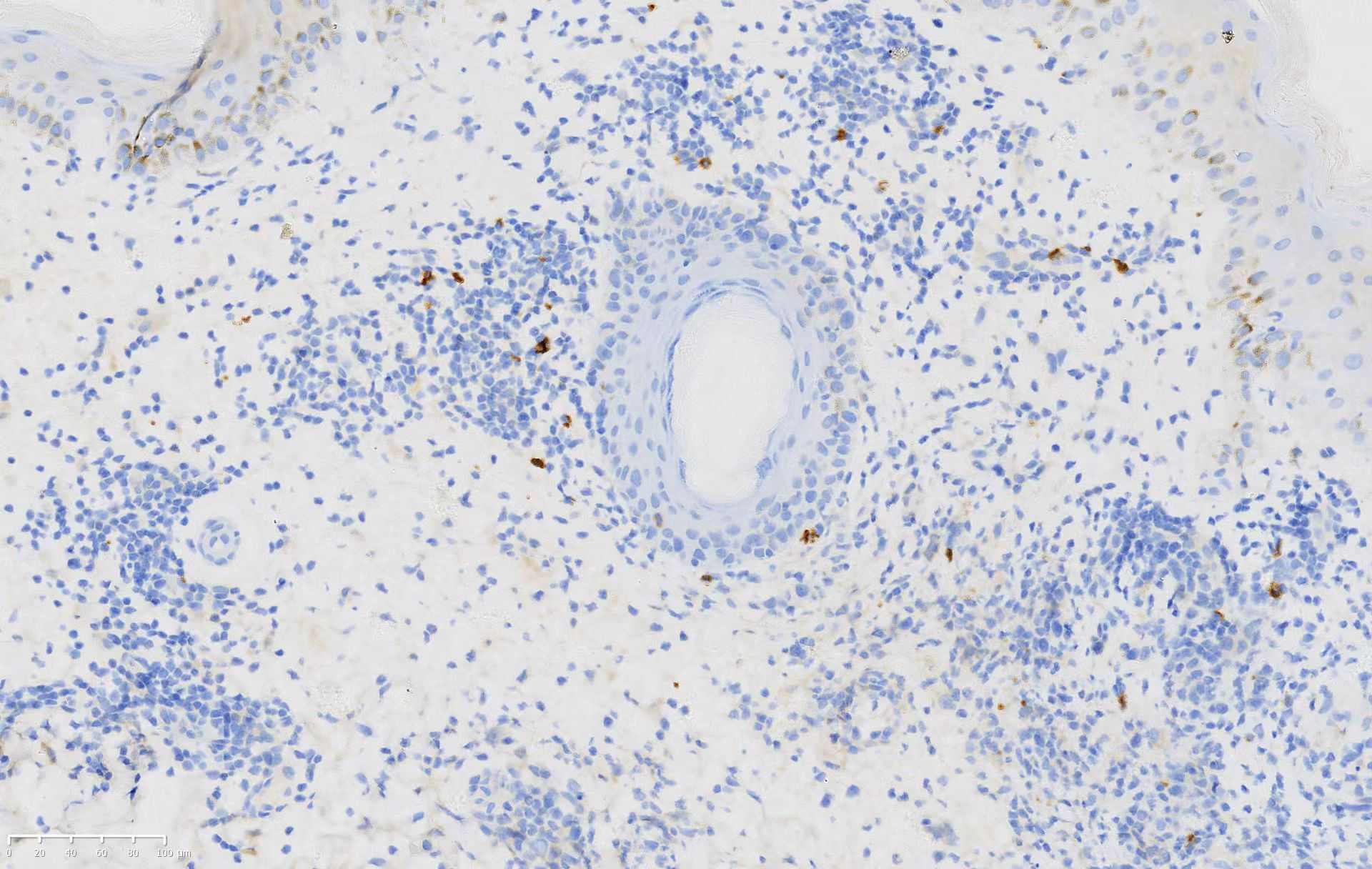
- Atypical lymphoid cells negative for clusters of differentiation 20 in the biopsy (clusters of differentiation 20, ×200)
- Atypical lymphoid cells positive for clusters of differentiation 56 in the biopsy (clusters of differentiation 56, ×200)
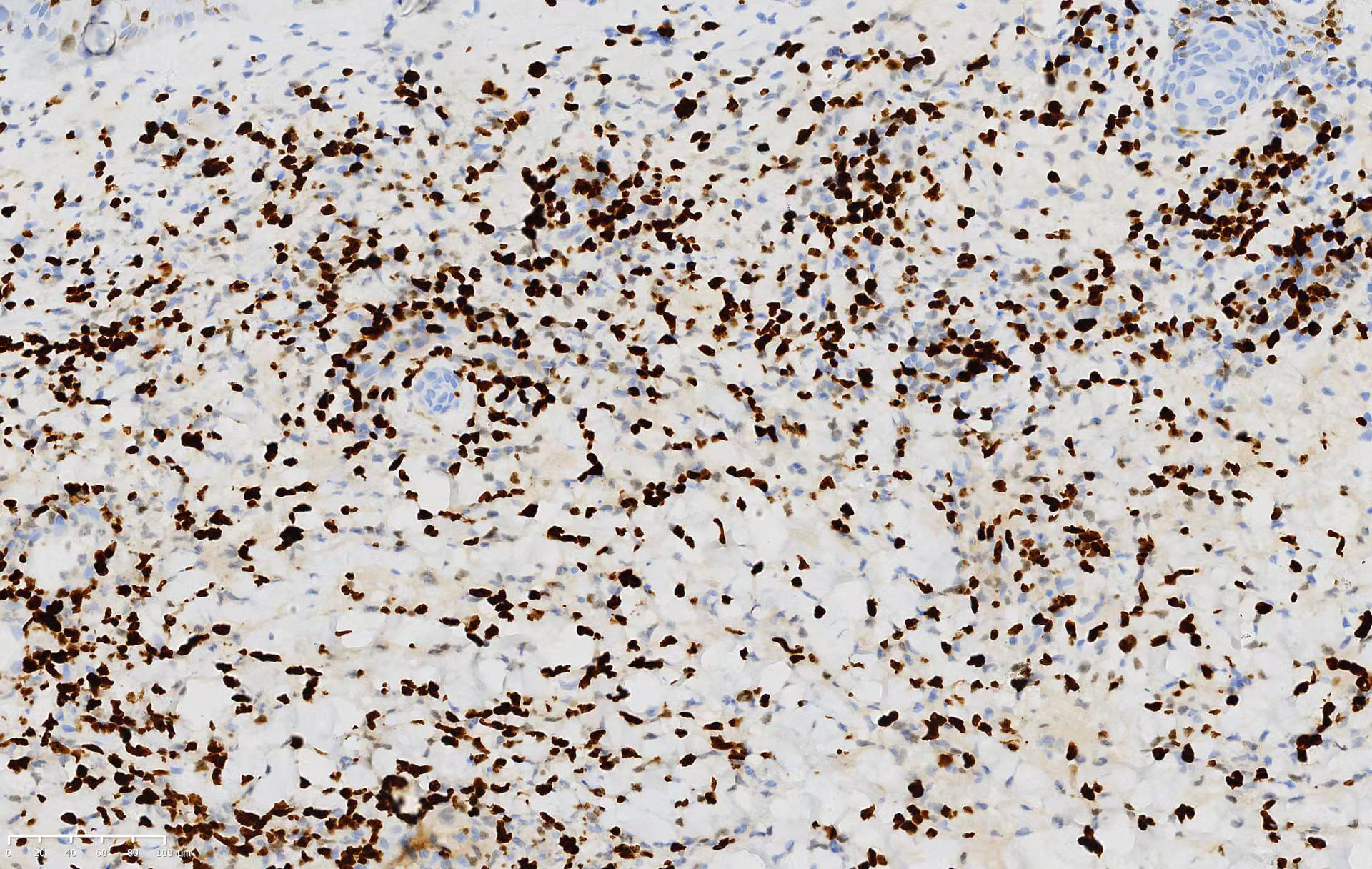
- Atypical lymphoid cells partial positive for Ki-67 in the biopsy (Ki-67, ×200)
- Atypical lymphoid cells positive for Epstein–Barr encoding region in the biopsy (Epstein–Barr encoding region, ×200)
