Translate this page into:
Firm asymptomatic nodule on the epigastrium in an adult male
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Neetu Bhari
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Singh S, Naveed S, Mehta N, Arava S, Bhari N. Firm asymptomatic nodule on the epigastrium in an adult male. Indian J Dermatol Venereol Leprol 2019;85:439 |
A 26-year-old man presented with a single, asymptomatic, slowly progressive, firm swelling on the epigastrium, of 18 months' duration. Cutaneous examination revealed solitary, 3×3 cm skin-colored non-tender, firm nodulo-plaque on the epigastrium [Figure - 1]. The lesion was dome-shaped and had a central umbilication. Laterally, the plaque was extending circumferentially underneath the skin with limited mobility. Other mucocutaneous and systemic examinations were within the normal limits. Dermoscopic evaluation showed a pigmented network with some structureless depigmented areas [Figure - 2]. Skin biopsy revealed pan-dermal spindle cell proliferation arranged in a storiform pattern, with infiltration into the subcutaneous tissue [Figure - 3] and [Figure - 4]. No significant pleomorphism or mitotic activity was noted on histology. The tumor cells were diffusely immunopositive for CD34 [Figure - 5].
 |
| Figure 1: Well-defined, skin-colored, firm, dome-shaped nodulo-plaque on the epigastrium |
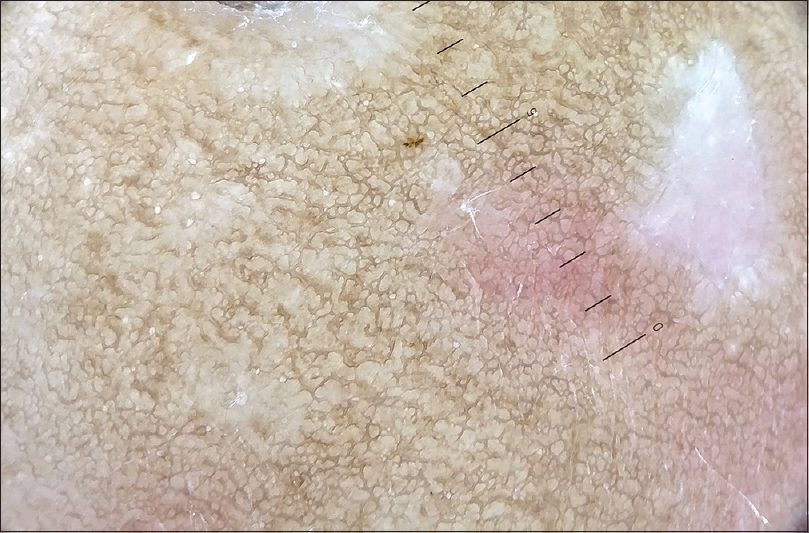 |
| Figure 2: Dermoscopy showing a pigmented network with some structureless depigmented areas (Heine Delta 20T, polarized, ×10) |
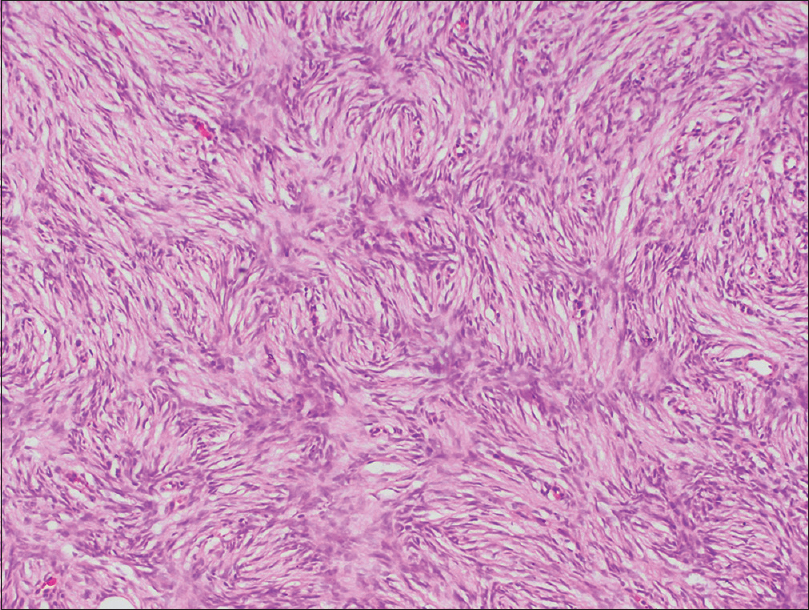 |
| Figure 3: Skin biopsy showing spindle cell proliferation arranged in a storiform pattern (hematoxylin and eosin, ×400) |
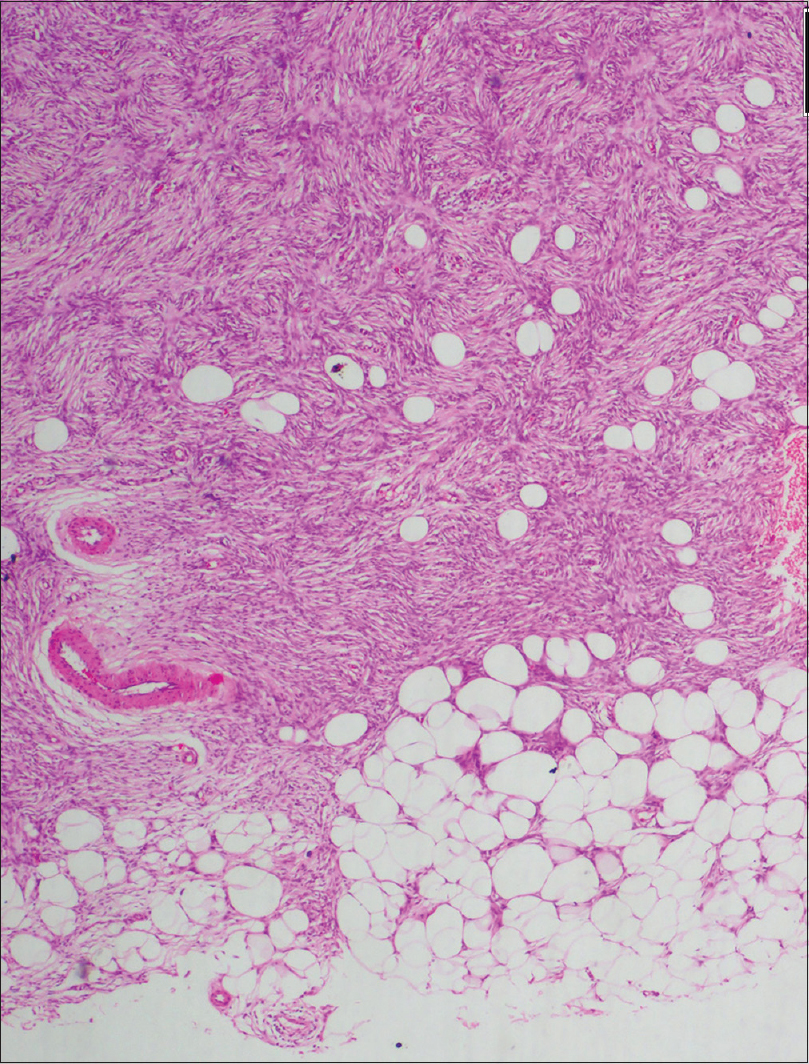 |
| Figure 4: Spindle cells infiltrating the subcutis (hematoxylin and eosin, ×100) |
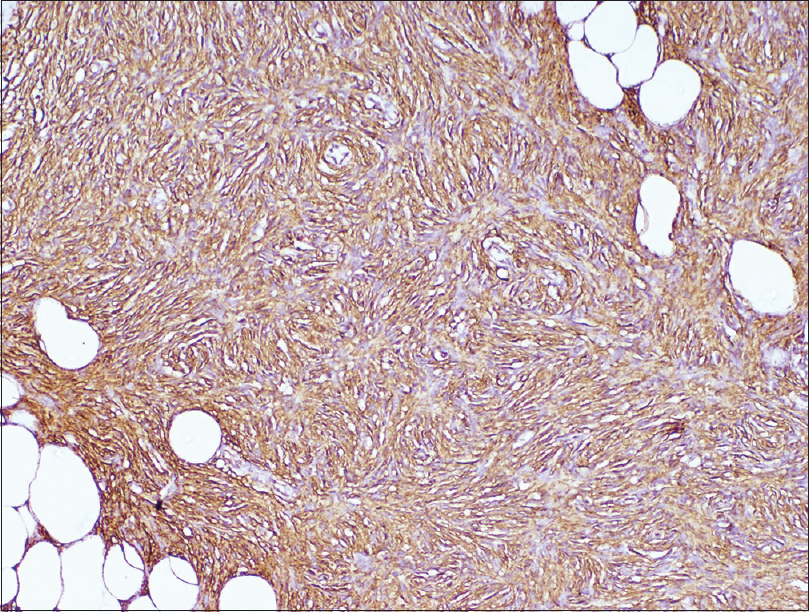 |
| Figure 5: Spindle cells showing positive staining with CD34 (CD34, ×400) |
Question
What is your diagnosis?
