Translate this page into:
Familial leiomyomatosis cutis affecting nine family members in two successive generations including four cases of Reed's syndrome
2 Department of Radiology, North Bengal Medical College, Darjeeling, West Bengal, India
3 Department of Dermatology, Venereology, and Leprosy, R. G. Kar Medical College, Kolkata, West Bengal, India
4 Department of Dermatology, Venereology, and Leprosy, Katihar Medical College, Katihar, Bihar, India
Correspondence Address:
Rajesh Kumar Mandal
Department of Dermatology, Venereology, and Leprosy, North Bengal Medical College, Darjeeling, West Bengal
India
| How to cite this article: Mandal RK, Koley S, Banerjee S, Kabiraj SP, Ghosh SK, Kumar P. Familial leiomyomatosis cutis affecting nine family members in two successive generations including four cases of Reed's syndrome. Indian J Dermatol Venereol Leprol 2013;79:83-87 |
Abstract
Reed's syndrome or familial leiomyomatosis cutis et uteri is an autosomal dominant disorder, characterized by multiple cutaneous and uterine leiomyomas. We report here a case of a 53-year-old woman who presented to us with multiple painful nodules over different parts of her body. Based on the histopathological examination, imaging, and past medical records, a diagnosis of Reed's syndrome was made. Three of her sisters had similar disease. Subsequently, it was found that a total of nine members of their family in two successive generations were affected with cutaneous leiomyomas. The present case series has been reported for its interesting clinical presentations and rarity.Introduction
Cutaneous leiomyomas are relatively rare, benign, smooth muscle tumors. They are divided into three types, namely, piloleiomyoma (arising from arrector pili muscle of hair follicle), genital leiomyoma (arising from tunica dartos of scrotum and mammary muscles of nipples), and angioleiomyoma (arising from smooth muscles of blood vessels). [1] They may be asymptomatic or painful at presentation. Reed′s syndrome or familial leiomyomatosis cutis et uteri is an extremely rare autosomal dominant condition, characterized by multiple cutaneous and uterine leiomyomas. [2] A subset of patients with Reed′s syndrome is predisposed to develop papillary renal cell carcinoma, necessitating evaluation of all patients for the presence of an occult renal malignancy. [3] So far, only a few sporadic cases of Reed′s syndrome have been reported from India. [4],[5]
Case Report
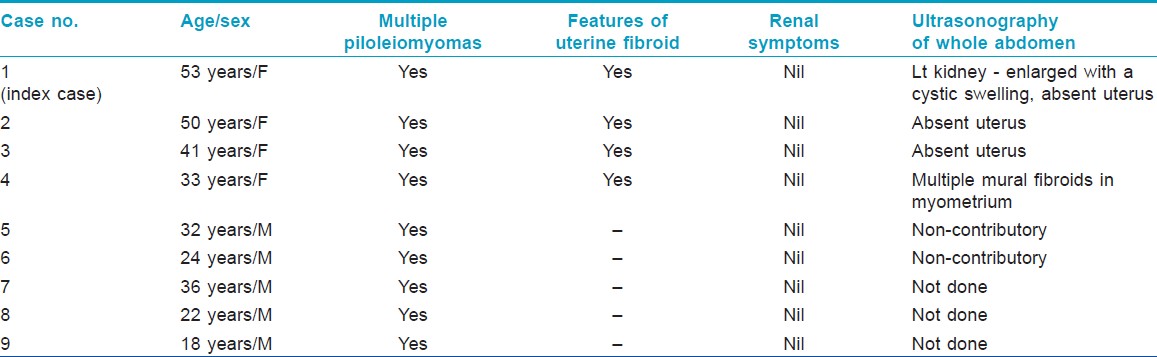
A 53-year-old woman presented to us with multiple painful nodules over different parts of her body. The nodules were present since her childhood and were gradually being increased in number and size. Nine members of her family (including three of her sisters and one brother) in two successive generations [Figure - 1] had similar cutaneous lesions [Table - 1]. The index case and two of her sisters had past history of significant menorrhagia and lower abdominal pain, for which they had undergone hysterectomy in their mid-thirties with the diagnosis of uterine leiomyomas. Her youngest sister, a 33-year-old woman, was also being investigated for menorrhagia and lower abdominal pain. Rest of the history was unremarkable.
