Translate this page into:
Flagellate dermatoses
Correspondence Address:
Premanshu Bhushan
Skin Institute and School of Dermatology, N-Block, Greater Kailash-1, New Delhi - 110 048
India
| How to cite this article: Bhushan P, Manjul P, Baliyan V. Flagellate dermatoses. Indian J Dermatol Venereol Leprol 2014;80:149-152 |
Introduction
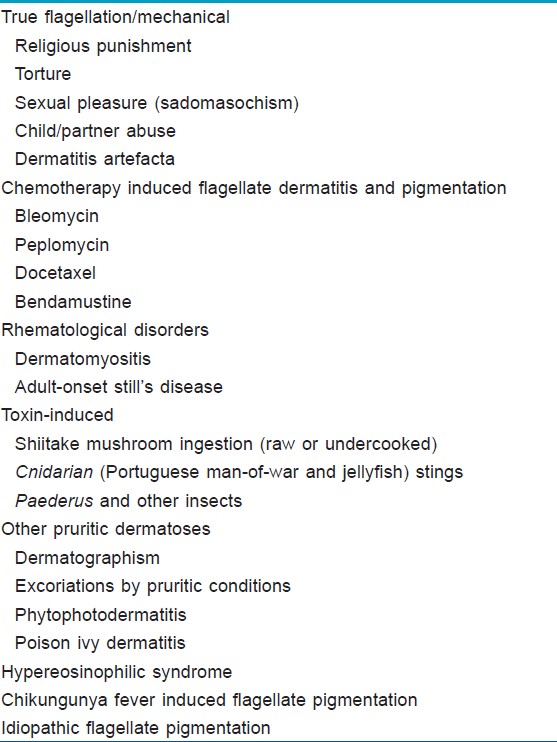
Flagellate dermatoses are uncommon figurate dermatoses characterized by parallel linear or curvilinear arrangement simulating the marks of whiplashes. The term flagellate dermatitis was originally introduced for bleomycin-induced dermatitis. However, with time other causes for this pattern have been recognized [Table - 1].
True flagellation/mechanical
Flagellation has been used in various religions for penance or punishment. [1] Whipping has also been used to "discipline" children, but in the modern context flagellate marks on children should arouse a suspicion of child abuse. [2] In adults, these could be suggestive of partner/spouse abuse or torture. Sadomasochistic behavior involves voluntary whipping of oneself or the partner for sexual gratification. [3] Artefactual whiplash marks may be produced for tangible or intangible gains in malingering and other psychiatric illnesses.
Chemotherapy induced flagellate dermatitis and pigmentation
Bleomycin is a polypeptide chemotherapeutic agent with predominant adverse reactions in the cutaneous and respiratory systems presumably due to the lack of inactivating enzyme, hydrolase in these tissues. [4] The common mucocutaneous lesions described are pigmentation (~50%), alopecia (~50%) [5] and flagellate dermatitis (8-66%). [4] This starts as diffuse, pruritic, flagellate, erythematous plaques over the trunk and extremities (scratch dermatitis) a few hours to 6 months after administration of the drug [Figure - 1]. The rash heals with persistent flagellate hyperpigmentation [Figure - 2]. Pigmentation has also been described without pruritus or rash. Although it usually appears after a cumulative dose >100 U; it has also been reported after doses as small as 14 U used for intralesional injections of verrucae. [6] The pathogenesis of bleomycin dermatitis remains speculative and various theories such as micro-trauma, inflammatory oncotaxis, increased melanogenesis, heat-recall and reduced epidermal turnover allowing prolonged melanocyte-keratinocyte contact have been proposed. [4],[7],[8] There is no specific treatment, but avoidance of bleomycin leads to eventual clearance over months to years. However, re-exposure may produce an aggravated reaction. Peplomycin is a bleomycin derivative with reduced pulmonary toxicity that is used for lymphomas and prostatic carcinoma. It has also been implicated in flagellate erythema by mechanisms similar to bleomycin. [7]
 |
| Figure 1: Bleomycin induced flagellate dermatitis |
 |
| Figure 2: Bleomycin induced flagellate pigmentation at same sites as in Figure 1 |
Docetaxel is a taxane with a high rate of cutaneous reactions including flagellate dermatitis. The reaction is apparently suppressed by corticosteroids, but withdrawal of steroids leads to reappearance of lesions. [9] Mahmoud and Eide reported a case of flagellate dermatitis from bendamustine, an alkylating agent approved in 2008 for the treatment of chronic lymphocytic leukemia and non-Hodgkin lymphoma. [10]
Rheumatological diseases
Dermatomyositis is known to produce linear lesions variously described as centripetal flagellate erythema, [11] zebra-like striped erythema, [12] and linear streaks [13] . In contrast to bleomycin-induced flagellate dermatitis, erythema is more pronounced than pigmentation. The trauma of scratching appears to play an important role, as in the bleomycin induced rash. [7] The histopathology is usually non-specific, but perinuclear vacuolization of the arrector pili muscle has been described. [14] The significance of this rash in relation to the prognosis or underlying neoplasm remains unclear. The rash generally disappears with corticosteroid therapy. [14]
Adult-onset Still′s disease is an autoimmune disease occasionally associated with flagellate erythema. Histopathology of flagellate lesions shows mild perivascular infiltration of mononuclear cells and neutrophils, along with some dyskeratotic cells in the epidermis. [15],[16]
Toxin-induced