Answer
Dermatofibrosarcoma protuberans.
Discussion
Dermatofibrosarcoma protuberans is a relatively rare, slow-growing, locally infiltrative, fibroblastic mesenchymal tumor, that arises from the dermis and invades deeper tissues (fat, fascia, muscle and bone) with a high rate of recurrence.[1] It accounts for <0.1% of all malignancies with an annual incidence of 0.8–4.5 per million in adults.[2] The most commonly affected age group is between 30 and 50 years, although it has been reported across all age groups.[3] The precise origin of dermatofibrosarcoma protuberans is not well known, but evidence hints that the cellular origin is fibroblastic, histiocytic or neuroectodermal.[4] Many authors propose a pluripotent progenitor cell (undifferentiated mesenchymal cell) as the origin of dermatofibrosarcoma protuberans because these tumors demonstrate some features of each cellular type.[4] Over 90% of dermatofibrosarcoma protuberans are characterized by a unique chromosomal translocation t(17;22) (q22;q13). This translocation leads to fusion of the gene for platelet-derived growth factor B chain on chromosome 22 with the collagen 1 alpha 1 gene on chromosome 17. This leads to an upregulation of functional platelet-derived growth factor B, which subsequently acts as a growth factor and potent mitogen for various connective tissue cells.[2],[4]
The most commonly affected sites are the trunk (40–60%) and proximal limbs (20–30%).[5] In its earliest stage, dermatofibrosarcoma protuberans most commonly presents as an asymptomatic, skin-colored, erythematous to brown hyperpigmented plaque that slowly enlarges over months to years. The plaque may develop nodularity, or it may evolve into a telangiectatic, atrophic and/or sclerotic plaque. Rapid growth, ulceration and surface hemorrhage can also be observed.[4] The tumor is often fixed to the dermis but moves freely over deeper tissues. Fixation to deeper structures is observed only late in the course of the disease.[2] The tumor has a low chance of metastasis, either to regional lymph nodes or distantly; however, it is aggressive locally. The local recurrence rate of dermatofibrosarcoma protuberans is reported to be upto 60%, but pooled data from various studies published over the last 20 years, till 2010, has found a recurrence rate of 7.3% after wide local excision.[3]
There are four clinical variants of dermatofibrosarcoma protuberans, namely sclerotic plaque-like, keloidal-type, tumor-like and atrophic plaque form.[6] The differential diagnoses include other fibrohistiocytic neoplasms, atypical fibrosarcomas, myofibromatosis, keloids, sclerosing basal cell carcinoma, morphea, anetoderma or a scar.[6]
Histologically, dermatofibrosarcoma protuberans are characterized by dense pan-dermal proliferation of spindle cells in a storiform or cart-wheel appearance with varying degree of vascularity and collagenization.[2] The tumor cells have large nuclei and low polymorphism with infrequent mitotic figures. The maximum cellularity of tumor is seen at the center of the lesion while the edges show irregular infiltration into the surrounding dermis. The epidermis on the tumor is atrophic with flattened rete ridges. The tumor cells also invade the subcutis along the fibrous septa, and infiltrate the lobules giving a typical honeycomb-like appearance. In later stages, infiltration into fascia, muscles, periosteum and bone can also be seen. A deep punch biopsy or incisional biopsy should be performed in all cases as deeper extent of tumor provides an important clue when the clinical differential is dermatofibroma, which is a dermal tumor with a non-infiltrating border. Various immunohistochemical markers have been found to be useful in diagnosing difficult cases. It stains positively for CD34, vimentin, apolipoprotein D, nestin while there is negative staining with desmin, S100 protein, FXIIIa, stromelysin III, HMGA1 and 2, tenascin, D2-40 and CD163.