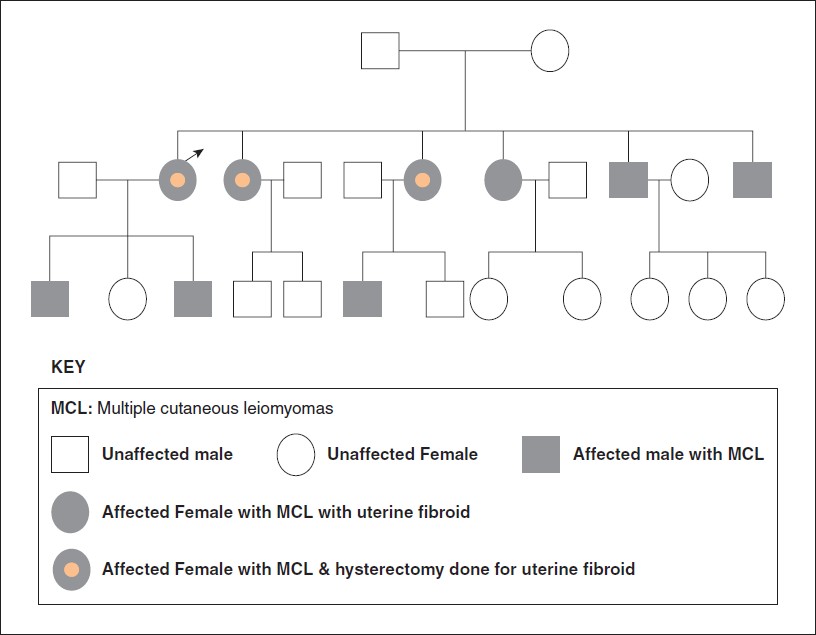 |
| Figure 1: Pedigree chart showing nine affected members in two successive generations |
On mucocutaneous examination, multiple flesh-colored, rubbery, tender, smooth-surfaced nodules (ranging in diameter from 0.5 cm to 3 cm) were noticed over different parts of her body [Figure - 2]. Similar lesions were also noted in the other affected family members [Figure - 3]. Rest of the mucocutaneous and systemic examinations were noncontributory. The findings of excision biopsy from a nodule showed encapsulated tumors in the dermis composed of interlacing fascicles of smooth muscles exhibiting eosinophilic cytoplasm and blunt-ended nuclei [Figure - 4]. Masson′s trichrome stained the smooth muscles dark red [Figure - 5].
 |
| Figure 2: (a) Multiple flesh-colored, rubbery, tender, smooth-surfaced nodules. (b) Close-up of the nodules |
 |
| Figure 3: (a-d) Multiple piloleiomyomas in different family members |
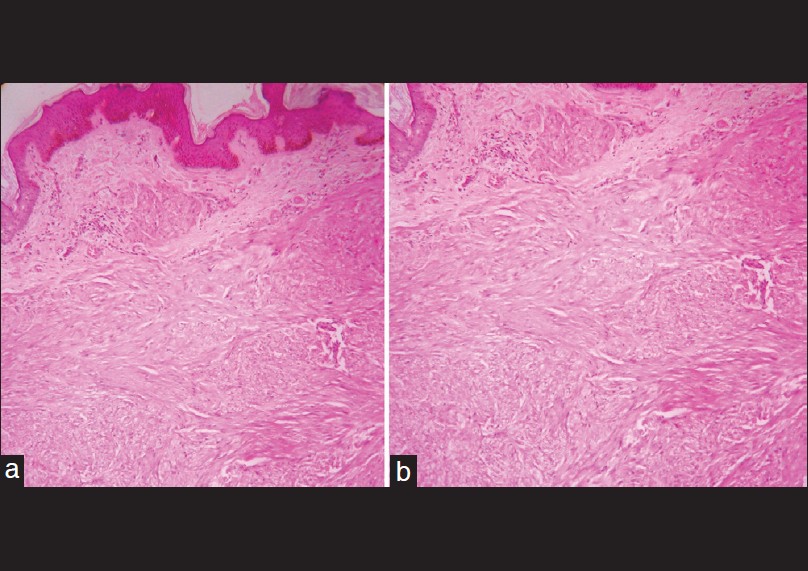 |
| Figure 4: (a) Smooth muscle fibers intermingled with collagen (H and E, × 100), (b) Muscle fibers with elongated nucleus with blunt ends (H and E, × 100) |
