Translate this page into:
Eyelid involvement in disseminated chronic cutaneous lupus erythematosus
2 Department of Ophthalmology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India
Correspondence Address:
A Singal
B-14, Law Apartments, Karkardooma, Delhi - 110 092
India
| How to cite this article: Pandhi D, Singal A, Rohtagi J. Eyelid involvement in disseminated chronic cutaneous lupus erythematosus. Indian J Dermatol Venereol Leprol 2006;72:370-372 |
Abstract
Eye involvement in chronic cutaneous lupus erythematosus (CCLE) has been reported infrequently. We describe two cases of disseminated CCLE, a 50-year-old woman and a 45-year-old man, with eyelid involvement and disease duration of 4 and 20 years respectively. The first patient showed an excellent response to chloroquine while there was lack of response in the second patient.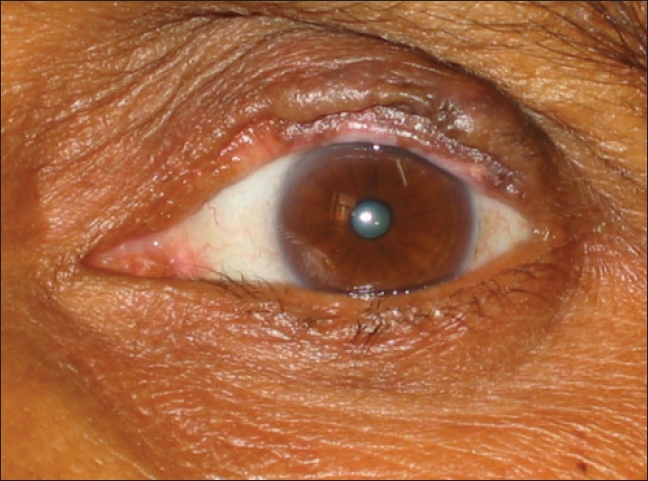 |
| Case 1 - Depressed plaque on left upper eyelid with rounded lid margin, madarosis and trichiasis |
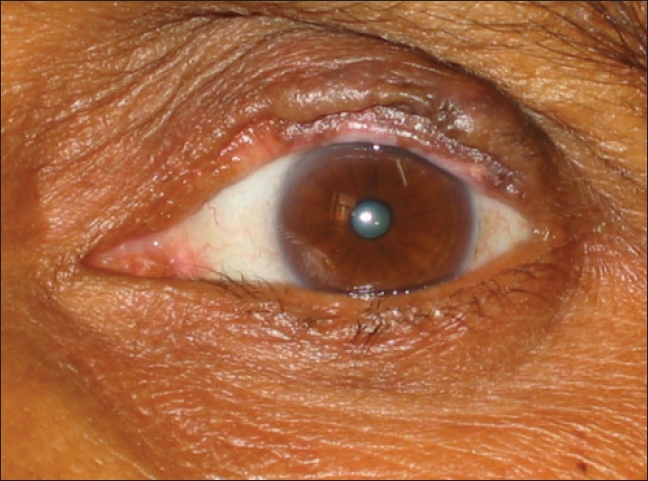 |
| Case 1 - Depressed plaque on left upper eyelid with rounded lid margin, madarosis and trichiasis |
Introduction
Eye involvement in chronic cutaneous lupus erythematosus (CCLE) was first described in 1932. Since then it has been infrequently documented in literature as ophthalmologic examination is often overlooked by the dermatologists. Eyelid involvement responds well to chloroquine, if started early in the course of the disease. However, delay in the recognition of eye lesions and institution of specific therapy leads to poor outcome and permanent sequelae.[1],[2],[3],[4] We highlight the role of chloroquine in the treatment of eye lesions in two adult patients.
Case reports
Case 1 A 50-year-old woman presented to the dermatology outpatient department with gradually progressive, scaly, erythematous raised lesions on the face, neck and scalp of two years duration. They healed with atrophic scarring following topical steroid therapy. Six months earlier similar lesions had appeared on the lower lip and forearm that flared following sun exposure. She also complained of sporadic redness, itching, swelling and watering of eyes for the past four years for which she was prescribed steroid and antibiotic eye drops with the presumptive diagnosis of chronic blepharitis. She gave history of burning sensation in mouth on intake of spicy food.