- Atypical lymphoid cells positive for clusters of differentiation 4 in the biopsy (clusters of differentiation 4, ×200)
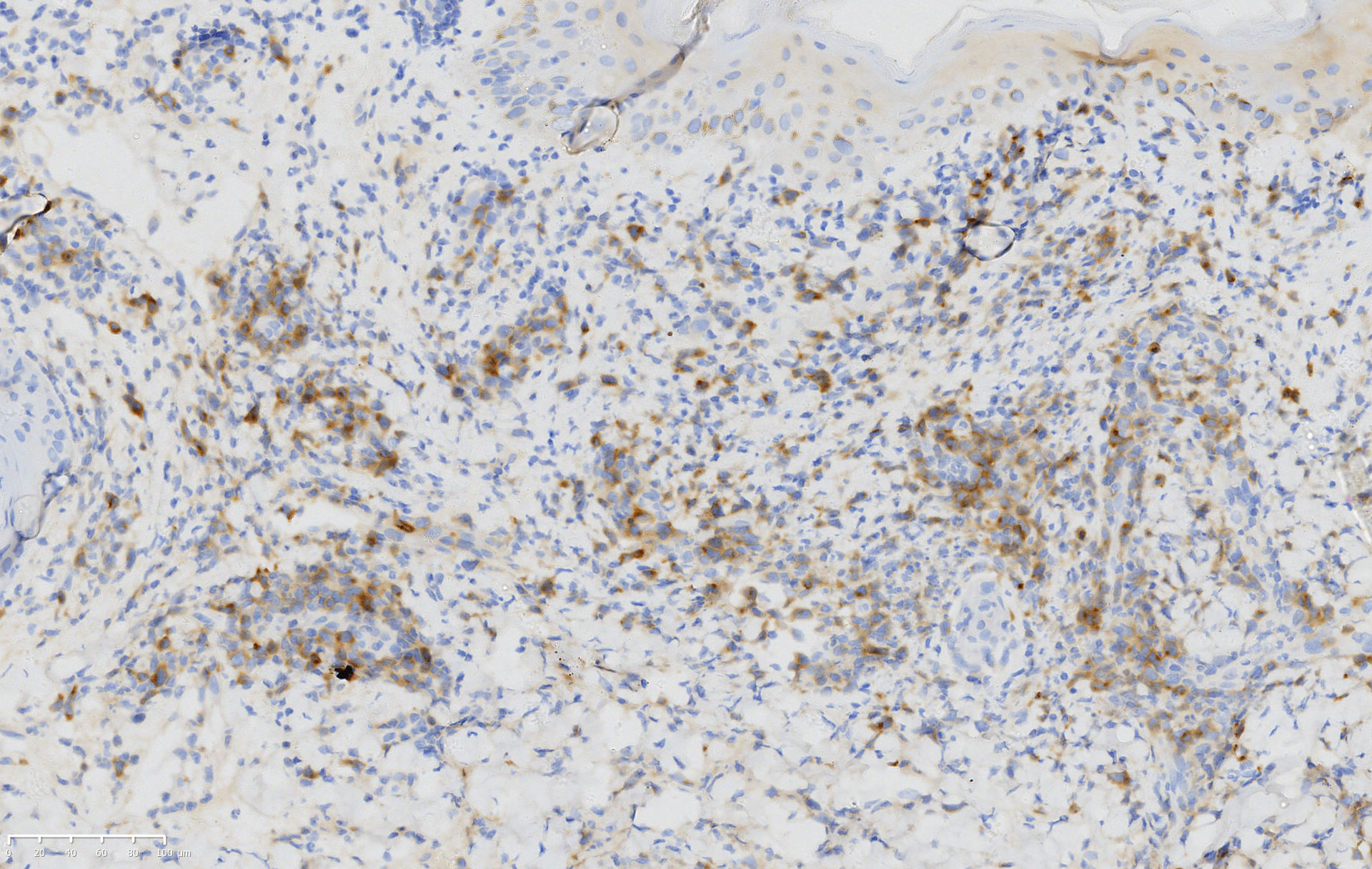
- Atypical lymphoid cells positive for clusters of differentiation 30 in the biopsy (clusters of differentiation 30, ×200)
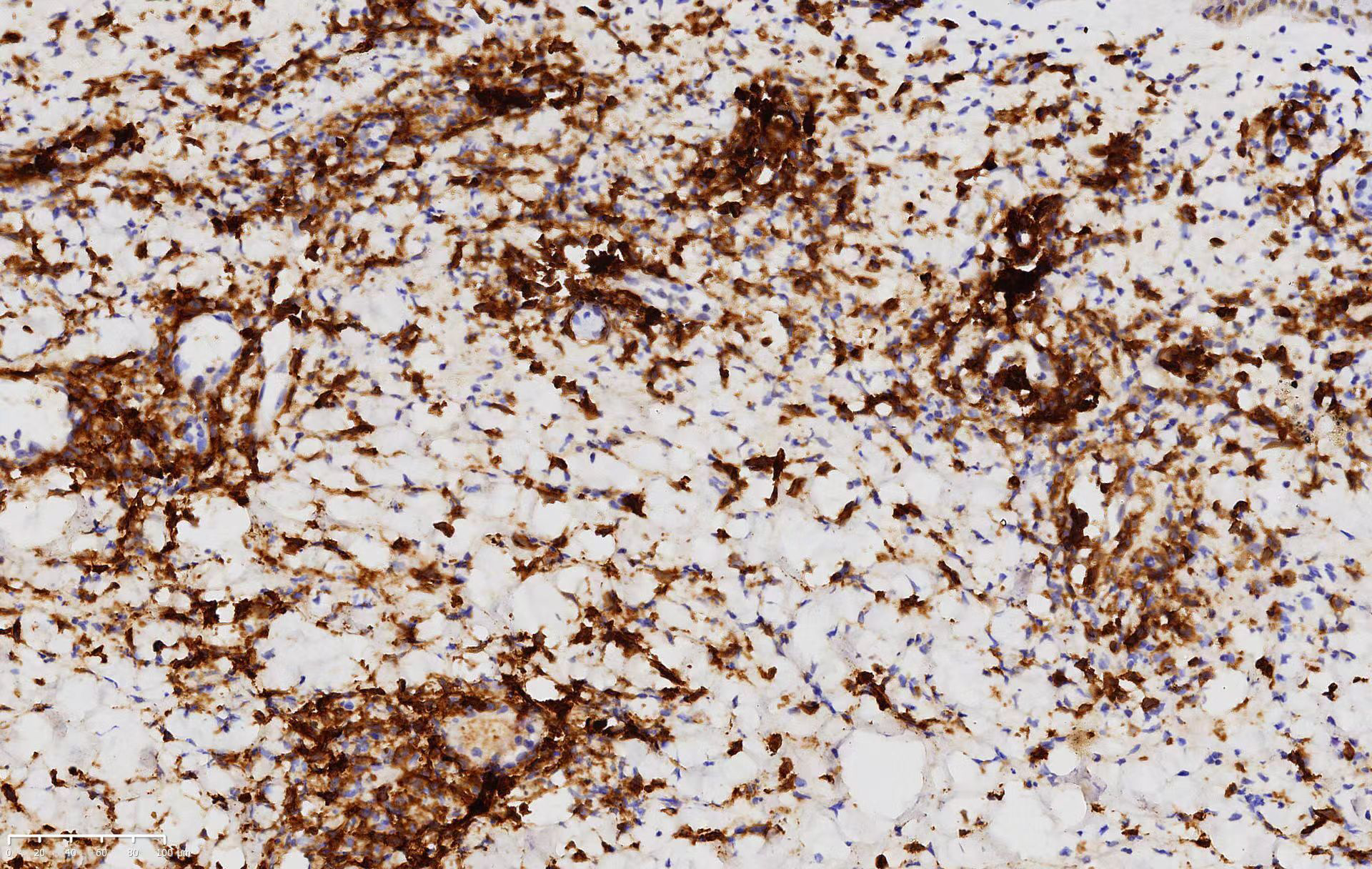
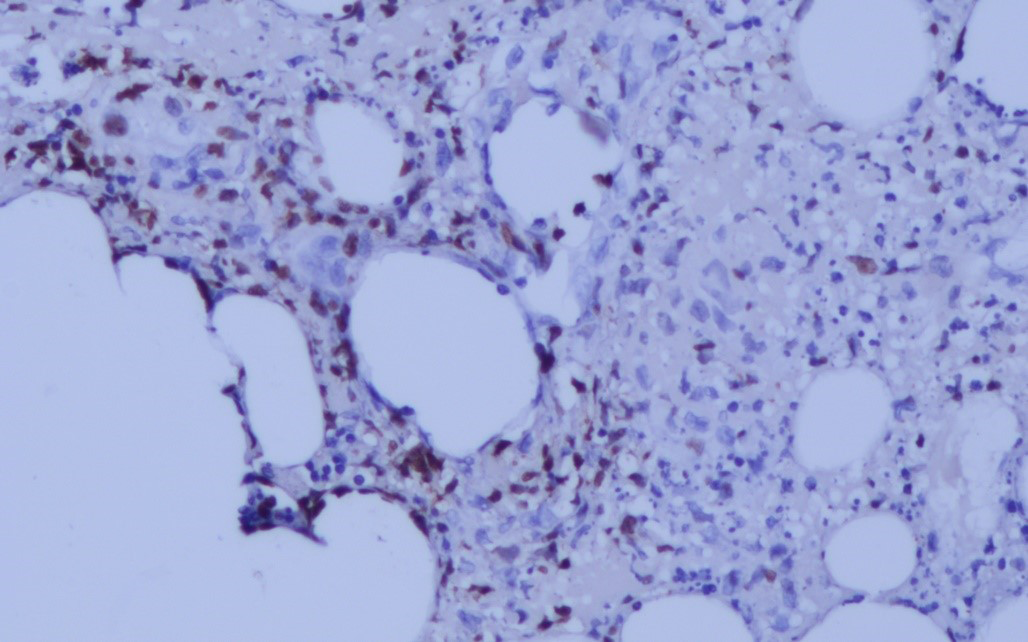
The patient later developed cough, sore throat and intermittent fever up to 39.0°C, with progressively worsening of skin lesions. Laryngoscopy revealed a mass in the posterior pharyngeal wall; unfortunately, no