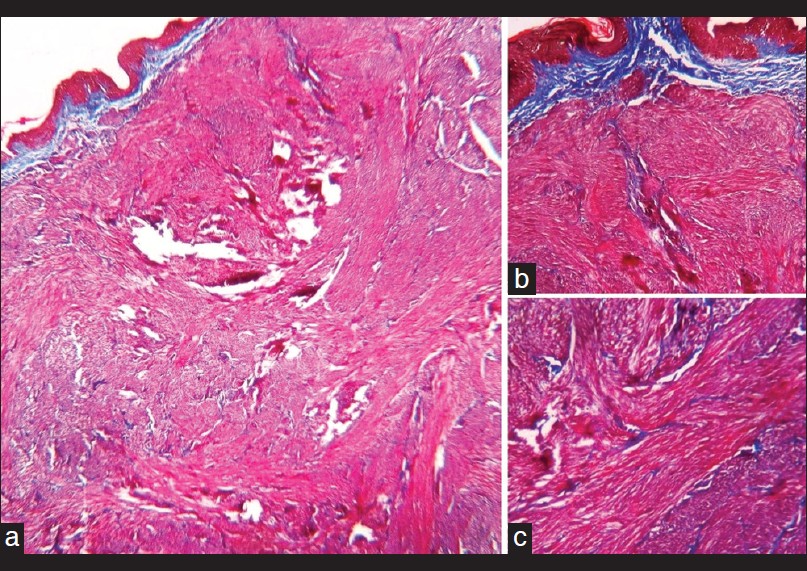 |
| Figure 5: Dark red staining of the smooth muscles. (a) Masson's trichrome, × 40. (b) Masson's trichrome, × 100. (c) Masson's trichrome, × 400 |
We could perform excisional biopsy from a cutaneous nodule in another sister of the index case which showed similar histopathological features. All the affected family members were screened for the presence of renal carcinoma. Routine blood examination, liver function test, and renal profile including urine examinations did not reveal any abnormality. Abdominal ultrasonography of the youngest sister revealed 10-12 mm mural fibroids in uterine myometrium. Ultrasonographic examination revealed enlarged left kidney with a cystic lesion in the eldest sister [Figure - 6], rest of them did not show any abnormal change or mass in kidney.
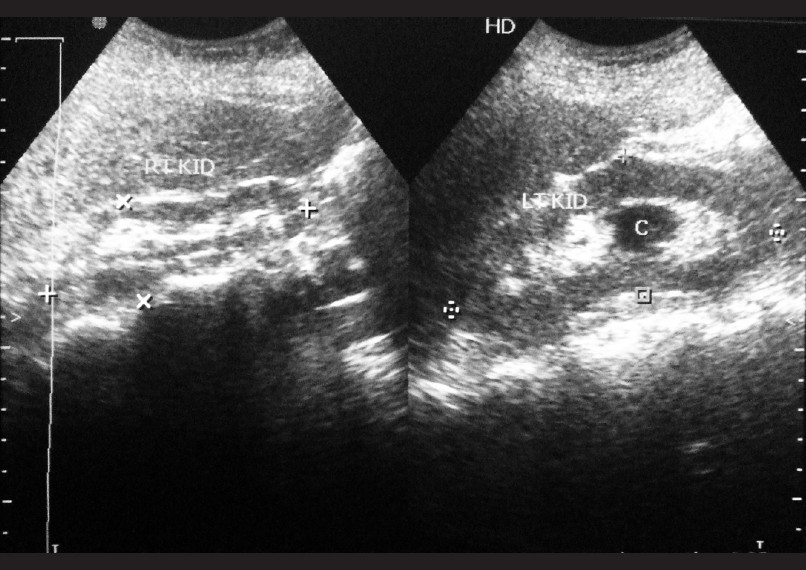 |
| Figure 6: Ultrasonography showing enlarged left kidney with small cystic mass |
The patient was referred to an urologist for the evaluation of the cystic lesion in kidney who excluded any malignancy.