The general physical examination was unremarkable. There was an erythematous plaque with marginal hyperpigmentation, telangiectases and adherent crusts on the lower lip. Similar multifocal lesions on the scalp were associated with atrophy, crusting and alopecia. The eyelids had depressed plaques on upper lid margins, extending from the eyelash line to posterior lid margins, with madarosis, trichiasis and destruction of the meibomian duct ostia [Figure - 1]. There was evidence of mild dry eye. Tear break-up time was reduced to 4-6 seconds, but the Schirmer and the basal secretion tests were normal. No abnormality was detected on direct and indirect ophthalmoscopy. The oral cavity had multiple erosions on the hard palate and violaceous plaques on the buccal mucosae.
Hematological, biochemical and serological tests for ANA, anti-dsDNA and rheumatoid factor were normal. Skin biopsy and direct immunofluorescence findings from the lower lip were diagnostic of discoid lupus erythematosus. The patient was started on chloroquine phosphate 250 mg twice daily and artificial tears. The skin and eye lesions regressed completely by two and four months respectively. The eyelid lesions healed with linear depressed scars on lid margins. The madarosis improved and trichiasis disappeared. Tear break-up time improved to 30 and 20 seconds in the right and left eye respectively.
Case 2 A 45-year-old man presented with multiple lesions on the face, scalp, trunk and upper limbs of 20 years duration for which he was on intermittent topical steroid therapy. All plaques had well-defined margins, depigmentation, adherent scale, follicular plugging, leukotrichia and atrophy. He complained of photosensitivity, periodic irritation and watering of eyes of similar duration for which he was prescribed symptomatic treatment by an ophthalmologist. Examination revealed erythematous and depigmented patches over upper and lower eyelids with thickening of lid margins, madarosis, loss of meibomian duct opening, trichiasis, erosions on lid margin and entropion in right eye. Corrected visual acuity was 6/18 and 6/6 in the right and left eye respectively. Fundus examination was unremarkable and tear break-up time was 5-6 seconds in both eyes requiring artificial tears.
Detailed clinical, hematological and radiological parameters did not indicate systemic involvement. Serological tests revealed a positive ANA but anti-dsDNA was negative. The skin biopsy and direct immunofluorescence were consistent with a diagnosis of chronic cutaneous lupus erythematosus. The patient had been irregularly treated with clofazimine, 100 mg twice daily and weekly steroid pulses (4 mg betamethasone in tapering doses) for about one year with no improvement. He was started on chloroquine, 250 mg twice daily following ophthalmic evaluation. After one year, he felt symptomatically better, lid margin erosions healed, thickening of lid margin reduced but entropion, madarosis and depigmentation persisted.
Discussion
CCLE is a predominantly cutaneous disease, although 25% patients may have serological abnormalities of systemic LE.[1] The presence of disseminated cutaneous lesions carries a higher rate of progression to systemic LE which may be seen in 2 to 20% patients. Lesions of the face are seen in 80 to 90% patients and mucosal involvement affecting the oral, nasal and genital mucosae is observed in 15 to 24% cases.[2] However, eyelid involvement is uncommon and when present alone causes diagnostic difficulty. The first report of conjunctival involvement dates back to 1932 when Klauder and Delong first described a dark red, atrophic, velvety conjunctivitis.[3] Since then a little over 20 cases have been documented in English dermatologic literature.[4] This may be an underestimate as Burge et al . detected eyelid involvement in 6% of patients in their series of CCLE.[5] The average duration before correct diagnosis for eye lesions in CCLE is two-three years.[2]
Eye lesions in CCLE are mostly asymptomatic and can lead to complications like loss of lid tissue, disorganization of mucocutaneous junction, loss of lashes, ectropion, entropion and symblepharon due to chronic inflammation of the deeper corium.[2],[5],[6] Less commonly, involvement can be in the form of hypertrophic conjunctival lesions, chronic blepharitis, dry eye or as an overlap with lichen planus.[2],[7],[8],[9] Periorbital edema has been the presenting feature in patients with lupus panniculitis.[4] Characteristically, in both our patients, no conjunctival lesions were seen although they had an evidence of mild dry eye.