biopsy specimen was obtained. On the 5th day of hospital stay, patient had a sudden intestinal perforation for which surgery was performed. The histopathological examination and immunohistochemical staining on the resected small intestinal tissue confirmed the diagnosis of extranodal NK/T cell lymphoma. Histopathological findings resembled the skin biopsy findings [Figures 5a and 5b]. Immunohistochemistry indicated that the atypical lymphocytes were positive for CD3, CD56, T-cell intracellular antigen 1, Epstein-Barr virus-encoded small RNAs, and perforin B, confirming a natural killer cell phenotype [Figures 5c–5f]. The Epstein-Barr virus-encoded small RNAs in situ hybridisation was positive for atypical lymphocytes. The proliferation marker, Ki-67, was positive in approximately 60.0% of the cells. These findings supported the diagnosis of secondary cutaneous extranodal NK/T-cell lymphoma.
- Biopsy scan of the small intestine tissue (H and E, × 40)
- Biopsy of the small intestine tissue, showing atypical lymphoid cells mixed with inflammatory cells (H and E, ×100)
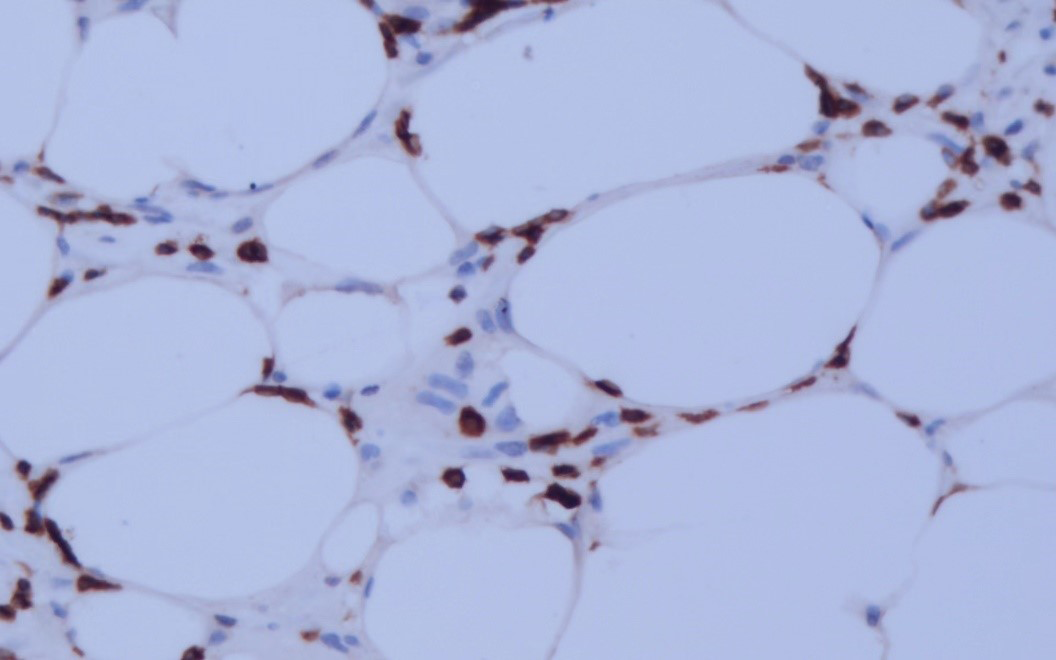