Based on the clinical findings, laboratory investigations, and imaging, a diagnosis of familial leiomyomatosis cutis affecting nine family members in two successive generations including four cases of Reed′s syndrome was made. We have prescribed oral nifedepine to our index case and referred her to our colleagues of plastic surgery department for further management of the cutaneous lesions.
Discussion
Clinically, piloleiomyomas manifest as small, smooth-surfaced, skin-colored or brown papules or nodules of varying size ranging from 0.2 to 2.0 cm diameter. They usually involve patients in the age group of 10-30 years. The lesions may be solitary or multiple and are distributed mostly over extremities, trunk, neck, and face. Usually, the lesions are tender, soft or firm in consistency, and without any fixity to the underlying tissues. Pain may be induced by cold, tactile, or emotional stimuli. [2] Pseudo-Darier sign, a transient piloerection or elevation of a lesion induced by rubbing, may be present. Leiomyoma may be present in linear or dermatomal distribution or even it can be disseminated in nature. [6] The other conditions that present with painful cutaneous tumors, such as, angiolipoma, neuroma, glomus tumor, eccrine spiradenoma, and blue rubber bleb nevus should be considered in the clinical differential diagnosis of leiomyoma cutis. The occurrence of multiple cases of leiomyomas in families has been described as autosomal dominant inheritance with incomplete penetrance. [7] Familial leiomyomatosis cutis et uteri or Reed′s syndrome is characterized by simultaneous presence of cutaneous and uterine leiomyomas. [3] Affected females develop uterine fibroids (leiomyomas) that are usually larger and more numerous and appear earlier than those in the general population. [2] Uterine leiomyomas may present with menorrhagia, dysmenorrhea, urinary frequency, pain, infertility, or a palpable abdomino-pelvic mass, depending on the size, location, and number of tumors. [8]
Association of Reed′s syndrome with papillary renal cell carcinoma has been postulated, and aggressive renal carcinoma may be a part of the complex, termed as hereditary leiomyomatosis and renal cell cancer (HLRCC). [3] Although abdominal ultrasonography in our index patient revealed presence of a renal cyst, there was no evidence of malignancy. The gene responsible for Reed′s syndrome has been localized to chromosome 1q42.3-43.
This gene encodes an enzyme, fumarate hydratase (FH), an active enzyme in the Krebs cycle that converts fumarate to malate. It is also thought to act as a tumor suppressor gene. [9] Another proposed mechanism of developing Reed syndrome is pseudohypoxia (due to defective enzymatic metabolism) leading to cellular transformation and tumorigenesis. [10]
The diagnosis of leiomyoma cutis may be suspected clinically and is confirmed histopathologically, which shows proliferation of smooth muscle bundles with varying amount of intermingled collagen in the dermis. The smooth muscle cells, described as cigar-shaped, consist of eosinophilic cytoplasm with an elongated nucleus with blunt ends. Masson′s trichrome may be used to differentiate smooth muscle (red) from collagen (blue-green); both smooth muscle and collagen appear pink-red on hematoxylin and eosin stain. They also stain positively for markers of smooth muscle differentiation (desmin and actin). [2],[ 9] One limitation of the present report is that we could perform histopathological confirmation in only two patients.
Uterine leiomyomas may show hyaline or myxoid degeneration, calcification, cystic degeneration, and red (hemorrhagic) degeneration. [8] Unlike cutaneous leiomyomas, uterine leiomyomas show positive staining for estrogen and progesterone receptors. [2] Magnetic resonance imaging (MRI) is currently considered to be the most accurate imaging technique for the detection and localization of uterine leiomyomas and well-circumscribed masses of homogeneously decreased signal intensity compared with that of the outer myometrium on T2-weighted images is the usual finding in a non-degenerated leiomyomas. [8] Decreased FH enzyme activity in cultured skin fibroblasts or lymphoblastoid cells is another method of diagnosis, but is rarely needed. [2] Detailed physical examination including pelvic examination, pelvic and renal ultrasonography, urinalysis, and referral to an urologist is recommended. [2],[9] The finding of cutaneous leiomyomas with concomitant erythrocytosis has been described and is explained by an effect of the "erythropoietin-like" behavior of the tumor. [7] However, we did not find any such association in our patients.