There are a few reports describing eye lesions as a marker for progression to systemic LE.[2] Paroli et al . described a patient of SLE, in remission for 15 years, where chorioretinopathy and lid lesions were the only sign of relapse.[10] Frith et al . documented conjunctival linear immuno-deposits on direct immunofluorescence in 48% of uninvolved bulbar conjunctiva but only rarely in the uninvolved skin or lip and postulated that either circulating antibodies bind more readily to the conjunctiva or clear less rapidly.[9] Therefore, periodic ophthalmologic evaluation of patients in remission may facilitate early detection of disease activity.
The differential diagnoses for eyelid lesions include rosacea, contact allergic dermatitis, tinea faciei, polymorphous light eruption, cutaneous lymphocytic infiltrates, lichen planus and cicatricial pemphigoid.[2] Gratifying results have been reported with chloroquine in up to 70% patients.[11] It was first used for eye lesions in 1982 with excellent response.[12] As is evident in case 1, there was symptomatic relief and objective reduction in all lesions including eyelid plaques. In case 2, the entropion persisted and reduction was less evident and will require surgical correction. This may be attributed to the long duration of the disease and the failure to establish a correlation between the eye and skin disease. Other therapies tried include topical, intralesional or oral steroids with variable results.[2],[5]
All patients with CCLE should be screened for ophthalmologic involvement. Those with eye lesions should undergo periodic clinical examination to identify recurrence and to institute early treatment in order to prevent complications and, also to screen for systemic involvement. Early institution of chloroquine therapy may prevent or decrease permanent disfigurement of the eye.
| 1. |
Dubois EL, Martel S. Discoid lupus erythematosus: Analysis of its systemic manifestation. Ann Intern Med 1956;44:482.
[Google Scholar]
|
| 2. |
Donzis PB, Insler MS, Buntin DM, Gately LE. Discoid lupus erythematosus involving the eyelids. Am J Ophthalmol 1984;98:32-6.
[Google Scholar]
|
| 3. |
Klauder JV, Delong P. Lupus erythematosus of conjunctiva, eyelids and lid margins. Arch Ophthalmol 1932;7:856-67.
[Google Scholar]
|
| 4. |
Inuzuka M, Tomita K, Tokura Y, Takigawa M. Lupus erythematosus profundus with unusual skin manifestation: Subcutaneous nodules coexisting with eyelid plaques. J Dermatol 2001;28: 437-41.
[Google Scholar]
|
| 5. |
Burge SM, Frith PA, Juniper RP, Wojnarowska F. Mucosal involvement in systemic and chronic cutaneous lupus erythematosus. Br J Dermatol 1989;121:727-41.
[Google Scholar]
|
| 6. |
Kearms W, Wood W, Marchese A. Chronic cutaneous lupus involving the eye lid. Ann Ophthalmol 1982;14:1009-10.
[Google Scholar]
|
| 7. |
Uy HS, Pineda R 2nd, Shore JW, Polcharoen W, Jakobiec FA, Foster CS. Hypertrophic discoid lupus erythematosus of the conjunctiva. Am J Ophthalmol 1999;127:604-5.
[Google Scholar]
|
| 8. |
Chung MS, Drube WT Jr. Patient with lichen planus and conjunctival immunopathologic features of lupus erythematosus. Am J Ophthalmol 1999;128:364-5.
[Google Scholar]
|
| 9. |
Frith P, Burge SM, Millard PR, Wojnarowska F. External ocular findings in lupus erythematosus: A clinical and immunopathological study. Br J Ophthalmol 1990;74:163-7.
[Google Scholar]
|
| 10. |
Paroli MP, Riso D, Pinca M, Pivette-Pezzi P. Chorioretinopathy and discoid plaques like lesions of the eyelids as useful indicators of systemic lupus erythamatosus progression. Lupus 2001;10:571-5.
[Google Scholar]
|
| 11. |
Callen JP. Chronic cutaneous lupus erythematosus. Clinical, laboratory, therapeutic, and prognostic examination of 62 patients. Arch Dermatol 1982;118:412-6.
[Google Scholar]
|
| 12. |
Nowinski T, Bernardino V, Naidoff M, Parrish R. Ocular involvement in lupus erythematosus profondus (Panniculitis). Ophthalmology 1982;89:1149-51.
[Google Scholar]
|
Fulltext Views
3,116
PDF downloads
957





