Translate this page into:
Flagellate pigmentation and exacerbation of melasma following chikungunya fever: A less frequently reported finding
2 V.M. Medical College and Safdarjang Hospital, New Delhi, India
3 National Institute of Pathology, ICMR, Safdarjung Hospital Campus, New Delhi, India
Correspondence Address:
Rajat Kandhari
Department of Dermatology and STD, V.M. Medical College and Safdarjang Hospital, New Delhi
India
| How to cite this article: Kandhari R, Khunger N, Singh A. Flagellate pigmentation and exacerbation of melasma following chikungunya fever: A less frequently reported finding. Indian J Dermatol Venereol Leprol 2012;78:774 |
Sir
Reports have emerged in recent years describing the mucocutaneous manifestations of chikungunya fever. [1],[2],[3],[4] Chikungunya fever is an acute viral infection, characterised by fever,severe arthralgia, and constitutional symptoms. The most commonly encountered skin findings associated with chikungunya fever is a maculopapular rash, which may occur with the onset of the fever, during the course of the fever or after the fever has subsided. The rash usually lasts for a period of 1-7 days. [2],[5] Other mucocutaneous manifestations which may occur include hyperpigmentation, transient nasal erythema, generalized erythema, tenderness and edema of the hands and feet, multiple apthous-like ulcers, vesiculobullous lesions, purpuric or hemorrhagic lesions and vasculitic lesions. [1],[2],[3],[4],[6] Chikungunya fever may also be associated with exacerbation of certain pre-existing dermatosis such as psoriasis [1],[3],[7] and lichen planus [3] to name a few.
We report a case of a 35 year old, female patient with streaks of hyperpigmentation on the trunk and the extremities. On questioning, the patient revealed that the brownish coloured lesions appeared in association with a fever, which had occurred three weeks back. The fever was associated with severe joint pains, persistent in nature; fatigue and dryness of the skin. There was accentuation of the pre existing brownish discoloration on either side of her face, which occurred on subsidence of the fever. She also revealed the occurrence of blackish, lesions on the palms. Tests for malaria, dengue fever and typhoid were negative. Viral culture and isolation were not performed. A probable diagnosis of chikungunya fever was made on clinical grounds and exclusion of other possible causes of fever with joint pains. On examination, we found asymptomatic, centrofacial, brownish-black discoloration, which was predominant on the nose and the upper lip. Bilateral malar region showed a reticulate pattern of pigmentation, which was present for two years prior to the fever, but had exacerbated once the fever subsided. The upper extremities and the back, showed an irregular, flagellate or "whip-lash" pattern of brownish pigmentation. There was speckled, discrete, freckle-like pigmentation seen on the palmar aspect of both hands, along with blackish macules on the fingers. Generalised xerosis and scaling were noted all over the body [Figure - 1]a-d. Two skin biopsies were performed, one from the right side of the back and the other from the nose. The biopsy from the back showed increased intraepidermal melanin in the basal and suprabasal keratinocytes [Figure - 2], whereas the biopsy from the nose demonstrated superficial and deep melanophages in the dermis with less prominent epidermal pigmentation along with extensive solar elastosis, suggestive of melasma.
 |