[7] At times, dermoscopy can aid in making a diagnosis. Various dermoscopic features have been described, i.e. delicate pigmented network, arborizing vessels, structureless light brown areas, shiny white streaks, pink background coloration, structureless hypo- or depigmented areas or a combination of these features.[8]
Surgical excision is the treatment of choice for dermatofibrosarcoma protuberans, with complete resection and pathologically negative margins as the aim. Either wide-local excision with a margin of 2–4 cm beyond the clinically visible tumor border, down to and including the fascia; or Mohs micrographic surgery along with frozen section margin examination of sequential horizontal sections can be performed.[1] Imatinib mesylate (oral dose 800 mg/day) monotherapy is approved for the treatment of adult patients with unresectable, recurrent or metastatic dermatofibrosarcoma protuberans.[9] It has also been used as an adjuvant to the surgical management. Conventional chemotherapy and radiotherapy have limited value in the management of dermatofibrosarcoma protuberans.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Saiag P, Grob JJ, Lebbe C, Malvehy J, del Marmol V, Pehamberger H, et al. Diagnosis and treatment of dermatofibrosarcoma protuberans. European consensus-based interdisciplinary guideline. Eur J Cancer 2015;51:2604-8.
[Google Scholar]
|
| 2. |
Llombart B, Serra-Guillén C, Monteagudo C, López Guerrero JA, Sanmartín O. Dermatofibrosarcoma protuberans: A comprehensive review and update on diagnosis and management. Semin Diagn Pathol 2013;30:13-28.
[Google Scholar]
|
| 3. |
Bogucki B, Neuhaus I, Hurst EA. Dermatofibrosarcoma protuberans: A review of the literature. Dermatol Surg 2012;38:537-51.
[Google Scholar]
|
| 4. |
Dimitropoulos VA. Dermatofibrosarcoma protuberans. Dermatol Ther 2008;21:428-32.
[Google Scholar]
|
| 5. |
Criscione VD, Weinstock MA. Descriptive epidemiology of dermatofibrosarcoma protuberans in the United States, 1973 to 2002. J Am Acad Dermatol 2007;56:968-73.
[Google Scholar]
|
| 6. |
Patil P, Tambe S, Nayak C, Ramya C. Dermatofibrosarcoma protuberans in a 9-year-old child. Indian Dermatol Online J 2017;8:195-7.
[Google Scholar]
|
| 7. |
Paramythiotis D, Stavrou G, Panagiotou D, Petrakis G, Michalopoulos A. Dermatofibrosarcoma protuberans: A case report and review of the literature. Hippokratia 2016;20:80-3.
[Google Scholar]
|
| 8. |
Bernard J, Poulalhon N, Argenziano G, Debarbieux S, Dalle S, Thomas L. Dermoscopy of dermatofibrosarcoma protuberans: A study of 15 cases. Br J Dermatol 2013;169:85-90.
[Google Scholar]
|
| 9. |
McArthur GA, Demetri GD, van Oosterom A, Heinrich MC, Debiec-Rychter M, Corless CL, et al. Molecular and clinical analysis of locally advanced dermatofibrosarcoma protuberans treated with imatinib: Imatinib target exploration consortium study B2225. J Clin Oncol 2005;23:866-73.
[Google Scholar]
|
Fulltext Views
3,163
PDF downloads
2,788