Treatment of cutaneous leiomyomas depends on the number of lesions and the degree of discomfort to the patient. As it is a benign condition, the avoidance of the precipitating factors, such as, pain, cold, and emotional stress may be the only treatment required. [2],[9] Calcium channel blockers like nifedepine can be a useful drug to reduce pain. Other drugs, such as, gabapentin [11] and doxazosin [12] have been tried with varying success. CO2 laser ablation and botulinum toxin type A injection may be tried for the control of pain. [2],[13] Solitary lesion or localized lesions can be excised surgically, with or without skin graft. [2] On the other hand, symptomatic uterine leiomyomas may be treated by conventional surgical methods (myomectomy, hysterectomy), newer surgical techniques (hysteroscopic or laparoscopic myomectomy), uterine artery embolization, or by gonadotropin-releasing hormone analogs. [8]
We seek to emphasize that any female patients with multiple cutaneous leiomyomas (MCL) should be screened for the presence of uterine leiomyomas and occult renal malignancy. At the same time, other family members should be screened for the presence of similar lesions. Urine analysis and pelvic ultrasound examination may be used as a cheap and widely available screening tool for the detection of renal malignancy. Suspected cases should be referred to an urologist for evaluation and management. The patients with MCL most commonly present to a dermatologist. Hence, dermatologists are in a crucial position to suspect and diagnose this condition and thus allowing early management.
| 1. |
Cassetty CT. Familial leiomyomatosis cutis et uteri. Dermatol Online J 2004;10:5.
[Google Scholar]
|
| 2. |
Emer JJ, Solomon S, Mercer SE. Reed's syndrome: A case of multiple cutaneous and uterine leiomyomas. J Clin Aesthet Dermatol 2011;4:37-42.
[Google Scholar]
|
| 3. |
Kiuru M, Launonen V. Hereditary leiomyomatosis and renal cell cancer (HLRCC). Curr Mol Med 2004;4:869-75.
[Google Scholar]
|
| 4. |
Rai VM, Balachandran C, Kudva R. Multiple painful nodules. Indian J Dermatol Venereol Leprol 2005;71:449-51.
[Google Scholar]
|
| 5. |
Srivastava KP, Bajaj AK. Reed's syndrome. Indian J Dermatol 2012;57:156-7.
[Google Scholar]
|
| 6. |
Sahoo B, Radotra BD, Kaur I, Kumar B. Zosteriformpilar leiomyoma. J Dermatol 2001;28:759-61.
[Google Scholar]
|
| 7. |
Jaime TJ, Jaime TJ, Melo DF, Guaraldi Bde M, Bastos Júnior Cde S, Lerer C. Do you know this syndrome? Piloleiomyoma. An Bras Dermatol 2011;86:1222-9.
[Google Scholar]
|
| 8. |
Murase E, Siegelman ES, Outwater EK, Perez-Jaffe LA, Tureck RW. Uterine leiomyomas: Histopathologicfeatures, MR imaging findings, differential diagnosis, and treatment. Radiographics 1999;19:1179-97.
[Google Scholar]
|
| 9. |
Kim G. Multiple cutaneous and uterine leiomyomatosis (Reed's syndrome). Dermatol Online J 2005;11:21.
[Google Scholar]
|
| 10. |
Sudarshan S, Pinto PA, Neckers L, Linehan WM. Mechanisms of disease: Hereditary leiomyomatosis and renal cell cancer-A distinct form of hereditary kidney cancer. Nat Clin Pract Urol 2007;4:104-10.
[Google Scholar]
|
| 11. |
Alam M, Rabinowitz AD, Engler DE. Gabapentin treatment of multiple piloleiomyoma-related pain. J Am Acad Dermatol 2002;46:S27-9.
[Google Scholar]
|
| 12. |
Batchelor RJ, Lyon CC, Highet AS. Successful treatment of pain in two patients with cutaneous leiomyomata with the oral alpha-1 adrenoceptor antagonist, doxazosin. Br J Dermatol 2004;150:775-6.
[Google Scholar]
|
| 13. |
Christenson LJ, Smith K, Arpey CJ. Treatment of multiple cutaneous leiomyomas with CO2 laser ablation. Dermatol Surg 2000;26:319-22.
[Google Scholar]
|
Fulltext Views
2,152
PDF downloads
566