| Figure 1: (a) speckled, discrete, freckle-like pigmentation on the palmar aspect of the hand along with blackish macules on the fingers, (b) brownish-black discoloration on the nose and the upper lip along reticulate pattern of pigmentation on bilateral malar region, (c) upper extremity showing brownish, with xerosis and scaling, (d) flagellate or "whip-lash" pattern of pigmentation on the trunk |
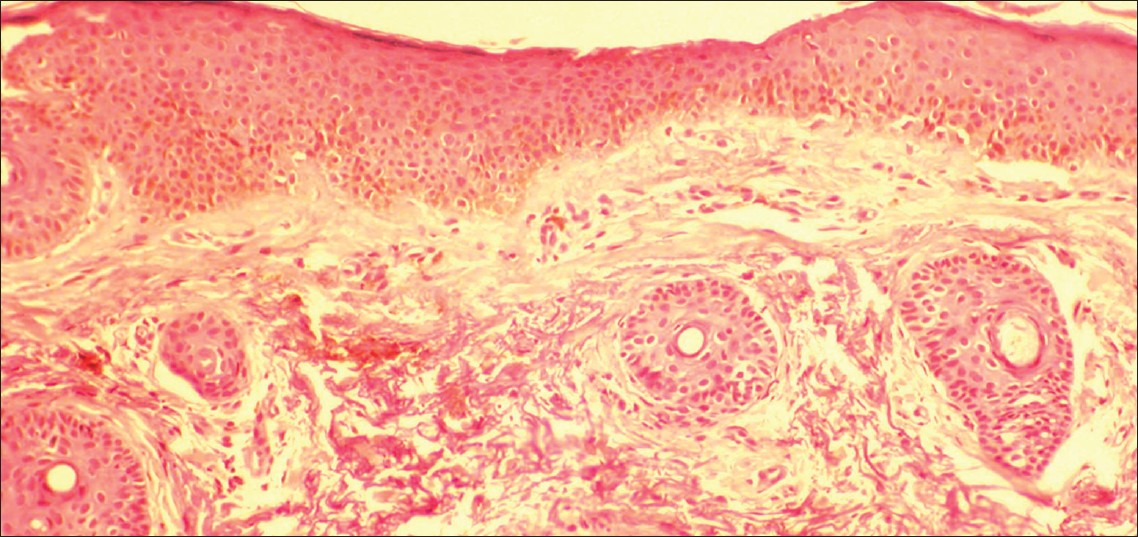 |
| Figure 2: Increased intraepidermal melanin in the basal and suprabasal keratinocytes (H and E, ×100) |
In a study done by Inamdar et al. [1] in 145 "suspected cases" of chikungunya fever, hyperpigmentation was reported as the most common finding. They reported flagellate pigmentation in two cases and accentuation of melasma in one case. Riyaz et al. [4] in their study of 162 patients of chikungunya fever, reported flagellate pigmentation and exacerbation of pre existing psoriasis, lichen planus and unmasking of Hansens disease with type 1 reaction. They, however, did not mention the number of cases having the flagellate pattern of pigmentation. Prashant et al[3] reported flare up of pre existing dermatosis in ten patients out of their group of 115, wherein six patients had a flare up of psoriasis and four patients experienced a flare up of lichen planus. They however did not report any patient with flagellate pigmentation. In another study [7] of 75 suspect cases of chikungunya fever, exacerbation of pre existing dermatological disease was noted in 4 patients, of whom two had psoriasis and one each had eczema and erythroderma. The exact cause of the hypermelanosis following chikungunya fever remains a mystery, although it is primarily considered a post inflammatory response. It is proposed that the chikungunya virus may be triggering the intraepidermal melanin dispersion or retention. [1] The presence of melanophages seen on histology may be considered a cause for the persistence of the pigmentation. [4]
| 1. |
Inamadar AC, Palit A, Sampagavi VV, Raghunath S, Deshmukh NS. Cutaneous manifestations of chikungunya fever: Observations made during a recent outbreak in south India. Int J Dermatol 2008;47:154-9.
[Google Scholar]
|
| 2. |
Bandyopadhyay D, Ghosh SK. Mucocutaneous features of Chikungunya fever: A study from an outbreak in West Bengal, India. Int J Dermatol 2008;47:1148-52.
[Google Scholar]
|
| 3. |
Prashant S, Kumar AS, Basheeruddin DD, Chowdhary TN, Madhu B. Cutaneous manifestations in patients suspected of Chikungunya disease. Indian J Dermatol 2009;54:128-31.
[Google Scholar]
|
| 4. |
Riyaz N, Riyaz A, Rahima, Abdul Latheef EN, Anitha PM, Aravindan KP, et al. Cutaneous manifestations of chikungunya during a recent epidemic in Calicut, north Kerala, south India. Indian J Dermatol Venereol Leprol 2010;76:671-6.
[Google Scholar]
|
| 5. |
Johnston RE, Peters CJ: Alphaviruses. In: Fields BN, Knipe DM, Howley PM, Chanock RM, Melnick JL, Monath TP, Roisman B, Straus SE editors. Fields Virology Volume 1, 3 rd ed. Philadelphia: Lippincott-Raven; 1996.p. 843-98.
[Google Scholar]
|
| 6. |
Pakran J, George M, Riyaz N, Arakkal R, George S, Rajan U, et al. Purpuric macules with vesiculobullous lesions: A novel manifestation of Chikungunya. Int J Dermatol 2011;50:61-9.
[Google Scholar]
|
| 7. |
Bhat RM, Rai Y, Ramesh A, Nandakishore B, Sukumar D, Martis J, et al. Mucocutaneous manifestations of chikungunya fever: A study from an epidemic in coastal Karnataka. Indian J Dermatol 2011;56:290-4.
[Google Scholar]
|
Fulltext Views
1,876
PDF downloads
1,372