- Atypical lymphoid cells partial positive for CD3 in the biopsy (CD3, ×200)
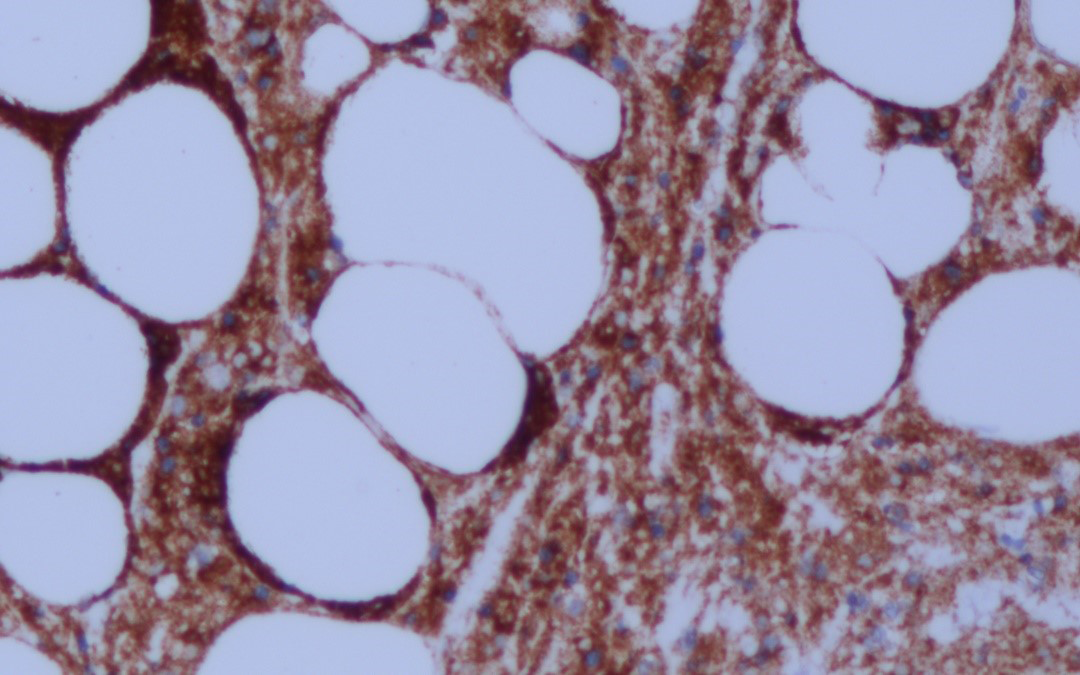
- Atypical lymphoid cells partial positive for CD56 in the biopsy (CD56, ×200)
- Atypical lymphoid cells partial positive for Epstein-Barr encoding region (EBER) in the biopsy (EBER, ×200)
- Atypical lymphoid cells partial positive for Granulase B in the biopsy (Granulase B, ×200)
After consultation with oncologists and haematologists, we proposed further investigations to define the lymphoma stage, but the patient refused. The patient experienced rapid disease progression, followed by death 3 months after the diagnosis.
Extranodal NK/T-cell lymphoma is a rare non-Hodgkin’s lymphoma associated with Epstein–Barr viral infection, with regional and ethnic differences, high recurrence and poor prognosis. It is mainly prevalent in East Asia and parts of Central and South America.1 The median survival time is only 5.3 months, and the 5-year overall survival rate is 49.9 ± 12.5%.2 Extranodal NK/T-cell lymphomas involving the skin and digestive tract are rare.