Shiitake mushrooms (Lentinus edodes) are commonly used in Asian cuisines and are known to produce flagellate dermatitis (toxicoderma). [17] The rash is very pruritic, predominantly truncal and does not generally heal with pigmentation. [7] Toxicoderma is probably caused by a lentinan-like polysaccharide, which is denatured by cooking and thus occurs only on eating raw or under-cooked mushrooms. [17] The prick and patch tests are negative. The intermittent intake of shiitake mushrooms can delay the diagnosis by years. [18]
Cnidarians (Portuguese man-of-war and jellyfish) [19],[20],[21],[22] contain nematocysts in their tentacles which discharge by an osmotic process when injected in the prey. Most human envenomations are caused by Anthozoa (anemones and corals), Hydrozoa (Portuguese man-of-war and hydroids), Scyphozoa (the true jellyfish) or Cubozoa (the box jellyfish). Initially, the victim experiences a severe burning pain in skin that comes in contact with the tentacles followed within minutes by a zigzag, whip-like pattern of raised red wheals 2-3 mm wide. Though about 80% of cases are limited to skin manifestations, some have systemic effects including malaise, vomiting, dyspnea and tachycardia.
Rove beetles of family Staphylinidae and genus Paederus contain a vesicant, pederin and produce lesions only when they are crushed on the skin. A wheal forms at the sites followed by a blister within 12-24 h, which may be a linear "whiplash dermatitis." [23]
Other pruritic dermatoses
Many other itchy dermatoses may present with linear marks simulating flagellate dermatitis [Figure - 3]. Dermatographism may produce a flagellate pattern [Figure - 4]. [21] Phytophotodermatitis and poison ivy dermatitis may cause flagellate lesions where the leaves have brushed the cutaneous surface. [21]
 |
| Figure 3: Neurotic excoriations mimicking a flagellate pattern |
 |
| Figure 4: Dermatographism in a flagellate pattern |
Hypereosinophilic syndrome
May et al., have described two men with HIV infection who had unusual cutaneous manifestations of hypereosinophilic syndrome, exfoliative erythroderma and linear flagellate plaques. [24]
Chikungunya fever induced flagellate pigmentation
Chikungunya fever commonly causes hyperpigmentation such as accentuation of melasma, pigmentation of nose, periorbital melanosis and irregular and flagellate patterns on the trunk and extremities. It is primarily considered a post-inflammatory response with the chikungunya virus probably triggering intraepidermal melanin dispersion or retention. [25],[26]
Idiopathic flagellate pigmentation
Pise et al., have reported a case with flagellate pigmentation without any systemic illness, pruritus or drug intake. [27] The flagellate marks did not follow the lines of Blaschko. It appears that rarely, flagellate pigmentation may be idiopathic; though the diagnosis should be one of exclusion.
Conclusion
Flagellate dermatoses are morphologically intriguing diseases produced by different etiological factors. Knowing the various causes of this pattern of skin eruption can help in the diagnosis and management of patients alarmed by this strange-looking eruption.
| 1. |
Flagellation-Wikipedia, the free encyclopedia. Available from: http://www.en.wikipedia.org/wiki/Flagellation. [Last accessed on 2013 Feb 27].
[Google Scholar]
|
| 2. |
Dubowitz H, Finkel MA. Child physical abuse and neglect. In: McInerny TK, Adams HM, editors. AAP Textbook of Pediatric Care (Pediatric Care Online). American Academy of Pediatrics; 2008. Available from: http://www.pediatriccareonline.org/pco/ub/view/AAP-Textbook-of-Pediatric-Care/394120/all/. [Last accessed on 2013 Feb 28].
[Google Scholar]
|
| 3. |
Kennedy CT, Burd DA, Creamer D. Mechanical and thermal injury. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8 th ed. Oxford: Wiley-Blackwell; 2010. p. 28.1-94.
th ed. Oxford: Wiley-Blackwell; 2010. p. 28.1-94.'>[Google Scholar]
|
| 4. |
Vuerstaek JD, Frank J, Poblete-Gutiérrez P. Bleomycin-induced flagellate dermatitis. Int J Dermatol 2007;46 Suppl 3:3-5.
[Google Scholar]
|
| 5. |
Litt JZ. Drug Eruptions and Reactions Manual. 16 th ed. New York: Informa Healthcare; 2010.
[Google Scholar]
|
| 6. |
Abess A, Keel DM, Graham BS. Flagellate hyperpigmentation following intralesional bleomycin treatment of verruca plantaris. Arch Dermatol 2003;139:337-9.
[Google Scholar]
|
| 7. |
Yamamoto T, Nishioka K. Flagellate erythema. Int J Dermatol 2006;45:627-31.
[Google Scholar]
|
| 8. |
Fernandez-Obregon AC, Hogan KP, Bibro MK. Flagellate pigmentation from intrapleural bleomycin. A light microscopy and electron microscopy study. J Am Acad Dermatol 1985;13:464-8.
[Google Scholar]
|
| 9. |
Tallon B, Lamb S. Flagellate erythema induced by docetaxel. Clin Exp Dermatol 2008;33:276-7.
[Google Scholar]
|
| 10. |
Mahmoud BH, Eide MJ. Bendamustine-induced "flagellate dermatitis". Dermatol Online J 2012;18:12.
[Google Scholar]
|
| 11. |
Nousari HC, Ha VT, Laman SD, Provost TT, Tausk FA. "Centripetal flagellate erythema": A cutaneous manifestation associated with dermatomyositis. J Rheumatol 1999;26:692-5.
[Google Scholar]
|
| 12. |
Dupré A, Viraben R, Bonafe JL, Touron P, Lamon P. Zebra-like dermatomyositis. Arch Dermatol 1981;117:63-4.
[Google Scholar]
|
| 13. |
Kimyai-Asadi A, Tausk FA, Nousari HC. A patient with dermatomyositis and linear streaks on the back. Centripetal flagellate erythema associated with dermatomyositis. Arch Dermatol 2000;136:667, 670.
[Google Scholar]
|
| 14. |
Gómez Centeno P, Sánchez-Aguilar D, Pereiro M Jr, Toribio J. Flagellate erythema and dermatomyositis. Clin Exp Dermatol 1998;23:239-40.
[Google Scholar]
|
| 15. |
Suzuki K, Kimura Y, Aoki M, Takezaki S, Tuchida T, Takano T, et al. Persistent plaques and linear pigmentation in adult-onset Still's disease. Dermatology 2001;202:333-5.
[Google Scholar]
|
| 16. |
Fujii K, Konishi K, Kanno Y, Ohgou N. Persistent generalized erythema in adult-onset Still's disease. Int J Dermatol 2003;42:824-5.
[Google Scholar]
|
| 17. |
Soo JK, Pearson IC, Misch KJ. A case of flagellation. Clin Exp Dermatol 2007;32:339-40.
[Google Scholar]
|
| 18. |
Garg S, Cockayne SE. Shiitake dermatitis diagnosed after 16 years! Arch Dermatol 2008;144:1241-2.
[Google Scholar]
|
| 19. |
Haddad Junior V, Silveira FL, Migotto AE. Skin lesions in envenoming by cnidarians (Portuguese man-of-war and jellyfish): Etiology and severity of accidents on the Brazilian coast. Rev Inst Med Trop Sao Paulo 2010;52:47-50.
[Google Scholar]
|
| 20. |
Queiroz Mdo C, Caldas JN. Comparative dermatology: Skin lesion produced by attack of jellyfishes (Physalia physalis). An Bras Dermatol 2011;86:611-2.
[Google Scholar]
|
| 21. |
Jackson SM, Nesbitt LT. The Physical Exam. Differential Diagnosis for the Dermatologist. Verlag: Springer; 2008. p. 109-10.
[Google Scholar]
|
| 22. |
Daly J, Scharf M. Bites and stings of terrestrial and aquatic life. In: Wolff K, Goldsmith L, Katz S, Gilchrest B, Paller A, Leffell D, editors. Fitzpatrick's Dermatology in General Medicine. New York: McGraw-Hill; 2008. p. 2037-53.
[Google Scholar]
|
| 23. |
Burns D. Diseases caused by arthropods and other noxious animals. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. Oxford: Wiley-Blackwell; 2010. p. 38.1-61.
[Google Scholar]
|
| 24. |
May LP, Kelly J, Sanchez M. Hypereosinophilic syndrome with unusual cutaneous manifestations in two men with HIV infection. J Am Acad Dermatol 1990;23:202-4.
[Google Scholar]
|
| 25. |
Kandhari R, Khunger N, Singh A. Flagellate pigmentation and exacerbation of melasma following chikungunya fever: A less frequently reported finding. Indian J Dermatol Venereol Leprol 2012;78:774.
[Google Scholar]
|
| 26. |
Riyaz N, Riyaz A, Rahima, Abdul Latheef EN, Anitha PM, Aravindan KP, et al. Cutaneous manifestations of chikungunya during a recent epidemic in Calicut, north Kerala, south India. Indian J Dermatol Venereol Leprol 2010;76:671-6.
[Google Scholar]
|
| 27. |
Pise GP, Vetrichevvel TP, Thappa DM. Idiopathic flagellate pigmentation. Indian J Dermatol 2007;52:117-8.
[Google Scholar]
|
Fulltext Views
23,999
PDF downloads
4,716