Extranodal NK/T-cell lymphoma mainly involves the lower limbs when it affects the skin. Patients often exhibit cellulitis, nodules, skin ulcers and vasculitic lesions.3 Extranodal NK/T-cell lymphoma mainly invades the colon when affecting the digestive tract, with atypical clinical features. Evident symptoms include abdominal pain, bloody stool, abdominal mass, weight loss, intestinal obstruction and intestinal perforation, of which intestinal perforation occurs in only 8.7% (92/1062) of cases.4 Early diagnosis is nearly impossible without specific symptoms and examinations and most patients undergo emergency surgery for intestinal perforation. Moreover, anticancer treatment is delayed in patients with intestinal perforation with severe peritonitis, gastrointestinal bleeding, septic shock and multiple organ failure, resulting in an extremely poor prognosis. Therefore, early diagnosis and surgical treatment of patients with extranodal NK/T-cell lymphoma are crucial before intestinal perforation occurs.
The diagnosis depends on histopathological and immunohistochemical findings. The examination of Epstein-Barr virus-encoded small RNAs in situ hybridisation is often used in diagnosing Epstein–Barr virus-related infections and is an important auxiliary method for diagnosing extranodal NK/T-cell lymphoma. Li et al. reported that the expression rate of Epstein-Barr virus-encoded small RNAs in patients with extranodal NK/T-cell lymphoma in Xinjiang was 94.2% (97/103).7 The prognosis of patients with extranodal NK/T-cell lymphoma is closely associated with disease location also. The median survival of patients presenting with the skin-limited disease is 27 months (95% confidence interval 9–45) and only 4 months (95% confidence interval 3–5) for those presenting with both cutaneous and extracutaneous involvement.8 A study found that the median survival time of patients with intestinal extranodal NK/T-cell lymphoma was 2.8 months (95% confidence interval 0.3–29), while that of patients with intestinal perforation was only 1.5 months (95% confidence interval 0.3–2.7).9 Other adverse prognostic factors include B symptoms, elevated lactate dehydrogenase levels, decreased albumin levels, advanced disease, extranodal involvement, and Epstein–Barr virus load in the tissues. Our patient had typical B symptoms, an increased lactate dehydrogenase level and a decreased albumin level.
Acknowledgement
We thank Dr. Kang for her excellent comments and Dr. Zhang for helpful guidance on the pathological pictures.
Declaration of patient consent
The authors certify that they have obtained the patient’s consent.
Financial support and sponsorship
Xinjiang Uygur Autonomous Region Key R & D program under Grant 2021B03001.
Conflict of interest
There are no conflicts of interest.
References
- Extranodal natural killer cell/t-cell lymphoma, nasal type, presenting as cutaneous nodules and a small-bowel perforation. Am J Dermatopathol. 2010;32:83-5.
- [CrossRef] [PubMed] [Google Scholar]
- SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study group. Blood. 2012;120:2973-80.
- [CrossRef] [PubMed] [Google Scholar]
- A case of extranodal natural killer/T-cell lymphoma, initially misdiagnosed as erythema nodosum. Indian J Dermatol Venereol Leprol. 2020;86:715-8.
- [CrossRef] [PubMed] [Google Scholar]
- Bowel perforation in intestinal lymphoma: Incidence and clinical features. Ann Oncol. 2013;24:2439-43.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- CD30 expression and survival in extranodal NK/T-cell lymphoma: A systematic review and meta-analysis. Oncotarget. 2018;9:16547-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Both c-Myc and Ki-67 expression are predictive markers in patients with extranodal NK/T-cell lymphoma, nasal type: A retrospective study in China. Pathol Res Pract. 2014;210:351-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathologic, immunophenotypic, and EBER in situ hybridisation study of extranodal natural killer/T-cell lymphoma, nasal type in ãmulti-ethnic groups. Clin Lab. 2014;60:419-5.
- [CrossRef] [PubMed] [Google Scholar]
- NK/T-cell lymphoma, nasal type, γδ T-cell lymphoma, and CD8-positive epidermotropic T-cell lymphoma-clinical and histopathologic features, differential diagnosis, and treatment. Semin Cutan Med Surg. 2018;37:30-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prognostic characteristics of gastrointestinal tract NK/T-cell lymphoma: an analysis of 47 patients in China. J Clin Gastroenterol. 2013;47:e74-9.
- [CrossRef] [PubMed] [Google Scholar]





